NEONATAL STATUS AND DEVELOPMENT AND TEMPERAMENT
advertisement

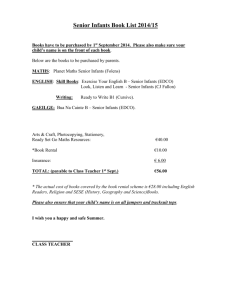
P138a DO VERY SICK NEONATES BORN AT TERM HAVE ANTENATAL RISKS? 1. INFANTS VENTILATED PRIMARILY FOR ASPHYXIA Sutton L, Sayer GP, Bajuk B, Richardson V, Berry G, Henderson-Smart DJ NSW Neonatal Intensive Care Units’ Data Collection, NSW Centre for Perinatal Health Services Research, Building DO2, Sydney University NSW 2006 E-mail: lsutton@mail.usyd.edu.au Aims: To describe the morbidity and mortality in a group of term neonates ventilated primarily for ‘perinatal asphyxia’, and ascertain antenatal and intrapartum risk factors for the neonatal morbidity. Methods: This was a population-based case control cohort study, conducted in Sydney and 4 large rural/urban Health Areas in New South Wales. The subjects, singleton term infants without a major congenital anomaly, were 182 cases admitted to a tertiary neonatal intensive care unit (NICU) for mechanical ventilation for > 4 hrs, and 550 randomly selected controls. This paper compares the 93 case infants ventilated primarily for ‘asphyxia’ related reasons with the controls. Risk factors for case/control status were analysed by maternal, antenatal, labour, delivery and combined epochs using logistic regression with results expressed in Odds Ratios (OR) and 95% Confidence Intervals (CI), p<0.05. Results: Significant predictors of case status were: Maternal epoch - Mother with no tertiary education (OR 2.56 [1.23, 5.32] p=0.012), primigravida (OR 1.98 [1.20, 3.26] p=0.007), pre-existing medical problem (OR 2.06 [1.05, 4.04] p=0.035). Antenatal epoch – any antenatal complication (OR 5.22 [3.17, 8.61] p=0.0001), birth weight <10th percentile (OR 2.20 [1.12, 4.33] p=0.02), male gender (OR 2.07 [1.27, 3.36] p=0.003). Labour epoch – rupture of membranes >24 hours but <8 days (OR 7.81 [1.05, 58.17] p=0.044), any complication of labour (OR 5.88 [3.33, 10.37] p=0.0001), induction of labour (OR 2.26 [1.34, 3.84] p=0.002). Prostaglandins was significant at (OR 2.42 [1.27, 4.60] p=0.007) in another model. Delivery epoch – forceps delivery (OR 3.56 [1.72, 7.38] p=0.0006), caesarean section in labour (OR 4.78 [2.67, 8.54] p=0.0001). The combined epochs – primigravida (OR 1.81 [1.05, 3.14] p=0.03), mother not having a tertiary education (OR 3.07 [1.36, 7.0] p=0.007), any antenatal complication (OR 3.49 [1.95, 6.23] p=0.0001), any complication of labour (OR 5.038 [2.61, 9.72] p=0.0001), caesarean section in labour (OR 2.00 [1.02, 4.04] p=0.049). Case infants had significantly higher rates than controls of thick meconium liquor (univariate OR 8.98 [5.08, 15.90] p=0.001) and antenatal fetal distress (OR 11.93 [7.26, 19.59] p=0.001). The median (25%, 75%) 5 minute Apgar for cases was 5 (3,8) and controls 9 (9,10). 40% of the cases had fits treated with anticonvulsants. 20 case infants (21.5%) died, 14 in the first 3 days. Of the 79 infants still alive on day 3, 39% were sedated/paralysed (3 died), 42% were neurologically normal, 19% were neurologically abnormal (3 died). Median (25%, 75%) age at discharge home varied from 10.5 (7, 15) days for the infants neurologically normal on day 3, to 18 (12,26) days for the survivors who had been sedated/paralysed on day 7. The median duration of hospital stay for control infants was 5 (3,6) days, and none died. 14% of controls were transferred to a special care nursery for feeding problems, respiratory distress, jaundice, and hypoglycaemia. Conclusions: This representative cohort of term infants ventilated primarily for ‘asphyxia’ had a significant burden of neonatal and longterm morbidity and mortality. Their mothers were more likely to have had medical problems before the pregnancy, antenatal complications, a complicated or induced labour and operative delivery. More detailed studies are needed to further elucidate the causal pathways to this morbidity, and devise preventative strategies. This study was supported by The Financial Markets Foundation for Children 270 P138b DO VERY SICK NEONATES BORN AT TERM HAVE ANTENATAL RISKS? 2. INFANTS VENTILATED PRIMARILY FOR RESPIRATORY PROBLEMS Sutton L, Sayer GP, Bajuk B, Richardson V, Berry G, Henderson-Smart DJ NSW Neonatal Intensive Care Units’ Data Collection, NSW Centre for Perinatal Health Services Research, Building DO2, Sydney University NSW 2006 E-mail: lsutton@mail.usyd.edu.au Aims: To describe the morbidity and mortality in a group of term neonates ventilated primarily for respiratory problems, and ascertain antenatal and intrapartum risk factors for the neonatal morbidity. Methods: This was a population-based case control cohort study, conducted in Sydney and 4 large rural/urban Health Areas in New South Wales. The subjects, singleton term infants without a major congenital anomaly, were 182 cases admitted to a tertiary neonatal intensive care unit (NICU) for mechanical ventilation for > 4 hrs, and 550 randomly selected controls. This paper compares the 86 case infants ventilated primarily for respiratory problems with the controls. Risk factors for case/control status were analysed by individual and combined epochs using logistic regression with results expressed in Odds Ratios (OR) and 95% Confidence Intervals (CI), p<0.05. Results: Significant predictors of case status were: Maternal epoch – mother’s age > 34 years (OR 2.13 [1.23, 3.71] p0.007), primigravida (OR 1.92 [1.2, 3.05] p=0.006). Antenatal epoch – any antenatal complication (OR 3.34 [2.08, 5.37] p=0.0001), birth weight <10th percentile (OR 2.81 [1.51, 5.24] p=0.001). Delivery epoch – forceps (OR 4.52 [2.16, 9.47] p=0.0001), caesarean section not in labour (OR 3.38 [1.83, 6.24] p=0.0001), caesarean section in labour (OR 4.00 [2.05, 7.80] p=0.0001), birth weight >90th percentile (OR 1.93 [1.08, 3.47] p=0.028). Infant characteristics – gestational age 37-38 weeks (OR 2.08 [1.28, 3.40] p=0.003), birth weight <10th percentile (OR 4.35 [2.32, 8.15] p=0.0001), birth weight >90th percentile (OR 2.75 [1.53, 4.95] p=0.0007). Combined epochs – any antenatal complication (OR 2.45 [1.47, 4.08] p=0.0006), birth weight <10th percentile (OR 3.36 [1.72, 6.55] p=0.0004), birth weight >90th percentile (OR 2.40 [1.29, 4.45] p=0.005), gestational age 37-38 weeks (OR 1.76 [1.03, 3.02] p=0.039), forceps delivery (OR 3.69 [1.69, 8.06] p=0.001), caesarean section not in labour (OR 2.37 [1.21, 4.63] p=0.012), caesarean section in labour (OR 2.76 [1.36, 5.63] p=0.005). 37% of the cases were 37-38 weeks gestation, compared with 22% of study controls. 36% (n=12) of the 37-38 week cases were born by caesarean section not in labour, compared with 23% of study controls. 