RABIES - heartha..
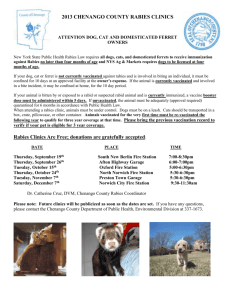
advertisement

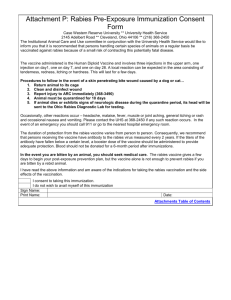
RABIES (Hydrophobia, Lyssa) Rabies is a viral zoonotic neuroinvasive disease that causes acute encephalitis in mammals. It is generally characterized by CNS irritation, paralysis, and death. Animals causing rabies can be classified into two. Canine rabies is caused by domestic animals while sylvatic rabies is caused by wild animals. Once symptoms of the disease develop, rabies is fatal. In the Philippines, around 300 to 600 Filipinos die every year. History-Cultural impact Because of its potentially violent nature, rabies has been known since 3000 B.C. The term "rabies" is possibly derived from the Sanskrit word "rabhas" or "to do violence". The Greeks derived the word "lyssa" meaning "lud" or "violent", this terminology is used in the name of the genus of rabies lyssavirus. In the 19th century rabies has been considered a scourge for its prevalence. Louis Pasteur was then able to test post-exposure treatments in 1895. It was not until 1960 when the virus itself was isolated. Epidemiology Etiology The virus that causes rabies is a rhabdovirus of the genus Lyssavirus. Incubation Period From 2 to 8 weeks up to a year depending on the following: • Site of the wound • Severity of the wound • Amount of virus introduced • Protection provided by clothing Pathophysiology Rhabdovirus Penetration to tissue Travels along peripheral nerves CNS Body tissue Clinical Manifestations Rabies is a highly neurotropic virus that evades immune surveillance by its sequestration in the nervous system. Upon inoculation, it enters the peripheral nerves. A prolonged incubation follows, the length of which depends on the size of the inoculum and its proximity to the CNS. Amplification occurs until bare nucleocapsids spill into the myoneural junction and enter motor and sensory axons. At this point, prophylactic therapy becomes futile, and rabies can be expected to follow its fatal course, with a mortality rate of 100%. The rabies virus travels along these axons to enter the spinal ganglion. Its multiplication in the ganglion is heralded by the onset of pain or paresthesia at the site of the inoculum, which is the first clinical symptom and a hallmark finding. From here, the rabies virus spreads quickly into the CNS, and spread is marked by rapidly progressive encephalitis. Thereafter, the virus spreads to the periphery and salivary glands. Signs and Symptoms I. Incubation period o The rabies virus transfers from peripheral areas to the CNS. o The infected individual remain asymptomatic. o The average duration of incubation is 20-90 days. o The rabies virus is segregated from the immune system during this period, and no antibody response is observed. II. Prodromal period o The virus enters the CNS. o The duration of this period is 2-10 days. o Paresthesia or pain at the inoculation site and hydrophobia are pathognomonic for rabies and occurs in 50% of cases during this phase. o Symptoms may include malaise, anorexia, headaches, fever, chills, pharyngitis, nausea, emesis, diarrhea, anxiety, agitation, insomnia, and depression. III.Acute neurologic period o This period is associated with objective signs of developing CNS disease. o The duration is 2-7 days. o Furious rabies may develop in this period. Patients develop agitation, hyperactivity, restlessness, thrashing, biting, confusion, or hallucinations. Episodes may be triggered by visual, auditory, or tactile stimuli or may be spontaneous. Seizures may occur. This phase may end in cardiorespiratory arrest or may progress to paralysis. o Paralytic rabies is also known as dumb rabies or apathetic rabies because the patient is relatively quiet compared with a person with the furious form. IV. Coma o This begins within 10 days of onset; the duration varies. o Without intensive supportive care, respiratory depression, arrest, and death occur shortly after coma. Diagnosis Observations of the presenting clinical manifestation and providing a history taking generally provides the basis for diagnosing rabies. However, for clarification purposes, Fluorescent Antibody Technique is used to demonstrate the Rabies viral antigens in infected cells that is usually done ante mortem by obtaining sample from the CSF. o Negri Bodies Negri bodies ae