Falls are focus of community hospital`s first EBP project
advertisement

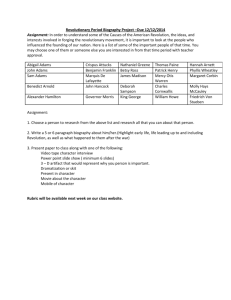
Falls are focus of community hospital’s first EBP project For reasons she can’t explain, Debbie Durant, RN, BSN, has seen a rise in the number of patient falls occurring recently at North Adams (MA) Regional Hospital. “Up until six months ago, our fall rate was pretty flat,” says Durant, director of the medical surgical unit at the 120-bed hospital. “But about six months ago, they began to jump, and we don’t know why. Was it that we weren’t assessing correctly, were we not putting the right interventions in place, or was it that our patient population changed—or a combination? That’s the question that started us down this road.” North Adams had been using what Peg Daly, RN, BS, the hospital’s education specialist, calls a hybrid version of several other falls risk assessments. “It’s not the Morse Falls Scale, not the Hendrick Scale. It’s the North Adams Regional Hospital Scale,” Daly says. It’s been in place for so long that no one remembers it being implemented—or who decided it would be effective for preventing patient falls. But with falls rising steadily and payer pressure on the hospital to eliminate hospitalrelated injuries, Daly says the old method simply wasn’t working anymore. That’s why the hospital turned to its falls committee to research evidence and change how nurses at North Adams assess patients’ risks for falls and how they intervene with at-risk patients. During the next several months, the committee has the following four goals: Decrease falls at North Adams by 10% 12 months after plan implementation Review and revise falls policy and procedures based on evidence-based data Recommend necessary education for staff members Develop ongoing performance improvement monitoring A few extra steps Once the falls problem was identified and brought to the attention of the hospital’s patient safety committee, Daly and Durant formed a falls subcommittee and recruited staff nurses to participate. The committee has representation from inpatient and outpatient areas of the hospital and meets weekly to discuss current practice and published research on the subject. The committee discussed various journal articles and literature found online and evaluated models used by other healthcare organizations. In particular, Daly says, the committee examined the assessment used by Department of Veterans Affairs hospitals and the Morse and Hendrick models used by a handful of neighboring organizations. “We compared risk assessment tools to the tool that we were already using and felt, after looking at everything, our tool was basically a hybrid of several scales,” says Daly. North Adams’ size and its previous success with a hybrid falls prevention model caused the committee to decide that the hybrid model was once again the way to go—and North Adams was the perfect place to test it. “We decided that if we were going to do all this work, we should try to validate its use in our facility,” Daly says, adding that instead of simply copying another organization’s best practice, the hospital could better find the right solution by testing it. “I suggested that we treat this as more of a research project so that we could gather the data and really see if it impacted our fall rate,” she says. The committee started by analyzing its current falls assessment process, including interventions. Up until six months before, the procedure had been effective, and Daly says many nurses believed that with a few simple additions, it could be so again. Beginning in January 2009, North Adams will use a revised model for assessing a patient’s risk and preventing falls based on the research and analysis done by the committee. The model includes: Addition of IV criteria to the assessment tool Institution of primary interventions for every patient who comes to the hospital for care and additional interventions for patients scored at low or high risk for falls Required documentation of interventions and completion of a falls risk assessment every eight hours and with any change in the patient’s condition An increased focus on orienting patients to their surroundings and educating them about falls prevention Increased involvement by hospital ancillary staff members in assessing patients’ likelihood of falling IV precautions When the falls committee started discussing North Adams’ old assessment models, staff nurses immediately identified one major flaw: Patients who were hooked up to IVs were being assessed in the same manner as those who did not have IVs. “When a patient has an IV, it is because of an event or a disease process that requires IV fluids or medications, thus can lead to instability in the patient’s condition and increasing the risk for a fall because they may be hemodynamically unstable,” Daly says. Add North Adams’ cramped layout, IV poles, pumps, and tubing, and other technical equipment to the equation, and you have conditions ripe for patient falls. In the revised falls assessment and prevention model, nurses will make every attempt to ensure patients’ IVs are inserted on a nondominant extremity, allowing patients to have their dominant extremity available to assist with movement, Daly says. Staff members will also place an increased focus on making sure that IV patient rooms are uncluttered and work with physicians to reduce the length of time patients undergo IV therapy when possible. Assessment for all Under the revised hybrid model, every patient that comes to North Adams will undergo a falls assessment every eight hours, including those seeking outpatient care. “Anyone who comes into the hospital, they’re coming in for a reason, not just because they thought it would be a nice vacation spot,” says Daly. “No matter what is wrong with you, we’re going to assess the possibility of you falling.” Under the old model, North Adams assessed all patients for falls risk, but only patients who were deemed high risk had fall interventions put in place. By revising the risk assessment tool, North Adams will now have a mechanism to implement primary interventions for all patients, with additional interventions for those deemed at risk. Documentation required Starting in January, nurses will be required to document not only the falls risk assessment, but also the interventions put in place. This step alone will drastically improve the old falls prevention model used at North Adams. “Staff liked what we were using ... but we couldn’t really quantify or qualify any of it unless we really monitored it during implementation,” Daly says. Now, with documentation requirements in place, the hospital will have a way of knowing which interventions were put in place and whether those interventions are working to prevent falls, Daly says. Documentation will be on paper for the first few months of 2009, but the hospital expects to have an online documentation tool available through its electronic medical record by summer, she says. Patient involvement Like most hospitals, North Adams recognizes that preventing falls isn’t solely the responsibility of the nursing staff—patients and their families must be involved, says Daly. Previously, when patients were admitted at North Adams, nurses would give a quick orientation of the hospital environment, pointing out the bathroom, the nurses’ station, and how to use the call button. But today’s model goes much further, educating patients and their families about precautions that can be taken to avoid falls. Staff members go over these precautions in person, says Daly, but North Adams has also created a one-page flyer that is left in each patient’s room. The flyer includes basic safety information, including a reminder for patients to wear proper footwear and use canes or walkers when getting out of bed and to sound the call bell when needed. This form can be left at the bedside and reviewed with the patient, family, and visitors each time a staff member is at the bedside. Signs are also posted in the room to remind patients to ask for help. “We’ve developed a sign that we’re going to put in every patient room on the wall facing the bed,” Daly says. “It says ‘Call, don’t fall’ in a big font so they can see it, as a reminder to use their call bell when they need to get up.” Ancillary staff involvement At presstime, Daly and Durant were working on the most important and hardest to implement portion of the new falls risk assessment: getting staff members from other hospital departments involved in the prevention of patient falls. If North Adams is to see a reduction in falls, Daly says, more than just the nursing staff will have to be part of the falls risk assessment team. Those working in food service, pharmacy, environmental services, and other departments will have to be trained to observe changes in patient status and situations that could increase the chances of a patient fall. For example, Daly says, the pharmacy currently does a quick assessment of a patient’s medications when they are entered into the electronic medical record, but with the new process, a pharmacist will perform a more careful analysis of the medications to check for potential drug interactions that may cause a patient to become disoriented and fall. “If they’re at high risk for a fall, we want them to look at medications and make sure that the pharmacy review is a little more in-depth,” Daly says. “But we’re still figuring out what that mechanism is. We have to work this out with the pharmacy.” Working among the silos of a typical hospital will be a challenge, Daly and Durant say. “When it comes down to it, patient safety isn’t just the responsibility of nursing,” Durant says, “but all departments.” Source: The Staff Educator, January 2009