Attracting and Retaining Individuals in Academic Pulmonary, Critical
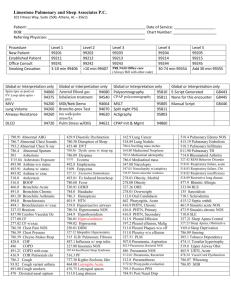
advertisement

Appendix II Summaries of three relevant, recent workshops sponsored by the American Thoracic Society which discuss issues similar to those in the NHLBI Training Workshop were presented on behalf of the ATS by Dr. Augustine Choi. The ATS Executive Committee established a Task Force in Scientific and Clinical Careers in the summer of 2008. The charge of this task force was to analyze the key attractions and barriers to entry and maintenance of clinical and scientific careers in pulmonary, critical care and sleep medicine. The major objectives of the task force was the following: The Task Force should present specific recommendations to increase attractiveness of these careers for trainees at multiple levels and for professionals in mid-career. The Task Force should identify specific positive elements of these careers that could be utilized for greater awareness and increasing entry into the career pipeline. The Task Force also should make recommendations about whether and how to interact with other sister organizations with similar goals in this area. Within the goals of the Task Force is the identification of specific steps that can be initiated within the next one to two years to increase attractiveness of these career pathways. Additional specific questions include: How can we increase the “pipeline” of undergraduate, medical and graduate students interested in clinical and research careers related to pulmonary, critical care and sleep medicine? How can we develop a network of “best practice” teaching materials to improve the quality of student teaching and thereby try to attract more students? Is there a role for ATS developing a method of recognizing a cadre of master teachers and/or mentors? The Appendix* includes the summary of the recommendations of the ATS Task Force in Scientific and Clinical Careers which was sent to the ATS Executive Committee in December of 2008. * personal communication approved by the ATS Executive Committee 1 “Attracting and Retaining Individuals in Academic Pulmonary, Critical Care and Sleep Medicine” The Academic Career Subcommittee members participated in 2 conference calls and multiple electronic communications with these interactions designed to analyze key attractions and barriers to entry and maintenance of clinical and scientific careers in pulmonary, critical care and sleep medicine. While addressing a broad spectrum of career opportunities in academic Pulmonary/Critical Care Medicine/Sleep Medicine (Pulm/CCM/Sleep), the Academic Career Subcommittee was deeply concerned about the shrinking and aging physician-scientist/clinical-investigator workforce, and the acute need to recruit and retain young physician-scientists in the field of Pulm/CCM/Sleep. A formal SWOT Analysis (Strengths, Weaknesses, Opportunities and Threats) was undertaken by each committee member who also reviewed drafts of Task Force survey questions and submitted additional questions for consideration. This document represents the summary of the formal SWOT analyses as well as the specific recommendations generated to increase attractiveness of academic Pulm/CCM/Sleep careers targeting trainees at multiple levels and professionals in mid-career. General Strengths of a Career in Academic Medicine Scientific careers in academic medicine are exciting, intellectually stimulating, enjoyable and satisfying Many career pathways exist in academic medicine including clinical educator and physician scientist pathways An academic career permits an attractive balance between patient care, teaching, and research as well as intellectual independence and flexibility Academic medicine is more stimulating than private sector clinical medicine and offers greater variety and geographic mobility Academic medicine is a noble calling, particularly in the training of future leaders of academic medicine Specific Strengths of an Academic Career in Pulmonary / Critical Care /Sleep Medicine Pulm/CCM/Sleep provides a procedure-rich specialty with intensive care opportunities that are attractive to many young physicians. Academic Pulm/CCM/Sleep medicine offers greater flexibility than private sector clinical medicine in terms of daily scheduling, meeting family obligations, and lifestyle Many excellent role models exist in academic Pulm/CCM/Sleep The Lung Division of NHLBI is proactive in attracting young trainees and junior faculty 2 A number of Chairs of Departments of Medicine in prestigious academic medical centers are Pulm/CCM/Sleep physicians Divisions of Pulm/CCM/Sleep, as well as their training programs, are highly regarded in major medical centers Weaknesses in Choosing an Academic Pulmonary/Critical Care/Sleep Medicine Career Many medical school graduates and residents seek medical careers that do not require a 100-hour work week as Pulm/CCM portends.. Current perception is of high stress, long work hours in ICU environment, possibly with