9 of the 12 cases born at 37-38 weeks by caesarean section not in labour developed hyaline membrane disease. The median (25%, 75%) 5 minute Apgar for respiratory cases was 8 (7, 9) compared with 5 (3,8) for cases with perinatal asphyxia, and 9 (9,10) for controls. The median SNAP score for respiratory cases was 13 (9, 18) compared with 15 (9, 23) for cases with ‘perinatal asphyxia’. Their mortality rate was 5.6% (5/89). For the survivors the median (25%, 75%) duration of mechanical ventilation was 3 (2, 5.5) days and tube feeds 3 (1, 8) days. Age at discharge home (median, 25% 75%), varied from 8 (6,12) days for infants not sedated or paralysed and neurologically normal on day 3, to 29 (26,31) days for those sedated/paralysed on days 3 and 7. Conclusion: This representative cohort of term infants ventilated primarily for respiratory problems, had less neonatal morbidity and mortality than those infants ventilated for perinatal asphyxia. Their mothers were more likely to be > 35 years and have a complicated pregnancy. These babies were more likely to have been born by caesarean section, to be 37-38 weeks gestation, and to be either growth restricted or large for gestational age. This study was supported by The Financial Markets Foundation for Children 271 P139 NEONATAL STATUS AND DEVELOPMENT AND TEMPERAMENT AT SIX MONTHS Hardy H, Spence K, Halliday R Grace Neonatal Nursery, Royal Alexandra Hospital for Children/New Children’s Hospital, Sydney NSW 2000 In several studies, benefits from individualized family-focused care have been demonstrated for preterm infants. Reduced duration of illness and hospitalization, and improved development and behaviour are amongst the benefits. Similar advantages may also apply to full-term infants. Both groups of infants are represented in the NICU of a Children’s Hospital. Before commencing the formal introduction of a programme of family-focused care in Grace Neonatal Nursery, a base line profile of the neonatal and developmental/behavioural outcome characteristics of infants admitted to this unit was required, and an indication of the existing relationship between neonatal status and subsequent behaviour and development. Aims: To describe the neonatal characteristics of a cohort of infants, prior to implementing a programme of family-focused care in the NICU, to obtain measures of development and temperament at six months of age (adjusted for prematurity), and to compare gestational age and severity of illness with development and temperament at six months. Method: Neonatal data – gestational age, birthweight, age on admission, length of stay and severity of illness (SNAP score) – for each infant were collected from the unit database for a three month period, from December 1997 to February 1998. With informed consent, a postal questionnaire which included the Revised Gesell Parent Developmental Questionnaire and the Short Infant Temperament Questionnaire was sent to the parents when their infant was six months of age (adjusted for prematurity). Approval for the survey was obtained from the Ethics Committee of the Hospital. Results: There were 125 infants (77 male, 48 female) in the three month cohort. The average gestational age was 37 weeks, birthweight 2920g, age on admission 14 days and length of stay 10 days. The median SNAP score was 6 (range 0 to 29). Consent was obtained from 113 families but 12 were not sent the questionnaire as either the mother or baby had died, the baby was receiving terminal care, or the parents were non-English speaking or were foster parents. Two families could not be traced. The questionnaire was sent to 99 families, and 54 (54.5%) returned the completed questionnaire. Development and temperament scores were comparable to those of a normal sample, with a tendency for gross motor development to be delayed in comparison with other areas of development. Neither development nor temperament was significantly correlated with either gestational age or severity of illness. Conclusion: A pre-intervention base line has been successfully established, and the feasibility of obtaining follow-up data by postal questionnaire has been demonstrated. 272 P140 MOTOR DEVELOPMENT OF HIGH RISK INFANTS AT 18 MONTHS, 3 AND 5 YEARS Goyen T-A1, Lui K2 1 Department of Neonatology, Westmead Hospital, Westmead, NSW, 2145; 2 University of New South Wales, Sydney E-mail: mumbersj@ozemail.com.au Introduction: We previously reported fine motor deficits in NICU survivors, even amongst fine motor development of a group of high-risk infants who did not have a major disability at 18 months, 3 and 5 years. The motor development of “micropreemies” (born <27 weeks and/or <750 g) over this period was also examined. Methods: High- risk infants (<29 weeks gestation or <1000 grams) born between 1992 - 1993 were enrolled in the Growth and Development Clinic at Westmead Hospital for long term follow up. Infants who were identified with a neurological or intellectual disability at 12 months corrected age were excluded from the study. Gross and fine motor skills were assessed by an occupational therapist with the Peabody Developmental Motor Scales at 18 months corrected, 3 and 5 years of age. Results: A total of 58 eligible infants completed all assessments at the specified ages. The median (interquartile range) gestational age and birthweight for the sample was 28 weeks (27-29) and 942.5 grams (793.8-1090) respectively. STAGE 18 m 3y 5y p-value GROSS DMQ 90.0 (87-100) 91.0 (81-98) 79.0 (75-82) 0.000* MOTOR Deficit (%) 13.8 32.8 81.1 <0.001** FINE DMQ 84.0 (82-89) 89.0 (77-97) 84.0 (78-90) 0.56 MOTOR Deficit (%) 53.5 46.5 63.8 0.26 Median (interquartile range) are shown, DMQ= Developmental Motor Quotient *p<0.05 Friedman Test for repeated measurements; **p<0.05 Chi Square Test for Trend Gross motor quotient significantly decreased over time, and this trend was not confined to the subgroup of “micropreemies”. These children had particular difficulties with items of balancing and ball skills. However “micropreemies” (n=16) consistently performed lower on tests of gross and fine motor skills compared with the rest. Quotients were significantly lower at 5 years (gross motor p=0.007; fine motor p=0.003). Furthermore gross motor skills at 18m were significantly lower for the “micropreemies” (p=0.02). Conclusion: A significant proportion of infants without a major disability continued to have fine motor deficits from 18 months to 5 years, reflecting an underlying problem with fine motor skills. The proportion of infants with gross motor deficits significantly increased over this period as test demands became more challenging, particularly for the “micropreemies”. 