Care Plan Pain - Community College of Philadelphia
advertisement

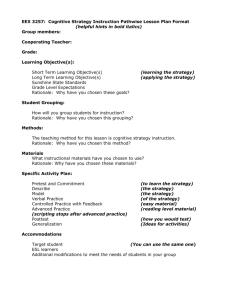
COMMUNITY COLLEGE OF PHILADELPHIA NURSING CARE PLAN Nursing 101, Fall 2006 Student_____Elaine Tagliareni Client initials______JP Age___83 years Defining Characteristics/Behaviors Intensity Pain Scale : “My pain is a 6”. Location (Mark a drawing or describe) Complains of discomfort on left side; aching in her back after PT Onset of Pain Upon arising and after PT : Movement makes it worse”. Duration Discomfort on left side is continuous with some relief after pain medication Nursing Diagnosis____Pain related to immobility and fatigue Contributing Factors Expected Outcomes (with rationales) 1. Physiological Integrity: Pathophysiology (Medical Diagnosis) Stroke on Left Side (CVA) (with rationales) The client will report to the nurse that her pain is a 0 today. Rationale: Impaired physical mobility can result in pain, joint stiffness and contractures (Gulanick, 127) 2. Growth and Development Developmental Norms: Decrease in sensory perception Increased pain threshold Acute pain may not be sharply perceived Mobility will be reduced ( Lecture) Nursing Interventions The nurse will 1. Give the client’s pain medication (Motrin) one hour before morning AM care and PT. Rationale: The peak effect of Ibuprofen is 1-2 hours when given PO. (Davis Drug Guide) The client will verbalize a sense of control over pain experience today to the nurse. 2. Provide client with sleep medication (Restoril) at a time consistent with previous pattern. Rationale: The patient’s experiences with pain may become exaggerated as the result of fatigue (Gulanick, 124)). 3. Walk the client in the hall 1 twice a day. Quality Ache or throbbing in left arm; Soreness in left leg and arm Associated Symptoms: No complaints of restlessness, listlessness No observable diaphoresis. Vital signs remain stable throughout the day and do not increase with pain. 3. Care Environment a. Environment/Hospital Fatigue: Client states “I am exhausted” Rationale: Fatigue heightens the perception of pain Change in routine and anxiety about cold and forgetfulness Rationale: Anxiety often increases pain perception and pain also causes feelings of anxiety . b. Mobility/Immobility Client has limited mobility due to left sided weakness Rationale: Immobility contributes to stiffness of joints, decreased blood flow to body parts which can lead to pain (Lecture) c. Medical/Nursing Treatments Rationale: Muscle atrophy is a common complication that arises from the lack of weight bearing found with immobility (P&P, 1442; Immobility leads to stiffness and muscle pain (Lecture). The nurse will 1. Reinforce the importance of asking for and taking pain medication to keep pain under control. Rationale:One can most effectively deal with pain by preventing it. Early intervention may decrease the total amount of analgesic needed. (Gulanick, 124) 2. Teach client to request that she is wrapped warmly with a hat and three blankets for PT. Rationale: Anxiety tends to reduce pain threshold and limit pain tolerance); decrease in anxiety will increase pain tolerance. Client attends PT daily; ROJM Rationale: The elderly are susceptible to injury and more pain during care activities). d. Medications (Pharmacology) 3. Include Angie in care- 2 Motrin q4 horus for pain planning about managing discomfort at PT and after periods of immobility. Rationale: Action of drug: used for analgesic effect. Inhibits prostaglandin release (Lilley, 734). e. Previous Patterns (if applicable) Client has a history of pain while hospitalized and experienced pain during previous hospitalization Rationale: If a client has experienced pain or is threatened by the anticipation of pain, the pain response is heightened. (Lecture). f. Diagnostic Tests (if applicable) g. Cultural Influences (if applicable) 4. Psychosocial Integrity a. Stressors Client is experiencing stressors: New setting (rehab facility) Pain Anticipation of pain Worry about “catching a cold” Evaluation of Expected Outcomes: Rationale: Involving the family in pain management increases compliance with the treatment regim; adding to the patient’s network of social supports can reduce the burden of suffering with pain. (Gulanick, 129) The client stated that her pain was a 0 today. The client stated that she now feels a greater sense of control over her pain even though she will never be able to fully control her life while in the hospital. 3 Overstimulation of eating with group Worry about Angie at home Concern about final outcome of illness, “Will I ever be cured?” Rationale: Anxiety tends to reduce pain threshold and limit pain tolerance (P&P, 1238 and Lecture) b. Coping Mechanisms Clients usual coping mechanisms are use of usual routines, talking and being with Angie, caring for self. Rationale: When a patient experiences pain in a health care setting such as a hospital, loneliness can be unbearable and coping styles are altered and influence the ability to deal with pain (P&P, 1238). c. Support Systems Angie is primary support person Rationale: An absence of a family or friends can often make the pain experience more stressful (P&P, 1238). 4 COMMUNITY COLLEGE OF PHILADELPHIA NURSING CARE PLAN Nursing 101, Fall 2004 Student________________________________ Client initials____________________ Defining Characteristics/Behaviors Age_______________ Contributing Factors Nursing Diagnosis______________________________________ Expected Outcomes (with rationales) 1. Physiological Integrity: Pathophysiology (Medical Diagnosis) Nursing Interventions (with rationales) The client will…….. The nurse will………… The client will…….. The nurse will………… 2. Growth and Development 5 3. Care Environment a. Environment/Hospital Evaluation of Expected Outcomes: b. Mobility/Immobility c. Medical/Nursing Treatments d. Medications (Pharmacology) e. Previous Patterns (if applicable) f. Diagnostic Tests (if applicable) g. Cultural Influences (if applicable) 4. Psychosocial Integrity a. Stressors 6 b. Coping Mechanisms c. Support Systems 7