required nighttime or in-house call coverage Inadequate number of positive role models in academic Pulm/CCM/Sleep medicine Residents and fellows have poor understanding of diverse academic career paths Difficult to predict which individual trainees are likely to gravitate towards an academic career making it difficult for training programs to focus limited resources on the most promising candidates Disparity in academic Pulm/CCM/Sleep medicine incomes versus private practice Limitations in exposing medical students to pulmonary & sleep biology pathobiology Lengthy period of research training to become an independent investigator combined with much lower salaries Extended duration of ACGME-mandated clinical activities which reduce research experience Physician-scientists are often unable to “get away from their work” meaning that we constantly think about our work and new research ideas. Also, the race for funding never ends so there is no time for a “break.” Little or no opportunities for part time work since this is not allowed by NIH Excessive clinical demands on junior faculty especially physician scientists Opportunities for Increasing Interest in Academic Pulm/Crit Care/Sleep Medicine Careers Dispel myths about academic medicine careers: salary structures, lifestyle Pulm/CCM/Sleep is a rapidly evolving, evidence-based specialty with many opportunities for basic and clinical research Expanded recent efforts at NIH which focus on awards for early career trainees, first-time RO1 recipients, and on programs to facilitate debt reduction Junior faculty could benefit from formal education focusing on career development and research (grant writing, for example), whereas fellows could benefit from more formal education about transitioning careers to faculty status Increase opportunities (summer and year round) to expose college students, med students and house staff to Pulm/CCM/Sleep research 3 Strengthen involvement of Pulm/CCM/Sleep physician-scientists in coursework in med schools Provide a culture of academic medicine where part-time work would be possible for people with young families, combined with a substantial campaign to convince students and residents that academics is flexible and “friendly” Research (mostly clinical research) is moving into community hospitals creating. an opportunity for more physician-scientists in locations other than large cities. Threats to Attracting and Retaining Individuals in Academic Pulmonary, Critical Care and Sleep Medicine Declining number of individuals entering pulmonary for the past 5 to 10 years The supply of physician-scientists/clinician-investigators in academic medicine is declining: debt load, prolonged duration of training, research funding woes Competing specialties in critical care (surgery and anesthesia) and sleep (neurology) Difficulty and uncertainty of securing meaningful extramural grant funding Perception of limited job security related to continue grant funding Excessive duration of training and time to achieve independent funding Increased value in work-life balance and controllable life-styles in the selection of a career pathway 85% of medical students carry debt of at least $100,000 at the time of graduation Clinical demands in academic centers are already heavy and potentially will increase if 24/7 attending coverage in ICUs is required The attraction for Pulm/CCM/Sleep training for many residents continues to be the ICU and procedures An aging population will require more Pulm/CCM/Sleep specialists for community clinical work, not for research Severely impaired NIH funding is greatly exacerbating the shortage of physicianscientists, unlikely to be remedied without substantial increases in funding Perception that being a physician-scientist means forever being on a treadmill Women find physician scientist careers less attractive than men Pulmonary is being dropped as a critical component of critical care training in some programs Summary of Recommended Actions: ATS should join other societies such as Association of Professors of Medicine, AAP, ASCI etc in nurturing the pipeline for physician scientist careers ATS should formalize an academic mentoring program for fellows and junior faculty with academic leaders 4 ATS should continue to advocate for additional mechanisms of salary support for promising academic oriented transitioning fellows with mandated protected time and for debt reduction grants for junior faculty ATS should convene PIs of pulmonary training grants to strategize on best practices in recruitment and retention of academic fellows ATS should continue to identify major concerns of residents, fellows, and junior faculty for pursuing careers in academic medicine ATS should develop recommendations for the comprehensive mentoring of fellows and junior faculty pursuing careers in academic medicine focusing particularly on challenges presented by specialization in Pulm/ CCM/ Sleep. Include website information with links for both mentors and mentees ATS should disseminate