273 P141 BEHAVIOURAL ADJUSTMENT, ADAPTIVE FUNCTIONING AND SELF-PERCEPTION AT 8 YEARS FOR CHILDREN BORN EXTREMELY PREMATURE Gibson F L, Bowen J R, Hand P J Neonatal Follow-up Program, Dept of Neonatology, Royal North Shore Hospital, St Leonards, NSW, 2065 E-mail: frgibson@laurel.ocs.mq.edu.au Aim: An increased incidence of behavioural difficulty among children born premature has been identified, however, few studies to date have examined premature children’s adaptive functioning or their self-perceptions. Behavioural adjustment outcomes have also been inconsistent partly due to the diversity between and within the samples studied, in addition to informant and measure issues such as reliability. This study aimed to examine the behavioural adjustment, adaptive functioning, and sense of competence and social acceptance of school-age children born extremely premature across home and school contexts. Methods: As part of a larger birth cohort study, 48 children born at <28 weeks gestational age and/or with a birthweight of <1000 grams, who attended a regular school at 8 years, were seen for follow-up assessments. A control group matched for gender, age, and school was also recruited. Demographic and social information was gathered through parent interview and questionnaires. Child behaviour was assessed with parent and teacher completed forms of the Child Behaviour Checklist (CBCL) and the Conners’ Rating Scales. The Vineland Adaptive Behaviour Scales were administered to assess child adaptive function and teachers completed the CBCL adaptive functioning scale. The Pictorial Scale of Perceived Competence (physical, cognitive), and Acceptance (peer, maternal) was administered to the children. Clinical cut-off scores were used to determine the incidence of behaviour problems and below adequate adaptive functioning within both groups. Results: There were no significant between group differences in demographic characteristics. The results of logistic regression revealed that significantly more premature children (13) than controls (2) were identified with behaviour problems on both of the parent completed measures (p =.01), however, only 4 premature children and 1 control child were identified with behaviour problems on both of the teacher completed measures. Very few children had clinical problems identified across all four measures, that is, on the parent and teacher completed CBCL, as well as the Conners’ scales. In terms of adaptive functioning, significantly more premature children were below adequate at home (premature 25%; controls 4%, p = .025) or in the problem range at school (premature 21%; 5% controls, p = .021). Finally, multivariate analyses indicated that premature children had a lower sense of competence than their peers (p = .025), although they did not differ in their sense of acceptance by others (p = .546). Conclusion: At early primary school age, children born extremely premature are more likely to have behaviour problems based on parent report and poorer adaptive functioning, both at home and at school, than their classmates While premature children may perceive that they have a lower level of physical and cognitive competence than their peers, this does not appear to impact negatively on their sense of acceptance by either their mothers or their friends. 274 P142 PERINATAL DETERMINANTS OF INTELLIGENCE AT AGE ELEVEN McConnell BA1, Thompson AJ2, Dornan JD3, Hepper PG1 1 School of Psychology, Queen’s University, Belfast, 2Department of Child Health, Queen’s University, Belfast, 3Department of Obstetrics and Gynaecology, Royal Group of Hospitals, Belfast Increasing attention has focused on the perinatal environment as an important period in determining outcome in later life. Much interest has been assigned to the Barker theory, relating low birth weight to adverse medical outcomes such as ischaemic heart disease. 1 However, there is limited research relating perinatal factors to developmental outcome measures such as intelligent quotient (IQ). Objective: This study aimed to compare fetal and early neonatal parameters with subsequent IQ scores in children aged 11 years. Design: 160 children (80 males), average age 11.9 years were included in the study. Previous perinatal measurements included birth and placental weight, skinfold thickness and mid-arm circumference, occipitofrontal circumference (OFC), length, ponderal index (birth weight (g) x 100/crown-heel length (cm3)), apgar scores and cord pH. Developmental outcome scores were measured using the British Ability Scales (version 2). IQ scores at age eleven were correlated with the perinatal measures using SPSS statistical package. Results: Pearsons Correlations (2 talied ) Cord pH -.156 .100 PL WT .095 .239 Lgth Head Scap Tricp .099 .222 -.096 .234 .107 .205 SNVA -.123 .193 .101 .209 .025 .754 .047 .562 SSA -.044 .641 .115 .152 .130 .109 -.061 .452 SVA SVA SNVA SSA BWT Pond .068 .418 Apgar 5 -.077 .339 .053 .511 -.040 .624 .090 .283 .149 .075 -.053 .512 .138 .085 .139 .087 .067 .428 .064 .446 -.067 .427 .121 .134 -.004 .964 Standard Verbal Ability Standard Non Verbal Ability Standard Spatial Ability Conclusion: Perinatal measurements did not correlate with developmental outcome measures (IQ) at age eleven years. There is no evidence that there is fetal programming of intelligence in later childhood. Barker DJB, ed. Fetal and infant origins of adult disease. London: BMJ Publishing Group, 1992. 275 P143 DO NEONATAL FACTORS INFLUENCE COMPLIANCE WITH 1-YEAR FOLLOW-UP McAvoy E, Bajuk B, Rochefort M Neonatal Intensive Care Unit, Westmead Hospital, Westmead NSW 2145 E-mail: bbajuk@mail.usyd.edu.au Aims: To identify the neonatal factors influencing compliance with the 1-year follow-up program for infants less than 29 weeks gestation at Westmead Hospital. Methods: All infants <29 weeks gestational age who were born 1/1/92 –30/6/98 and registered with the Growth and Development Clinic at Westmead Hospital. The data were analysed using SAS version 6.12 for Windows. Key Findings: There were 454 infants born during the study period. Of these infants 119 died before hospital discharge, 3 died before their first birthday and 332 were eligible for follow-up at 12 months of age (corrected for premature). 286 (86%) infants were assessed 46 (14%) infants were either lost to follow-up or refused to attend. The table shows the significant and non-significant factors associated with compliance at follow-up. Variable Multiple gestation Male gender Antenatal steroids Tertiary birth Caucasian Primipara Maternal age <25 HDP TPL ROM>24hrs APH Fetal distress IUGR Caesarian ROP grade 3 or 4 IVH grade 3 or 4 Infection BW GA TPN VENT LOS Apgar1 Apgar5 Not Attend 23.9 45.6 82.6 97.8 91.3 43.5 58.7 4.4 89.1 39.1 28.3 15.2 4.4 32.6 12.5 2.2 58.7 Median [25, 75] 946.5 [800, 1195] 27 [26, 28] 18.5 [13, 25] 42.5 [25, 55] 85 [69, 98] 5 [3, 6] 7.5 [6, 9] Attend 23.4 50.4 77.3 95.8 83.9 42.7 19.2 16.8 73.4 29.7 33.2 18.2 5.9 38.8 12.9 7.3 40.2 Median [25, 75] 940 [790, 1130] 27 [26, 28] 21 [14, 29] 45 [30, 62] 84 [70, 102] 5 [3, 7] 8 [6, 9] P value NS NS NS NS NS NS 0.001 0.029 0.021 NS NS NS NS NS NS NS 0.019 OR 95% CI 3.05 0.24 1.21 2.174-4.285 0.065-1.030 1.074-1.372 1.46 1.103-1.933 Conclusions: The mothers of infants who did not attend follow-up are more likely to be younger and have had threatened preterm labour. The infants are more likely to have had neonatal sepsis, and have had slightly less assisted ventilation and total parenteral nutrition. 