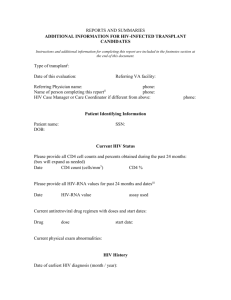
Initial Work-up of HIV infected Adult
advertisement

J Cohn MD 13 July 2014 Initial Work-up of HIV-Infected Adult 1) Obtain documentation to confirm HIV infection to adhere with HRSA standards a) copy of antibody test result OR b) repeat antibody test at your site 2) Complete history to document current health status with additional attention to: a) HIV exposure history b) Sexually transmitted infections or complications of substance abuse c) Partner counseling and referral for possible source of infection and possible recipients of infection d) Current transmission behaviors and current exposed persons e) Presence of depression or domestic violence f) Prior treatment g) Medication allergy and intolerence h) Psychosocial supports 3) Complete Physical Exam with special emphasis on a) Skin lesions b) Oral lesions c) Lymphadenopathy d) Genital and perirectal lesions 4) Tuberculin Skin Test or interferon-gamma releasing assay (IGRA) 5) Basic Laboratory tests: a) CD4+ lymphocyte count* b) Quantitative plasma HIV RNA level by RT-PCR (Roche Cobas Taqman or Amplicor, Abbot RealTime), bDNA (Versant HIV RNA) or RNA amplification (Nuclisens HIV1 QT)* c) HIV genotype or other resistance test for previously untreated patients (Reverse Transcriptase and Protase mutations; integrase genotype only for suspected integrase resistance) d) CBC with differential and platelet count e) Tests of liver and renal function, electrolytes and phosphorous f) Urine analysis g) Serologic test for syphilis h) Hepatitis A IgG antibody to determine potential value of Hepatitis A Vaccine i) Hepatitis B serology to determine need for Hepatitis B vaccine (Hep B Surface Antigen, Hep B Surface Antibody, Hep B Core Antibody) j) Hepatitis C antibody because of the high rate of co-infection with Hepatitis C k) Baseline Toxoplasma antibody l) Baseline fasting glucose, total cholesterol, HDL (and LDL) cholesterol and triglycerides should be performed before initiating antiretroviral therapy. m) Baseline urine or urethral gonorrhea and Chlamydia testing (nucleic acid amplification tests are the most convenient) n) For persons having receptive anal intercourse (men or women): anal swab for gonorrhea and Chlamydia (NAAT has excellent test characteristics but is not certified for this use) o) For persons having oral sex, pharyngeal swab for gonorrhea and Chlamydia (NAAT has excellent test characteristics but is not certified for this use; Chlamydia is not necessarily a pharyngeal pathogen) *Two baseline values of CD4 count and plasma HIV RNA are desirable. In situations where the results are extreme and consistent with the clinical presentation repeat tests may not be necessary. Plasma HIV RNA levels may be elevated above the patient’s baseline during acute infections or inflammatory episodes and following a vaccination: ideally HIVRNA testing should be postponed if initiating therapy can be delayed. Page 1 of 5 J Cohn MD 13 July 2014 Additional/Optional laboratory tests p) HLA B*5701 assay to be used before abacavir is prescribed q) CCR5 cell tropism assay to be used before a CCR5 antagonist is prescribed r) Consider G6PD level: screen for deficiency in susceptible men or test prior to dapsone or primaquine use (especially in men from the Mediterranean, India, or Southeast Asia) s) Baseline HSV-2 specific (Glycoprotein G2) IgG antibody (consider in persons with a history of STDs or genital ulcers t) Baseline CMV antibody test for persons from usual prevalence populations (not needed for IDU or MSM who are very likely to be infected) u) Varicella antibody (may be done in persons without a history of chicken pox or zoster) 6) Women specific evaluation a) Use of, and need for, contraception b) Vaginal exam for i) Assessment of vaginitis/vaginosis ii) Pap smear iii) Screen for cervical gonorrhea and Chlamydia (nucleic acid amplification tests are the most convenient) and vaginal Trichomonas (wet mount and/or Trichomonas culture). Note all women <25 years should be screened for chlamydial infection. 7) Evolving standards a) Consider anal Pap smear among persons who had anal receptive intercourse (men or women) and those with anogenital warts; can consider for women with cervical dysplasia. Recommended Health Maintenance Adherence with care and transmission behavior monitoring For everyone: Inquire about ongoing sexual activity or substance use and symptoms of STIs at each visit in order to provide targeted brief prevention messages or feedback, or to refer for behavior change counseling or drug treatment. Opportunistic Infection Prophylaxis For CD4 count <= 200 Initiate Pneumocystis prophylaxis (trimethoprim-sulfamethoxazole DS one daily or TIW, OR dapsone 100 mg daily, OR atovaquone 1500 mg daily) For