detailed financial data (salary) for faculty during their first few years of academic practice to help dispel myths of dramatic salary differential between academic and private practice in the first several years postfellowship ATS should collect and disseminate accurate data related to career success and retention rates for academic Pulm/CCM/Sleep faculty that may offset pessimistic attitudes about academic career viability Increase exposure of medical students to strong Pulm/CCM/Sleep role models ATS should fund a prospective assessment of trainee characteristics that predict future success in academic Pulm/CCM/Sleep and assist academic training programs and divisions in recruitment, selection, and training of the most promising candidates for successful careers in academic Pulm/CCM/Sleep. References 1. Revitalizing the Nations Physicians Scientist Workforce. Association of Professors of Medicine, Report of the Physician Scientist Taskforce. Monograph pgs 1-45. 2. Academic and Career Development of Pulmonary and Critical Care PhysicianScientists. Am J Respir Crit Care Med 173: 23–31, 2006. 3. Attitudes & Perceptions of Internal Medicine Residents Regarding Pulmonary and Critical Care Subspecialty Training,” CHEST 2005, 127; 630-636. 4. Pulmonary and Critical Care: The Unattractive Specialty,” CHEST 2005, 127; 1085-1087 ATS Scientific and Clinical Careers in Pulmonary, Critical Care and Sleep Task Force Sister Societies and Other Organizations Subcommittee 5 Charge: How can the ATS work with sister societies to improve the attractiveness and eliminate some of the barriers to careers in pulmonary, critical care and sleep? SWOT Analysis: Strengths: 1. Each of the major sister organizations including the American Thoracic Society (ATS), the American College of Chest Physicians (ACCP), the Association of Pulmonary and Critical Care Program Directors (APCCCMPD) and the Society for Critical Care Medicine (SCCM) are strongly committed to increasing the pool and numbers of individuals entering clinical, academic, and public health careers in pulmonary, critical care and sleep, and related disciplines. 2. The larger organizations have complementary strengths, with the ATS most vocally supporting academic and research careers, while the focus of ACCP and SCCM remains largely centered on clinical career. The APCCMPD is principally focused on training. 3. Most of our members (including leadership) are members in at least two of these organizations. Therefore, cross talk should be easily facilitated. The APCCMPD group is independent and convenes both in association with the international meetings of the ATS and the ACCP. 4. Workforce analysis continues to support expansion of the numbers of individuals needed for Pulmonary, Critical Care, and Sleep Career, meaning that the career outlooks for those who select to train in our specialties looks to remain extremely favorable for the foreseeable future. Weaknesses: 1. Traditionally some competition has been perceived in attracting fellow members to one or another of these sister societies. This perception has perhaps limited concerted efforts to increased recruitment of members in training to the general area of pulmonary, critical care, sleep and related disciplines. 2. While these sister societies have focused on increasing the participation of subspecialty fellows at their international meeting, relatively little effort has been centered on attracting internal medicine residents, and undergraduate science students to attend these meetings. These individuals have not yet made career selections. 3. Healthcare reimbursement for Pulmonary and Critical Care is currently not as attractive as other subspecialties, such as cardiovascular medicine, gastroenterology, and oncology. This is not the situation for sleep medicine, which for the near future may serve as a mitigating factor. 6 4. Work-life balance is increasingly perceived as unfavorable for career selection in pulmonary and critical care medicine. This limits recruitment in general, but may also significantly negatively impact the recruitment of female candidates into clinical careers within these disciplines, particularly critical care. 5. The pool of US students entering science and technical related careers continues to decline. However, internationally trained individuals in these disciplines remain plentiful. Opportunities: 1. Considerable opportunities exist to reach out to both undergraduate students and PhD students and internal medicine residents early in their training, before final career selection has been made. Particular interest might be focused on MD/PHD students interested in academic careers. 2. Sleep medicine currently enjoys attractive reimbursement, and in a mixed specialty career, can mitigate several of the factors listed above (reimbursement and work-life balance). 3. Numerous internationally trained individuals have interest in pulmonary, critical care and sleep, and related disciplines, but are hampered in completion of training due to regulatory and legislative issues (e.g. Visa and NIH training grant issues). 