276 P144 SIDE EFFECTS AND NEURODEVELOPMENTAL OUTCOME OF EARLY POSTNATAL CORTICOSTEROIDS IN PRETERM INFANTS Rajadurai VS, Agarwal P, Sriram B, Malathi I Department of Neonatology KK Women’s and Children’s Hospital, 100 Bukit Timah Road, Singapore 229899 E-mail: samuel@kkh.com.sg Background: Our centre was one of the centres that participated in the open study of early corticosteroids treatment (OSECT) in preterm infants with respiratory illness, the primary outcome measure being death or oxygen dependence at 36 weeks post-conceptional age (Trial Coordinator: Prof HL Halliday, Royal Maternity Hospital, Belfast). We report the adverse effects and neurodevelopmental follow-up of the infants enrolled into the trial from our centre. Objectives: To document the side effects and neurodevelopmental outcome at two years of infants exposed to early postnatal corticosteroids. Methods: Prospective randomised controlled trial. The entry criteria were gestation < 30 weeks, FiO2 > 0.30, age less than 72 hours, need for intubation and ventilation. Treatment allocation consisted of early steroids (within 72 hours), group 1 dexamethasone at weaning doses of 0.5mg/kg, 0.25mg/kg, 0.10mg/kg and 0.05mg/kg per day for a total of 12 days; group 2 Inhaled budesonide using aerochamber 400mcg twice daily for infants under 1000g and 600mcg twice daily for infants 1000g – 1500g for 12 days or until extubated. Late steroids (> 14 days) dexamethasone (group 3) or budesonide (group 4) was considered if the infants needed mechanical ventilation and oxygen. Follow-up at 2 years of corrected age: growth parameters, neurological examination, evaluation of hearing and vision, psychological assessment using Bayley Scales of Infant Development – 2nd edition and Vineland Adaptive Behaviour Scale). Results: Fifty infants were enrolled (group 1 = 13, group 2 = 12, group 3 = 13, group 4 = 12). There were 6 deaths (24%) in the early steroid (groups1 and 2) and 2 (8%) in the late steroid groups (groups 3 and 4). Survivors without CLD were not different between the early and late steroid groups, 11 (44%) vs 12 (48%) respectively. Overall, infants exposed to dexamethasone (groups 1 and 3, n = 26) had higher incidence of complications as compared against budesonide (groups 2 and 4, n = 24), namely severe hyperglycaemia 8 (31%) vs 2 (8%), gastrointestinal haemorrhage (GIH) 6 (23%) vs 3 (12%), gastrointestinal perforation (GIP) 3 (12%) vs 1 (4%), proven sepsis 11 (42%) vs 1 (4%), hypertension 1(4%) vs 0 (0%) in the respective groups (p=0.049). Early dexamethasone (group 1) had higher incidence of complications compared to the late dexamethasone (group 3) – severe hyperglycaemia 6 (46%) vs 2 (15%), GIH 5 (38%) vs 1 (8%), GIP 2 (15%) vs 1 (8%), and sepsis 7 (54%) vs 4 (31%) (p=0.10). Neurodevelopmental follow-up at 2 years of the 9 survivors of early dexamethasone (group 1) revealed normal cognitive development in 4 (44%), mild delay in 1 (11%), cerebral palsy 1 (11%) and significant developmental delay (MDI < 70) in 4 (44%). Conclusion: Early postnatal exposure of dexamethasone in very preterm infants seems to be associated with increased incidence of short-term adverse effects and also neurodevelopmental handicap at 2 years. A large-scale randomised trial, with survival free of neurodevelopmental handicap as the major end point needs to be done before its use can be recommended. 277 P145 HIGH HOSPITALIZATION RATE FOR RSV BRONCHIOLITIS (RSVB) IN TOWNSVILLE, AUSTRALIA: WOULD VACCINATION OF HIGH-RISK INFANTS BE COST EFFECTIVE? Whitehall JF, Bolisetty S, Norton R, Patole SK, Whitehall JS Kirwan Hospital for Women, Townsville, Australia E-mail: Whitehaj@health.qld.gov.au Background: An unusually high rate of hospitalization for RSV positive bronchiolitis (RSVB) exists in Townsville where 10% of the population is Aboriginal and Islander (AI). Palivizumab vaccine is known to reduce the hospitalization rate of RSVB. Aim: To study the rate of hospitalization, demographic & clinical characteristics of RSVB & the possible role of Palivizumab in Townsville. Design: Retrospective analysis of data on all children hospitalized in Townsville General Hospital for RSVB between Jan 97-Oct 99. Methods: Rate of hospitalization /1000 live births & severity of illness (duration of hospitalization & oxygen therapy) were analyzed according to-ethnicity (AI Vs non- AI), gender, birth weight, age & date of admission. RSVB cases were defined as those with positive immunofluorescence &/or culture. Based on reported efficacy of Palivizumab in reducing hospitalizations, the cost of routine vaccination of high-risk infants ( 2.5 kg at birth) was compared with the estimated cost of their hospitalization. Results: 88 cases of RSVB (AI: 30, non-AI: 58) were hospitalized during the study period. One (1%) died, 3 (3.4%) required admission in intensive care unit, 24(27%) added oxygen, 25 (28%) intravenous fluids. The overall hospitalization rate/1000 live births was 46 and 14 for AI and non-AI respectively (p<0.001); for those < 2.5 kg at birth it was 90 and 67 respectively. Severity of illness did not differ in the two ethnic groups. Mean duration of hospital stay was longer in those <2.5kg compared with those >2.5kg at birth [6 Vs 4 days, p 0.005] For those <2 kg at birth it was even longer [8 Vs 4 days, p 0.001]. Male: female ratio was 1:1.5 and 2.4:1 in AI and non-AI at all ages. 45 (51%) of children were admitted under 6 months of life, 66 (75%) under one year. A marked seasonal variation was noted in AI, with 28(93%) hospitalized in the first six months of the year. The peak month was March. An estimated cost of vaccine for all babies <2.5kg at birth during first 5 months of the year approximated A$190,000 compared with estimated hospitalization cost A$30960. Discussion: Our overall & birth weight specific (<2.5kg) hospitalization rates for AI (46/1000,90/1000) are significantly higher than those reported so far (USA: 4.7, UK: 14.3, Bedouin in South Israel: 18/1000). Our peak of admissions occurred during hot, late summer rains rather than in winter. Female predominance, as in AI, has not been reported. Conclusion: Even though, our high rate of hospitalization for RSVB, doubtless underestimates the true incidence, the cost of routine vaccination of all babies <2.5 Kg appears very high. 278 P146 THE QUALITY OF LIFE OF MOTHERS AND FAMILIES CARING FOR PRETERM INFANTS REQUIRING HOME OXYGEN THERAPY: A BRIEF REPORT McLean A3; Townsend A3; Clark J1; Sawyer MG1; Baghurst P1; Haslam R2; Whaites L1 Research & Evaluation Unit, Division of Mental Health1 & Department of Perinatal Medicine2, Women's and Children's Hospital, North Adelaide, 5006 and Adelaide Medical School3, Adelaide, 5000 E-mail: haslamr@wch.sa.gov.au Objective: To investigate the impact on mothers and families of caring for a premature infant requiring home oxygen therapy (HOT). Methodology: The subjects were the mothers of premature infants discharged home with oxygen from the Women's and Children's Hospital, Adelaide between September 1996 and February 1998. Mothers of preterm infants matched to within one month of age and not discharged on oxygen were used as controls. Twenty-six HOT infants were identified. Four mothers could not be contacted and 2 declined interview. HOT infants were divided into HOT and OFF-HOT groups depending on whether they were still