CD4 count <= 100 Test for serum toxoplasma antibody Provide toxoplasma prophylaxis for persons with positive antibody result (TMS SMX DS one daily or add weekly pyrimethamine 50 mg/leucovorin 25 mg to daily dapsone ). Monthly self test for visual acuity or ophalmology exam every 6 months For CD4 count <= 50 Initiate prophylaxis for Mycobacterium avium complex (MAC) with azithromycin 1200 mg daily When to stop prophylaxis: For CD4 count > 100 for 3-6 months with effective antiretroviral therapy Can safely discontinue prophylaxis for M. avium For CD4 count > 200 for at least 3-6 months with effective antiretroviral therapy Can safely discontinue prophylaxis for Pneumocystis jirevicii Page 2 of 5 J Cohn MD 13 July 2014 Vaccines For everyone: Pneumococcal vaccine: Pneumococcal conjugate vaccine (PCV13) should be given followed at least 2 months later by PPV23 (see below). If PPV23 is given first, then PPV23 should be given one year after PCV13. Pneumococcal polysaccharide vaccine (PPV23) should be given at least 2 months after PCV13 and when the CD4 count >=200 cells/cu mm. If given initially at lower CD4 count, consider repeating when CD4 count rises above 200. CDC recommends consideration of repeat vaccination once 5 years later and/or at age 65/ Annual inactivated Influenza vaccine for each season (live influenza vaccine is contra-indicated for HIV+ patients). Hepatitis B vaccination (3 doses) and Hepatitis A vaccination (2 doses) for susceptible persons especially Hepatitis C infected person . Can use 3 doses of combined vaccine for both Hepatitis A and B. Check Hepatitis B surface antibody to confirm vaccine response after 3rd dose. For Hepatitis B vaccine nonresponders consider (a) booster, (b) repeat series (perhaps after CD4 count is >200), or double dose series (especially after CD4 count is > 350 cells/uL). Current CDC guidelines for HIV+ persons recommend HBV vaccine for all HIV+ persons at risk (surface antibody negative and surface antigen negative). They recommend vaccination for those only positive for Heb B Core Antibody. Other experts suggest testing core antibody positive patients for HBV DNA and deferring vaccination for patients with detectable HBV viremia. A single lifetime dose of the new combined Tetanus/adult diphtheria/pertussis vaccine (Tdap) when the tetanus booster is due; otherwise Tetanus/adult diphtheria vaccine (dT) every 10 years. Quadravalent HPV vaccine (6/11/16/18) 3 doses at 0,2,and 6 mnths for HIV infected persons aged 9 – 26 who have not previously been vaccinated. Varicella vaccination (2 doses) for susceptible persons with CD4 count > 200. Consider Hepatitis A vaccine 2 doses (0 and 6-12 months) for non immunes and always for Hepatitis C coinfected persons. Consider Zoster vaccination for persons over age 60 with a CD4 count >200 and a history or serologic evidence of prior varicella infection. Consider meningogoccal and Hemophilius B vaccine for likely exposure, splenectomy. Monitoring For persons on antiretroviral therapy: Inquire specifically about medication adherence at every visit and document this. Some useful questions include: Ask how many doses were taken of each drug at each of the last three days. Ask when if any medication doses were missed in the last week or month. Ask when was the last time a dose was missed. Have the patient indicate on a scale of 1-100 what percent of each medication they take. Ask about why missed doses occur, and problem solve with the patient HIV RNA: repeat 4 weeks after starting or changing antiretroviral therapy. Follow every 4-8 weeks until the virus is fully suppressed. When fully suppressed, follow every 3-4 months for 2 years. After 2 years of Page 3 of 5 J Cohn MD 13 July 2014 consistent full viral suppression with CD4 > 300, follow viral load every 6 months. If HIV RNA levels remain >= 200 consistently, monitor every 3 months. CD4 lymphocyte counts (some labs may require a concurrent CBC with differential to provide the CD4 count): For patients with fully suppressed virus for 2 years, adherence with scheduled visits, and a CD4 300-500, monitor CD every 12 months. With full viral suppression for 2 years and CD4 >500,, no CD4 monitoring is required. For patients without consistently suppressed HIV RNA, test every 3-6 months. Repeat test when clinical changes occur including occurance of opportunistic conditions or use of immunosuppressive therapy. Avoid testing during acute infections and inflammatory states and in the weeks following vaccination. Repeat unexpected results before accepting them as accurate. Consider HIV resistance testing with a genotype assay if viral suppression (<50 copies/μL) is not achieved within 4-6 months of therapy, or if a patient with fully suppressed virus develops a viral load ≥500-1000 