cytoplasmatic inclusion bodies found in the purkinje cells of the brain in cases of rabies. Negri's bodies are important because their presence make possible a positive diagnosis of rabies. Dr. Adelchi Negri reported the identification of what he believed to be the etiologic agent of rabies, the Negri body. In his report, he described Negri bodies as round or oval inclusions within the cytoplasm of nerve cells of animals infected with rabies. Treatment Treatment of humans consists of thorough flushing and cleansing of the bite wound with soap and water to be followed by introduction of vaccines. o Post-exposure treatment Post-exposure treatment is given to persons who are exposed to rabid animals. It consists of local wound treatment, active immunization (vaccination) and passive immunization (administration of rabies immunoglobin). o Active and passive immunization Active immunization or vaccination aims to induce the body to develop antibodies against Rabies whose effect lasts for 1 to 3 years. Passive immunization is the process of giving an antibody to persons with Category III exposure (head and neck bites, multiple/single deep bites, contamination of mucous membranes, licks of the eyes, lips and mouth) in order to provide immediate protection against Rabies, which should be administered within the first seven days of active immunization. The effect of the immunoglobulin is only short term. o Immunization schedule Grade of exposure I Type of exposure Contact with a rabid suspected rabid animal Immunization schedule or Contact with an inoculated animal Touching/feeding animal, Touching but no contact with saliva; inoculated lure, and skin undamaged prior to skin intact and during contact No immunization necessary If uncertainty exists than schedule B is to be followed. II a) Animal has nibbled or licked exposed skin. b) Contact with saliva c) Superficial, non- bleeding scratches made by the animal Touching inoculated lure, skin damaged. Immediate immunization according to schedule B. In case of uncertainty concomitant prophylaxis as specified in schedule C. If animal is examined & found to be non-rabid then continue as in schedule A III a) All bites b) Bleeding scratches c) All scratches on the head, neck, scapular region, arm & hands d) Contact of animal saliva with mucous membrane of patient Contact of inoculated lure with mucous membrane or fresh skin wound Immediate concomitant prophylaxis per schedule C. If animal is proved non-rabid it is adjustable to continue treatment as in schedule A. Schedule A Schedule B Schedule C Prophylactic immunization prior to exposure. Immunization after exposure. Concomitant prophylaxis after exposure. Rabipur® as in schedule B + 1 X 20 I.V./kg body wt. One injection IM on days One injection IM on human rabies immunoglobulin concomitantly with 0,3,7,14,30 & if days 0,7,28 and 365 injection of Rabipur or on day 7 after the first injection necessary on day 90. of Rabipur® at the latest. Nursing Responsibilities • Wound cleaning • Medication- antibiotic, anti-tetanus • Control circulatory and CNS damage • Patient isolation/transmission Prevention Education Animal Control Vaccination Proper surveillance National Rabies Prevention & Control Program Goal: Human Rabies is eliminated in the Phil. And the country is declared rabies-free Objectives: a. Human Rabies: reduce incidence from 7/mil to 1/mil by 2010 & eliminate by 2015 b. Canine Rabies: reduce from 70/100,000 to 7/100,000 by 2010 & eliminate by 2015 Key facts Rabies is widely distributed across the globe. More than 55 000 people die of rabies each year. About 95% of human deaths occur in Asia and Africa. Most human deaths follow a bite from an infected dog. Between 30% and 60% of the victims of dog bites are children under the age of 15. Wound cleansing and immunizations, done as soon as possible after suspect contact with an animal and following WHO recommendations, can prevent the onset of rabies in virtually 100% of exposures. Once the signs and symptoms of rabies start to appear, there is no treatment and the disease is almost always fatal. Globally, the most cost-effective strategy for preventing rabies in people is by eliminating rabies in dogs through animal vaccinations. March is Rabies Awareness Month and September 28 is World Rabies Day! JORA MARJORIE M. DIMAYUGA