4. Both the ATS have excellent support services for approaching and communicating with governmental bodies and agencies about these concerns. Further, these sister societies have a significant history of working together on key regulatory issues. Threats: 1. Projected worsening of medical economics and health care reimbursements threatens to reduce interest in clinical careers. Considerable concerns exist about reduced reimbursements for ICU related diagnoses as well as changing reimbursement for pulmonary and sleep diagnostic procedural reimbursements. 2. Uncertainty that reduced funding for basic and clinical research at the Federal level and for public health initiatives might occur threatens to reduce interest in research and academic careers in pulmonary, critical care and sleep, and related disciplines. 3. Increased focus of the next generation of trainers on appropriate work-life balance may further threaten our already overtaxed specialty areas. Suggested Solutions: 7 1. Greater communication and concerted efforts between these sister societies and other organization will be needed to increase the numbers of individuals seeking careers in pulmonary, critical care, sleep, and related disciplines. 2. Consideration may be given for either a summit meeting or a joint conference call series involving representatives of the sister societies and organizations to improve the attractiveness and eliminate some of the barriers to careers in pulmonary, critical care and sleep and related areas, as listed below. 3. Concerted efforts must be undertaken to increase participation of undergraduate science students, MA and PhD students, and undifferentiated internal medicine residents, as well as international trainees within each of the key societies and organizations. Suggested mechanisms can include expanded travel awards and committee memberships specifically for these types of trainees to participate at these meetings. In addition, we may want to focus some specific effort on MD/PhD students or MD/MPH students seeking academic careers. 4. Consideration should be given for outreach activities of domestic and international trainees at the undergraduate or internal medicine level beyond participating at the international meetings of these societies. For instance, the societies might consider expanding grants or even joint funding opportunities specifically to facilitate the lab research or training of such individuals, who have to yet select a career area. 5. The societies need to continue to jointly lobby governmental and regulatory organization to support increased training slots for pulmonary, critical care, sleep, and related disciplines. 6. Investigate and support studies of new clinical staffing models that improve worklife balance. 7. Increase communication and joint efforts of the sister societies to voice concerns about Medicare reform and reimbursement changes so that reduced clinical revenue does not further compromise recruitment of trainees into pulmonary, critical care, sleep, and related disciplines. 8. Enhanced joint efforts of the sister societies to communicate and work for stable governmental funding both for training and research in areas related to pulmonary, critical care, sleep, and related disciplines. 9. Increased joint effort of the sister societies to communicate and petition for governmental and legislative reform bringing relief for international trainees (e.g. enhanced opportunities for NIH training grant participation, more flexible visa rules). This would significantly foster greater influx of learners into pulmonary, critical care, and sleep medicine and related research areas. 8 Pulmonary and Critical Care ATS Task Force on Career Attractiveness S.W.O.T. analysis Process: Committee members and local Pulmonary/Critical Care Medicine (PCCM) faculty and fellows were contacted in person and by email and asked to describe what they found attractive or unattractive about a career in PCCM. In addition, small unstructured focus group meetings were held with internal medicine residents who had recently decided on 9 subspecialty fellowship. Comments were organized into S.W.O.T. format and circulated to committee members for comment and revision. We focused on issues related to house staff choice of a career in PCCM, rather than Fellows’ choice of academic careers or career retention of practicing PCCM specialists and scientists. Review of data over the past 5 years from the NRMP does not indicate dwindling interest in PCCM. On the contrary, the number of fellowship programs, slots, and applicants have all increased and the ratio of applicants to positions has remained stable. We considered the goal of this exercise to maintain the health of a vigorous field of Medicine, rather than respond to a demographic crisis. Strengths 1. High acuity, high stakes, high adrenaline medicine. 