Laboratory Exercise 10: Physiology of Ventilation (Breathing)

Laboratory Exercise 10: Physiology of Ventilation (Breathing)
To get air into and out of the alveoli (ventilation) is accomplished by the action of the diaphragm and intercostals muscles. These muscles are under the automatic control of the respiratory centers in the medulla oblongata and pons.
The respiratory centers are controlled by the amount of CO
2
and H
+
ions in the blood and cerebrospinal fluid. When CO
2 and H
+
ions levels change they will change the rate and depth of breathing.
A. Volume Changes with Ventilation
1. Thoracic (Chest) Cavity Volume Changes during Breathing – Correlation of volume changes of
the chest cavity during inspiration and expiration on changing depth of breathing.
The lungs do not possess an inherent pumping mechanism to exchange air with the atmosphere.
The pumping mechanism is assumed by the diaphragm and intercostals muscles.
When the breathing muscles contract, the dimensions of the thoracic cavity enlarge, this causes
the intrathoracic pressure drops, to lower the pressure in the lungs and airways below atmospheric.
The result is inspiration, movement of atmospheric air into the respiratory passageways.
When the breathing control centers in the medulla and pons signal an end to the inspiration,
breathing muscles relax, the thoracic cage recoils, pressure gradients are reversed. The greater
intrathoracic pressure causes air to be expired. A breathing cycle (one breath) includes
inspiration and expiration. A normal breathing rate at rest for an adult is 12-18 breaths/minute.
This called eupnea or eupneic breathing (eu-true breathing).
Axillary measurements reflect chest expansion caused by intercostals muscle contraction.
Xiphoid measurements reflect lower thoracic region expansion when the diaphragm contracts.
2. Pulmonary (Lung) Volume Changes During Breathing - Correlation of inspiration and expiration
with lung volume changes on changing depth of breathing.
Measurements of Static Lung Volume
During eupneic breathing, when the body is not being stressed, about 500 mL of air moves into and
out of air passageways of the breathing system during inspiration and expiration. The volume of air
inspired or expired is the tidal volume. Only about 350 mL of tidal volume reaches the alveoli, the
other 150 mL, “dead air”, remains in the spaces of the conducting pathway, nose, pharynx, larynx,
trachea and bronchi. Tidal breathing suffices in a resting state, pulmonary reserves are essential if
breathing is to keep pace with more strenuous physical activity.
1
In the laboratory, a wet spirometer is used to measure exhaled tidal and reserve volumes.
Tidal volume –the amount of air inhaled and exhaled during quiet (eupneic) breathing,
normal volume – 500mL.
Expiratory Reserve volume – the volume of air that can be forcibly expired after tidal air has been
expelled, normal volume - 1100 mL.
Expiratory Reserve Vol. = Total Expiratory Capacity -Tidal Vol.
(ERV) (TV)
1600 - 500 = 1100 mL
Inspiratory Reserve volume - the volume of air that can be forcibly inhaled after tidal air has been
inhaled, normal volume 3000mL.
Inspiratory Reserve Vol. = Total Inspiratory Capacity -Tidal Vol.
(IRV) (TV)
3600 - 500 = 3100 mL
Inspiratory reserve volume cannot be measured directly by spirometry, but may be calculated.
IRV = Vital Capacity (VC) – TV- ERV.
4600 - 500 – 1100 = 3000 mL
Vital Capacity (VC) – the total exchangeable air in the lungs. It is the sum of tidal and reserve
volumes. It is a measure of a person’s physical fitness. To record vital capacity inhale maximally
and exhale as forcibly as possible until exhalation is complete, normal volume - 4600 mL.
Residual volume (RV) – volume of air remaining in the lungs after a maximal exhalation, normal
volume - 1000 mL.
Functional Residual Capacity = ERV + RV
1100 + 1000 = 2100 mL
Total Lung Capacity (TLC) = IRV + TV + ERV + RV
5600 mL = 3000 500 1100 1000
VC
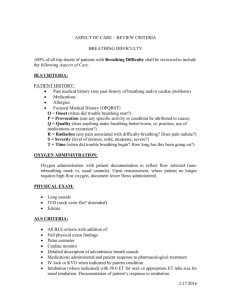
Dynamic Measure of Air Flow from the Lungs – Forced Expiratory Volume
Vital capacity is used to diagnose lung disease, but obstructive diseases such as asthma and emphysema may give a normal vital capacity value. A test used in conjunction with vital capacity reveals exhaled volume and how rapidly the air is expelled. The forced expiratory volume (FEV t
) is the volume of air expelled forcibly / 1 second. This test gives an indication of rate of air outflow through the respiratory passageways. The value is expressed as FEV
1
as the volume air expelled over a second of time. The FEV
1
/VC ratio is 0.75-0.80 is considered normal. This means a healthy person exhales about 80% of the vital capacity in 1 second. If there is obstruction in the airways the FEV t
is less and ratio will be less.
2
B. Changes in Intrathoracic Pressure of the Thoracic Cavity
These changes are necessary to move venous blood in the inferior vena cava to the heart.
Cyclical changes in intrathoracic pressure during breathing affect gas exchange and the
cardiovascular system. Thoracic cavity movements during breathing create a suction effect which
helps move venous blood through the inferior vena cava to the heart. The thin walled veins
alternately constrict on exhalation and dilate during inhalation as the pressure around the veins rises
and falls.
The Valsalva maneuver (holding your breath, by closing off the glottis, contracting the diaphragm
and contracting the abdominal wall muscles to increase intra-abdominal pressure) illustrates how
the inferior vena cava responds to intrathoracic pressure changes and the effect breathing has on
circulation. In this procedure, inhale maximally, hold breath. This forces air against closed glottis
increasing intrathoracic pressure to constrict the inferior vena cava. During ordinary breathing
intrathoracic pressure will decrease in the inspiratory phase and the inferior vena cava dilates and
blood is sucked up into it.
In the Valsalva maneuver, breathing rate (number of breaths/minute) and breathing amplitude
(depth of breathing) decrease. Pulse rate (number of heart contractions/minute) has increased and
pulse amplitude and blood volume ejected from the heart are decreased. The explanation for
changes in the pulse rate and amplitude: On holding the breath, blood cannot return to the heart.
To get blood to the tissues, heart beats faster, since less blood is pumped pulse amplitude decreased.
C. Control of Breathing
The level of CO
2
and H
+
ions in the blood affects the breathing centers to effect rate and depth of
breathing.
Breathing rate and depth are increased as the levels of CO
2
and H
+
ions are increased. Lowering
blood levels of CO
2
and H + ions lowers rate and depth of breathing (apnea).
Hyperventilation - blows off CO
2,
lowers blood CO
2,
this leads to apnea - shallow breathing and long
pauses between breaths.
Hyperpnea – increasing CO
2
and H
+
ions in the blood forces the breathing centers to increase rate
and depth of breathing.
3
D. Auscultation of Respiratory Sounds
Auscultation is listening to breath sounds produced within the body. Auscultation is an important
part of a physical examination. Obstructed airways are distinguished by wheezing or crackling
sounds as air passes through them.
Using the diaphragm side of the stethoscope, breathing sounds can be heard.
Bronchial sounds – air entering and leaving trachea and bronchi. The expiration duration is greater
than the inspiration, pitch of the sound on expiration is high. Place the stethoscope over the lower
part of the trachea and bronchi.
Vesicular sounds - air entering and leaving the alveoli. The inspiration duration is greater than the
expiration, pitch of sound on expiration is low.
Place stethoscope over the lungs.
4