on oxygen at the time of interview. After initial consent by letter, parents were interviewed. Standard questionnaires were used to assess family and maternal functioning. Their responses were analysed using a series of simple and multiple regression analyses. Results: HOT infants were more premature (25.2 vs 27.0 weeks) and of lower birthweight (737 vs 937 grams) than controls and there was a higher proportion of males (60% vs 35%). Mean scores on the Impact on Family Scale were significantly higher for those still on HOT (64.8±11.3) compared with those OFF-HOT (53.3±9.8) and the controls (49.0±9.2). Similarly, parental Quality of Life scores as assessed by the SF-36 were consistently lower for the HOT group, with OFF-HOT and control group scores being similar. After adjustment for gestational age, chronological age, birth weight and place of residence (urban/rural), the care required by premature infants receiving HOT had a significantly greater impact on their families than the care of infants not receiving HOT. Mothers of premature infants receiving HOT reported significantly less vitality and more mental health problems than mothers of infants not receiving HOT. Conclusions: (1) Caring for a premature infant on HOT may have an adverse impact on the lives of mothers and families. (2) The impact of HOT on mothers and families is limited to the period of time in which the infant is on treatment. (3) An increase in home supports is required for families of infants on HOT. 279 P147 SIDS AWARENESS IN NORTH QUEENSLAND: A SURVEY OF INFANT SLEEPING PRACTICES IN INDIGENOUS AND NON-INDIGENOUS WOMEN Panaretto K, Smallwood VE, Cole P, Whitehall J Townsville Aboriginal and Islander Health Service (TAIHS) and Kirwan Hospital for Women, Townsville, Thuringowa, Qld 4817 E-mail: whitehaj@health.qld.gov.au Background: Sudden Infant Death Syndrome (SIDS) is the most common cause of postneonatal death in Queensland (0.98 per 1000 live births, 1994-1996). SIDS rates have fallen dramatically in the non-indigenous population due to aggressive risk reduction education. A recent review of SIDS deaths in North Queensland suggests the rate in the indigenous population is up to 6 times that of the non-indigenous population, consistent with other states. This may be because education campaigns are not reaching the indigenous population. Aim: To assess infant sleeping practices and awareness of SIDS risk factors in the indigenous and non-indigenous population of Townsville, a large remote urban centre in North Qld. Methods: A random sample of 60 young mothers, 30 Indigenous (Murri) women and 30 nonindigenous, with children less than 2 years of age were surveyed using sections of the West Australian Infancy and Pregnancy Survey 1997-1998, developed by the TVW Telethon Institute for Child Research, Princess Margaret Hospital, Perth, Western Australia. The women were interviewed over a three week period in Townsville. The prevalence of SIDS risk factors, including demographic data, smoking, infant feeding, sleeping position, bedding, and bed sharing have been assessed in the two groups. SIDS awareness was also assessed, as were suggestions for appropriate SIDS education for Murri women. Incidence, medians and univariate association (2) between indigenous and non-indigenous groups will be performed where appropriate using SPSS. Results: The Murri women were significantly younger and more likely to be single than the NonIndigenous women. There was no significant difference in the median age of the infants between the two groups (8 months, range 0.3-26). 53% of the Murri women smoked during pregnancy, 23% of Non-Indigenous women (p=0.015); 60% of Murri women were smokers at the time of the interview; 50% of the Murri partners smoked and smoking occurred in 40% of Murri households (27% and 20% respectively for Non-Indigenous women). 83% of women in both groups reported having breast fed at any time, with 30% of Murri women still breast feeding at the time of interview (cf 47% of Non-Indigenous women). 37% of Murri infants slept prone (cf 16%), 93% slept in the same room as their parents, 77% shared a bed (cf 13% of Non-Indigenous infants). The Murri households had significantly more members with 50% including extended family members (cf 23%). 33% of Murri women were strongly SIDS aware compared with 93% of Non-indigenous women. However, 60-75% were aware of individual risk factors on specific questioning. The Murri women believe that sleeping with their infants will protect them. Conclusion: This small survey suggests prevalence of SIDS risk factors are higher in the Murri population and a new approach to education is urgently needed to promote SIDS awareness amongst Murri women. 280 P148 AN ANALYSIS OF SUDDEN UNEXPECTED DEATHS IN INFANCY IN QUEENSLAND, 19941997 Chandran G, Hockey R, Brookes K*, Colditz P**,Naylor C**, Payton D** Perinatal Epidemiology Unit, Mater Hospital, Brisbane & **The Queensland Council on Obstetric and Paediatric Morbidity and Mortality; * SIDS Queensland E-mail: Jking@mater.org.au Aims: To analyse all sudden unexpected deaths of infants (SUDI) in Queensland between 1994 and 1997, in order to determine the relative contribution of deaths from Sudden Infant Death Syndrome (SIDS) and to explore differences between the Indigenous and non-Indigenous populations. Methods: This is a population-based study of all infant deaths registered in Queensland from 1994 to 1997. On the basis of information obtained from death certificates, autopsies and other relevant information, predetermined criteria were applied to identify those infants whose deaths were sudden and unexpected, and to classify them into SIDS or non-SIDS. As information on Indigenous status has been recorded only since 1997, comparisons between Indigenous and nonIndigenous populations were only possible for that year. Findings: There were 1333 infant deaths in the four year period 1994-1997, giving an infant mortality rate of 7.1 per 1000 live births. Two hundred and sixteen deaths (16.2%) were categorised as sudden and unexpected (SUDI). One hundred and eighty of the SUDI deaths were classified as SIDS (83%), and 36 as non-SIDS. The overall rate of SUDI for this period was 1.15 deaths per 1000 live births and the SIDS rate was 0.96 per 1000 LB. The majority (78%) of the non-SIDS cases resulted from injuries and were more likely than SIDS cases to occur at age greater than six months. SIDS occurred predominantly (92%) prior to the age of six months. Males were disproportionately represented in both the SIDS and non-SIDS cases (69% and 61% respectively). Over the four-year period, the rate of SIDS declined from 1.05 per 1000 live births to 0.96 but this was not statistically significant. The rate of non-SIDS deaths increased from 0.17 per 1000 live births to 0.32 per 1000 LB, again not statistically significant. In 1997, the rate of SUDI deaths was 5 times higher for Indigenous infants, (4.84 cf 0.98 per 1000 LB, p<0.01) and the SIDS rate was 5.9 times higher, (4.04 cf 0.69 per 