2. Applied physiology prominent feature of diagnosis and management a. Appeals to the mechanically inclined. b. Bridges basic and clinical science c. Ideal teaching material for clinician-educators 3. Wide range of practice settings a. Ambulatory care b. Critical Care c. Sleep medicine 4. Wide range of patient care opportunities a. Occupational medicine b. Short-term consultation c. Long-term chronic care d. Palliative care e. Acute crisis intervention 5. Wide range of potential lifestyles which can evolve over time a. Fully in-patient b. Critical Care c. Ambulatory Care d. Sleep 6. Procedure-oriented practice, if desired, with expanding procedural options. 7. Opportunities for public health and political advocacy a. Tobacco b. Air pollution. c. Industrial medicine d. Global health e. Disaster management 8. Some diseases, for example PAH, CF and ARDS, have had major breakthroughs and improvements in outcomes in recent years. 9. Multi-system disease management a. Critical Care crosses silos: The General Internist for the really sick 10 b. Many pulmonary diseases are multi-system (PAH, neuromuscular diseases, rheumatologic illnesses, cancer) 10. End-of-life care a. Opportunities for rewarding relationships with patients and families b. Opportunities to improve neglected area of medical care Weaknesses 1. Many common PCCM diseases have little public awareness (COPD, ARDS) or bearing the stigma of self-induced illness (emphysema). 2. Common chronic illnesses have intractable symptoms and little new therapy (COPD). 3. House staff typically encounter outpatient treatment “failures” whose treatment appears formulaic: a. Refractory COPD and asthma b. Continued smokers c. Medical non-adherence d. Progressive CF patients e. Lung transplant failures 4. Almost all patients suffer dyspnea, a miserable symptom with no treatment. 5. Compensation and work hours (or at least their ratio) may not be on a par with “competing” subspecialties such as Cardiology and GI. 6. Critical care practice can lead to mid-career burnout. 7. General sense that much of ICU care is wasted on patients unlikely to benefit. 8. Perceived by house staff as not having a particularly family-friendly lifestyle, and few female role models. Opportunities 1. Increasing public awareness and attention is being paid to asthma and COPD. 2. Staffing shortages in Critical Care will persist for the foreseeable future. 3. Increasing emphasis is being placed on multidisciplinary care, protocols, and patient safety, for which ICUs have been the advance guard. 4. Epidemic of sleep-disordered breathing is occurring as a complication of obesity. 5. House staff exposure to successful outpatient management of pulmonary disease can be improved. 6. House staff teaching on pulmonary services can be improved a. Some programs excel in MICU, others on in-patient services b. Few excel at teaching outpatient management and continuity c. Commitment to teaching cited by many house staff as strong positive when present d. Role modeling and teaching of long-term doctor-patient relationships and management can be strengthened in many programs Threats 11 1. Reimbursement always under stress; several of CMS proposed “never events” are common and probably cannot be completely eliminated in ICU patients. 2. Society of Critical Care Medicine (SCCM) is positioning itself as the critical care society and multiple non-PCCM pathways into critical care exist. 3. One-year sleep fellowship may divert many applicants away from Pulmonary or PCCM. 4. Demands for 24-hour attending staffing of ICUs may make lifestyle less attractive. 5. Hospitalist movement has created opportunities to practice critical care in many hospitals without the need for additional fellowship training. 6. Duty hour restrictions on house staff have increased service demands on PCCM fellows in some programs, especially for ICU coverage. Disgruntled Fellows are one of the most effective deterrents for interested house staff. Recommendations 1. An enthusiastic commitment to house staff education was routinely cited as a feature that attracts house staff to a subspecialty. Application of this will necessarily vary by local institutional resources. However, the following should be considered: a. Careful weighing of educational versus service requirements for house staff on pulmonary or ICU rotations. b. Formal curriculum development as a vehicle to focus faculty on educational issues and methods. c. Self-conscious role modeling by clinicians. d. Efforts to recognize and reward teaching excellence at the Divisional and Departmental levels. e. Incorporating regular didactic sessions into medical ICU or pulmonary rotations. 2. Broaden house staff exposure to the wide range of practice, scientific, and lifestyle opportunities within the field. a. Incorporate exposure to successful outpatient management and longitudinal care into house staff training. b. Provide opportunities for house staff participation in research or advocacy activities. c. If funding is available, sponsor house staff attendance at national or regional specialty society meetings. 12