copies/μL. Routine genotype testing checks for RT and Protease mutations; a separate genotype test for integrase mutations is required if integrase resistance is suspected. Safety Lab Testing: Depending on antiretroviral drug combination and co-morbidities: monitor CBC/differential/platelet count, renal and liver function, fasting glucose and blood lipids, urine analysis at 3-6 month intervals. (For patients with normal values on treatment, fasting lipids can be done annually). Annual Lab Monitoring for everyone: Annual tuberculin skin test or interferon-gamma releasing assay Annual for sexually active persons: Annual serologic test for syphilis Annual screening for gonorrhea and Chlamydia and testing for symptoms or recent unprotected sex exposure (urine, urethral, cervical, anal [for receptive anal intercourse], oral [gonorrhea screen only for oral sex] Consider annual anal Pap smear For Women: Repeat Pap smear (after initial normal Pap smear) in 6 months, and then repeat Pap smear every 12 months Refer women with Epithelial Cell Abnormalities on Pap smear (Atypical Squamous Cells and Squamous Intraepithelial Lesions) for colposcopy Review of contraceptive needs every 6-12 months Baseline bone densitometry in post-menopausal women ≥ 65 years and in younger postmenopausal women who have ≥ 1 risk factor for premature bone loss. Cancer screening guidelines (other than cervical cancer) from American Cancer Society 2014: Breast cancer: Screening annual mammography with clinical breast exam starting at age 40; mammography or other imaging earlier for high risk women. Clinical breast exam every 3 years for women in their 20’s30’s. Colon cancer screening starting at age 50. Options for persons at average risk include annual fecal occult blood testing (FOBT) on 3 consecutive daily specimens, flexible sigmoidoscopy with or without annual FOBT every 5 years, double contrast barium enema every 5 years, or colonoscopy every 10 years Prostate cancer: Discuss pros and cons of PSA testing for men at usual risk at age 50, or at age 45 for African American men and men with a father or brother diagnosed before age 65 with prostate cancer. Annual PSA screening and digital rectal exam for men at average risk starting at age 50; screen men at high risk (African American men or those with a family history) starting at age 45; screen men at very high risk (African American men with a family history) starting at age 40. Page 4 of 5 J Cohn MD 13 July 2014 Here are additional health maintenance interventions from IDSA/HIVMA HIV Primary Care Guidelines 2013 and US PHS Prevention Task Force, 2014: 1. Counseling to reduce alcohol misuse and for tobacco cessation. 2. Screen for depression if treatment is readily available. The US PHS task force considers the evidence insufficient to recommend routine screening for partner abuse, although patients in the HIV clinic may be at higher than average risk 3. Dietary counseling for those with risk of cardiovascular disease or diet-related disease. 4. Annual screen for hypertension and obesity and treat or counsel accordingly. 5. Fasting lipids and fasting glucose or Hb A1C prior to ARVs, within 3 months of starting ARVs, and annually on ARVs. 6. Screen for dyslipidemia in men ≥ age 35 years and women ≥ 45 years. Screen younger persons with coronary risk factors. 7. Screen for osteoporosis in post-menopausal women and men >=50 . 8. Aspirin primary chemoprophylaxis for persons at high risk of coronary artery disease. 9. Annual screening for lung cancer annually in persons 55-80 years of age using low dose chest CT if there is at least a 30 pack year smoking history and smoking continued within past 15 years, in a person with a reasonable life expectancy and ability to undergo lung resection surgery. 10. Screen men 65-75 years old who have ever smoked for abdominal aortic aneurysm with a one time ultrasound; consider selective screening in men of the same age who never smoked. REFERENCES Aberg JA et al, Primary Care Guidelines for the Management of Persons Infected with Human Immunodeficiency Virus: 2013 update by the HIV Medicine Association of the Infectious Disease Society of America. J Infect Dis November 13 2013 Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents HIV-1 infected adults and adolescents. Department of Health and Human Services May 1 2014 www.aidsinfo.nih.gov CDC. Guidelines for the Prevention and Treatment of Opportunistic Infections in HJV-infected Adults and Adolescents. Recommendations from the CDC, NIH, and HIVMA/IDSA. Last Updated May 7 2013. Accessed at www.aidsinfo.nih.gov on 13 July 2014 American Cancer Society. Accessed www.cancer.org 13 July 2014 US Public Health Service. Accessed www.uspreventiveservicestaskforce.org 13 July 2014 Page 5 of 5