1000LB, p<0.01). Conclusions: The apparent marginal decline in the rates of SIDS and increase in SUDIs from causes other than SIDS over the period 1994-1997 may be indicative of an emerging trend, and warrants further analysis, particularly for Indigenous deaths. The disproportionate rate of SIDS among Indigenous infants is again highlighted. Public health messages about SIDS prevention may not be as effective for the Indigenous community. Educational interventions in the perinatal period may also be need to be broadened to include consideration of sudden unexpected infant deaths from other preventable causes 281 P149 CORTISOL DEFICIENCY, ANDROGEN EXCESS AND REDUCED THYROID FUNCTION IN < 30 WEEK GESTATION INFANTS ? HORMONAL FACTORS IN THEIR MORBIDITY Yeung MY1,2, Smyth JP2 1 Department of Pharmacy, 2 Department of Neonatal Intensive Care, Nepean Hospital, Sydney, NSW E-mail: yeungm@wahs.health.nsw.gov.au Exogenous surfactant, the wider use of antenatal and postnatal steroids and improvements in ventilation have not reduced chronic lung disease (CLD) in preterm infants < 30wks gestation to the extent that was hoped. This may be a cost of their increased survival. Antenatal steroid therapy reduces RDS, IVH and NEC and matures the surfactant profile briefly. Mega-dose postnatal dexamethasone (0.5mg/kg per day starting dose) reduces CLD at 28 days of age and 36 wks postconceptional age (PCA) in these infants. This short-term benefit has however, been associated with an increased risk of adverse neurodevelopmental outcome. Cortisol is known to modulate fetal heart and lung development, as well as the maturation of a variety of enzyme and biochemical pathways. Preterm infants < 30 wks gestation are relatively cortisol deficient with elevated cortisol precursors. They have a poor cortisol response to stress in their first postnatal weeks. These findings are consistent with the structural and biochemical immaturity of the adrenal gland. They also have an immature hypothalamic-pituitary-thyroid hormone axis and reduced tissue thyroid hormone responsiveness. Superimposed on this is the further reduced thyroid function seen in non-thyroidal illness in which elevated cytokine levels have been implicated. Repeated antenatal steroids and high dose postnatal dexamethasone are “unphysiological”, may not have the protective action of cortisol and appear to be deleterious to lung and brain growth. This may be through inhibition of cell replication and catabolism, as well as decreased TSH secretion and reduced peripheral conversion of T4 to T3. Extremely preterm infants have elevated androgens and androgen precursors, the steroid products of the adrenal fetal zone. The production of fetal androgens persists and the androgen levels remain elevated in these infants until 42 wks PCA. This corresponds to the timing of involution of the fetal zone in the adrenal gland and appears unaffected by preterm birth. Preterm boys are known to have a worse outcome and a higher incidence of CLD for reasons that are not well understood. Fetal androgens, e.g., androstenedione and dehydroepiandrosterone (DHEA), have been shown, in vitro, to have an anti-glucocorticoid and an inhibitory effect on human fetal lung growth and maturation. Postnatal cortisol deficiency may deprive the low gestation infant of the optimum protective and maturational effects of this hormone, resulting in over-exuberant cytokine production and inflammatory responses. Considered together, the relative cortisol deficiency/androgen excess and thyroid immaturity in these infants may be factors in their high level of morbidity. It is conceivable that a period of early low-level postnatal hydrocortisone (cortisol) administration could improve the pulmonary as well as the overall outcome of these infants. It may also reduce the need for higher dose glucocorticoid treatment and the associated side effects. A multi-centre randomised controlled trial of early low-dose hydrocortisone appears warranted. 282 P150 COMPARISON OF TEMPERAMENT AT 12 MONTHS BETWEEN CASES AND CONTROLS IN THE NSW TERM BABIES’ STUDY Sutton L, Bajuk B, Gibson F, Berry G, Henderson-Smart DJ NSW Neonatal Intensive Care Units’ Data Collection, NSW Centre for Perinatal Health Services Research, Building DO2, Sydney University NSW 2006 E-mail: lsutton@mail.usyd.edu.au Aims: To compare maternal assessment of temperament at 1 year between cases and controls enrolled in the New South Wales (NSW) term babies’ study. Methods: This was a population-based case control cohort study, conducted in Sydney and 4 large rural/urban Health Areas in New South Wales. The subjects, singleton term infants without a major congenital anomaly, were 182 cases admitted to a tertiary neonatal intensive care unit (NICU) for mechanical ventilation, and 550 randomly selected controls. Follow-up at 1 year included physical examination, Griffiths Mental Developmental Scales (1996 revision), Ages and Stages Questionnaire and Toddler Temperament short questionnaire (TTQ). Risk factors for TTQ scores of cases and controls were analysed using logistic regression, with results expressed in Odds Ratios (OR) and 95% Confidence Intervals (CI), p<0.05. Results: TTQ’s were completed for 91.3% of 150 eligible cases (n=137), and 90.8% of 447 eligible controls (n=406). This included 16 of the 18 children with a provisional diagnosis of cerebral palsy. Significantly more controls (14.3%) than cases (5.8%) were scored as being difficult on the TTQ (p=0.031). Similar proportions of cases (16.1%) and controls (15.8%) were scored as being easy, with more cases (78.1%) than controls (70%) in the average temperament category. There were no significant differences between cases and controls on the TTQ subscales. In logistic regression significant associations with difficult temperament were: Cases - non-Caucasian (OR 4.8[1.05, 22.2] p=0.04), unemployed father (OR 6.5[1.28, 33.25] p=0.02). Controls - non-Caucasian (OR 2.6[1.33, 5.15] p=0.005), on medications (OR 2.66[1.17, 6.07] p=0.02), admission for minor surgery (OR 5.87[2.03, 16.97] p=0.001). Significant associations for scoring in the more difficult range for the subscales were: Withdrawn/shy – Cases: cerebral palsy (CP) (OR 7.48 [2.02,27.69] p=0.003), female (OR 4.45 [1.43,13.76] p=0.009). Controls: weight <10th percentile (OR 2.58 [1.01, 6.6] p=0.048). Overreactive – Controls: mother who had not completed the higher school certificate (OR 1.68 [1.06,2.67] p=0.028). The whole group: males (OR 1.68 [1.12,2.51] p=0.012). Uncooperative – Cases: unemployed father (OR 8.79 [2.12, 36.46] p=0.003), male (OR 4.63 [1.05,20.34] p=0.043). Arrhythmic – Cases: mother who had not completed the higher school certificate (OR 8.00 [1.75,36.62] p=0.007), Asian (OR 7.00 [1.65,29.72] p=0.008). Conclusions: The demographic associations with difficult temperament and its various dimensions in this cohort are comparable with those of the original normative sample. Admission to hospital and longterm medication in the first year of life, were associated with difficult temperament in the control children. It is encouraging that cases are not perceived as being more difficult than controls. Most of the children in this cohort with CP had a severe functional disability, and were perceived as withdrawn. These results will be compared with temperament outcomes at 3 years. This study was supported by The Financial Markets Foundation for Children, NSW Health Department, APEX Foundation for Research into Intellectual Disability 283 P151 NUTRITIONAL CONSEQUENCES OF INDOMETHACIN (INDO) THERAPY FOR PATENT DUCTUS ARTERIOSUS (PDA) IN 750-1250GM PREMATURE INFANTS – A CASE-CONTROL STUDY Dodd G, McPhee A Dept Neonatal Medicine, Women’s and Children’s Hospital, North Adelaide 5006 E-mail: mcphee@wch.sa.gov.au Study Aims: INDO therapy for the treatment of PDA in premature infants <1250gms is frequently associated with protracted renal dysfunction requiring fluid (and nutrient) restriction. We assessed, via a case-control study, the impact of INDO therapy on nutrient intake and weight gain in the first month of life in premature infants of 750-1250 gms birth weight. Methods: Case-control study of babies managed in the NICU at the WCH between 1994 and 1998; two weight cohorts, 750-999gms and 1000-1250gms were studied. Infants with PDA treated with INDO (INDO group) were matched for birth weight (+/-100gms), gestational age (+/-1 wk) and sex with infants without PDA, (NO INDO group). Case note audit was used to determine clinical profiles, together with detailed fluid and nutritional intakes (enteral and parenteral) on days 4, 8, 12, 16, 20, 24 and 28. Comparisons between INDO and NO-INDO groups within each birth weight cohort were made using ANOVA with repeated measures; a calorie intake of 90-100 cals/kg/day was considered a desirable target intake for growth. Results: By design, the groups were well matched for birth weight, gestational age and sex; their clinical profiles were also comparable. Calorie intake (a) and weight gain (b) for each birth weight cohort are shown. INDO infants had lower calorie intakes on days 8 and 12 in the 750-999gm cohort and on days 8-20 in the 1000-1250gm cohort. In both cohorts INDO infants achieved target calorie intakes later than NO-INDO infants, and showed lower bodyweights at 20-28 days. a. Calorie Intake For Babies 750-999 g a. Calorie Intake For Babies 1000 - 1250 g Mean Calories / kg / day Mean Calories /kg /day 140 120 100 80 60 40 20 0 4 8 PDA 12 16 20 24 Post Natal Day 120 100 80 60 40 20 0 4 28 1200 1450 1150 1400 1100 1350 Weight (grams) Weight (grams) 12 16 20 24 Post Natal Days 28 N=22/group b. Weight During First 28 Days (1000-1249 g) b. Weight During First 28 Days (750-999 g) 1050 1000 950 900 1300 1250 1200 1150 1100 850 1050 4 indomethacin 800 4 indomethacin 8 PDA No PDA N=15/group No PDA 140 8 12 16 20 24 28 Post Natal Day 8 12 16 20 24 28 Post Natal Day no indomethacin no indomethacin Conclusions: INDO therapy is associated with significant calorie restriction and diminished weight gain in the first month of life in infants with birth weight 750-1250gms (these adverse nutritional consequences of INDO may have long term implications). 284 P152 RESISTIVE INDEX FROM RENAL ARTERIAL DOPPLER IN THE DIAGNOSIS OF SIGNIFICANT PATENT DUCTUS ARTERIOSUS IN PRETERM INFANTS Armstrong DL, Harding JE, Teele RL National Women’s Hospital, Auckland, New Zealand E-mail: damiena@ahsl.co.nz Background: Up to 50% of preterm, extremely low birth weight neonates will have a patent ductus arteriosus (PDA). Because a PDA is associated with problems such as cardiac failure, intraventricular haemorrhage and necrotising enterocolitis, prompt diagnosis and treatment is important. Clinical examination and radiographs of the chest are known to be unreliable in the diagnosis of PDA. Although the “gold standard” investigation is direct visualisation of the PDA by echocardiography, this procedure is not always available in every neonatal unit. It is known that renal arterial waveforms are altered by the presence of a PDA but a prospective study comparing echocardiography with renal Doppler investigation, within minutes of each other, has not been performed. We undertook such a study. Aims: This study compares the findings from echocardiography and renal arterial Doppler examination in preterm infants suspected of having PDA. Methods: In preterm infants at risk for PDA, renal ultrasonograms, including Doppler study, were performed immediately before or after echocardiography. Echocardiograms were performed by one of three investigators. A single investigator, who was not involved in the infant’s care, performed the renal scans. The ductus arteriosus was identified using colour Doppler, images were frozen on screen and the ductus arteriosus was measured using electronic callipers. A PDA >1.5mm diameter was considered significant. Other information obtained included left atrial/aortic ratio, size of foramen ovale, presence of a left to right shunt and flow pattern in the descending thoracic aorta. Immediately before or after echocardiograms, both renal arteries were identified on ultrasonography and a pulsed wave Doppler display was acquired. Resistive index (RI), using measurements of the peak systolic and end diastolic renal arterial velocities was obtained for each renal artery. Findings: Forty-one scans were performed on 27 babies. Mean gestational age was 26.8 weeks (SEM 0.4), mean birthweight was 915g 55 and mean postnatal age was 12.2 days 2. A receiver operator curve was plotted and used to determine optimal cut off values for the RI. When the renal artery RI was >1.1 the likelihood ratio for having a significant duct was 13.7 (sensitivity 82%, specificity 94%). When the renal RI was < 0.9 the likelihood ratio for having a significant PDA was 0.2 (sensitivity 45%, specificity 100%). Conclusions: Resistive index obtained from renal arterial Doppler represents a simple investigation that can be used to predict a significant PDA. 285 P153 HAEMOLYSIS AFTER INFUSION OF PACKED RED CELLS THROUGH PERCUTANEOUS CENTRAL VENOUS CATHETER-AN IN VITRO STUDY Tuladhar R, Porter D, Patole SK, *Muller R, Whitehall JS Kirwan Hospital for Women, *James Cook University, Townsville, Qld Background: Percutaneous central venous catheters (PCVC) are often used in neonates needing long term venous access. Data on haemolysis after infusion of packed red cells (PRBC) through PCVC is not available. Aim: To compare occurrence / extent of haemolysis after PRBC transfusion through PCVC with that after infusion through peripheral intravenous cannula in an in vitro study. Methods: 20 mls of PRBC ready for use in neonates, were transfused at 5ml / hour over 4 hours through either a 23 G silicone PCVC [Vygon, Germany, (n=9)] or 24 G cannula [Insyte, Becton, USA, (n=9)]. PRBC packets were assigned to “PCVC” or “Cannula” group according to computer generated random numbers contained in 18 sealed coded envelopes. Transfusion equipment [30 ml syringes (Terumo, USA), syringe pump (Atom 1235,USA), 3 way tap (Connecta TH, Sweden), extension set (B. Brauwn, Malaysia)] and environmental temperature (24+20C) were similar for all experiments. Significant haemolysis was defined prospectively as rise in free haemoglobin (FHb) by>0.15% midway through and/or at the end of transfusion. For each experiment 5 blood samples were collected- (1) From PRBC packets before starting transfusion. From the tip of cannula / PCVC –(2) at commencement of transfusion (3) midway through the transfusion (4) at end of transfusion &(5) from residual blood in the syringe at end of transfusion. The samples were immediately centrifuged at 100g for 5 minutes & the supernatant plasma was analyzed for FHb by a Coulter MAXM Hematology analyzer. Statistics: Non parametric tests were used due to skewed distributions. Results: Median (25%-75%) FHb in PRBC packets, were 10 (3-10) gram % and 4 (3-10) gram % for PCVC and Cannula group respectively. Median (25%-75%) FHb levels in samples 2-5 are shown below Table1 PCVC (Vygon) n=9 Cannula (Insyte) n=9 Sample number FHb: median(25%-75%) FHb: median(25%-75%) 2 start of Transfusion (Tx) 2.5 (2-8.2) 2.0 (2-7.5) 3 Midway through Tx 3.5 (2-9) 3.0 (2-7.5) 4 End of Tx 3.5 (2.2-9) 3.0 (2-8) 5 Residual blood in syringe 3.5 (2-8.2) 3.0.(2-8) Median (range) differences in FHb for samples 3 Vs2, 4Vs2 &5Vs2 were not significantly different for PCVC and Cannula (Wilcoxon rank sum test: all p>0.5) Conclusion: PCVC may be used for PRBC transfusions. (Acknowledgements: Queensland Surgical) 286 P154 EFFECT OF EARLY TARGETED INDOMETHACIN ON THE DUCTUS ARTERIOSUS AND UPPER BODY BLOOD FLOW IN THE PRETERM INFANT Osborn DA, Kluckow M, Evans N Departments of Neonatal Medicine, Royal Prince Alfred and Royal North Shore Hospitals, and Department of Obstetrics and Gynaecology, University of Sydney, Sydney, NSW E-mail: davido@peri.rpa.cs.nsw.gov.au Aim: To determine the short term effect of indomethacin on ductus arteriosus (PDA) constriction and blood flow to the upper body and brain in the early postnatal period. Background: Early low superior vena cava (SVC) flow is associated with large diameter PDA and subsequent intraventricular haemorrhage when SVC flow improves. We hypothesised that ductal constriction induced by indomethacin would increase SVC flow when the infant's spontaneous postnatal ductal constriction had failed. Methods: The study was a randomised, double blind, crossover trial of indomethacin (Indo) versus placebo. 111 infants born before 30 weeks had echocardiograms at 3 and/or 10 hours. Trial packs had 2 identical vials (labelled A and B) randomly allocated to contain Indo 0.2 mg/kg or placebo. Infants were eligible if the colour Doppler PDA diameter was >1.6mm. All infants received vial A first. Echocardiogram was repeated 1 hour after vial A. Crossover to vial B occurred if the PDA was still >1.6mm and constriction was <30%. Further echocardiograms were done 1 and 2 hours post intervention. Primary outcomes were SVC flow (mls/kg/min) and ductal constriction. Results: 70/111 (63%) infants had a ductus > 1.6mm and were randomised at mean age 4 hours. 35 had Indo first and 35 placebo first. The 2 groups were well matched. One hour after the first vial, there was no difference between the two groups in degree of ductal constriction (placebo: -15% vs Indo: -20%), change in SVC flow (placebo: -9% vs Indo: -1%) or right ventricular output (placebo: +2% vs Indo: -5%). 53 infants given Indo (either as vial A or vial B) had blinded but non-placebo controlled measures at 2 hours. At this time, there was a significant PDA constriction (mean 2.4 to 1.5mm, p<0.001), no change in SVC flow (mean 71.9 to 70.5 mls/kg/min) and a small but significant reduction in RVO (mean 198 to 180 mls/kg/min; p = 0.001). After Indo, babies born before 27 weeks showed greater falls in RVO and SVC flow than those born after 26 weeks. (Change RVO: -17% vs -2%, p = 0.001; and change SVC flow: -11% vs +14%, p = 0.07). Conclusions: Indomethacin had minimal effect on PDA constriction at 1 hour and no consistently positive or negative effects on blood flow. Significant ductal constriction had occurred 2 hours after indomethacin and flow measures tended to fall in less mature babies while being maintained in the more mature. 287 P155 COULD ILEUS DURING PHOTOTHERAPY IN NEONATES BE A DIRECT EFFECT OF LIGHT? Kadalraja R, Patole SK, *Muller R, Whitehall JS Kirwan Hospital for Women, *James Cook University, Townsville, Australia Background: Phototherapy (PT) is shown to cause vascular smooth muscle relaxation in animal experiments. Association of PDA with PT is reported in neonates <1.5 kg. Abdominal distension, Ileus & bile stained aspirates are common in neonates under PT. Direct photorelaxation of gut smooth muscle or gut ischemia due to stealing of mesenteric flow by peripheral vasodilatation may be responsible for ileus during PT. In term neonates, postprandial increase in velocity of blood flow to gut is reported to be significantly less after PT. Data on gut flow (in absence of associated risk factors for ileus) after commencing PT in preterm neonates is not available. Objective: To compare mesenteric flow before & after commencing PT in stable, preterm neonates with no associated risk factors for ileus Design / Methods: Superior mesenteric artery blood flow (maximum, minimum velocity & resistive index) was measured by ultrasound pulsed-Doppler method in 6 consecutive neonates before and 8-12 hours after commencing continuous PT. At the time of study they did not have associated risk factors for ileus (PDA, indomethacin /aminophylline /morphine /pancuronium therapy, polycythemia, sepsis, electrolyte imbalance, umbilical vascular catheters & enteral feeds) their ventilatory/ oxygen needs were minimal & cardiovascular support was not required. Results: Birth weight, gestational age & postnatal age of enrolled neonates at study ranged from 885-1410 grams, 27-29 weeks & 2-4 days respectively. Mean +(Sd) level of serum bilirubin before starting PT & at flow recording was 130+ 52 & 165+ 40 mmol/litre respectively. Table: Mesenteric flow (m/sec) before and after PT V max V min RI Cases Pre Post Pre Post Pre Post 1 0.38 0.38 0.10 0.10 0.74 0.74 2 0.51 0.39 0.02 0.15 0.62 0.62 3 0.51 0.47 0.08 0.08 0.80 0.85 4 0.49 0.64 0.03 0.18 0.79 0.72 5 0.14 0.61 0.03 0.21 0.79 0.66 6 0.35 0.55 0.12 0.21 0.66 0.62 Mean + (Sd) Maximum (V max) velocity, & resistive index (RI) before (Pre) and after (Post) commencing PT were not significantly different. [Pre Max: 0.39+0.14 Vs Post Max: 0.15 +0.05, p=0.26] [Pre RI: 0.73 +0.07 Vs Post RI: 0.7 +0.08, P=0.27] Minimum (V min) velocity Post RI was significantly increased. [Pre Min: 0.06 +0.04 Vs Post Min: 0.15 + 0.05, p=0.03] Conclusion: Overall, mesenteric flow did not change significantly post PT. Increased diastolic flow post PT flow may possibly be due to photorelaxation of mesenteric vessels. Development of ileus in absence of associated risk factors may be due to direct effect of light on gut smooth muscle if mesenteric flow is unchanged. 288