Welcome to the Healthy Families Update from CWTAC
advertisement

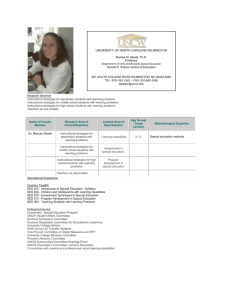
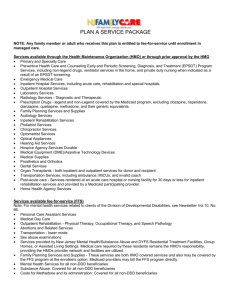
california institute for mental health Healthy Families Update Welcome to the Healthy Families Update from CIMH! Our Goal: Provide brief, practical updates on HF Mental Health issues for County Administrators, Health Plan Liaisons, and Mental Health Workers. We hope this will improve communication and expand access to the HF Mental Health benefit. Please share this newsletter with Access Teams, mental health staff, and others! This Month’s Topic: A Summary of Responsibilities—Who is Supposed to do What, When for HF members with mental health needs? Upcoming Topics: Billing Questions, Hospitalization…and more. Other Great Sources of Information on HF Mental Health This winter, CIMH will produce a Healthy Families Reference Guide, containing key policies, contact information, and a way to store issues of this newsletter. In the meantime, you can turn to the following: HF Mental Health Benefits in a Nutshell Healthy Families mental health coverage includes the diagnosis and medically necessary treatment of serious mental illness. Benefits are split into two parts: Basic and SED. Basic Benefits (Health Plans Provide) Outpatient services (20 visits/year w/$5 copay), mental health inpatient hospital services (up to 30 days/year, no charge), alcohol and drug abuse inpatient as medically appropriate to remove toxic substances from the system (no charge), alcohol and drug outpatient (20 visits/year w/$5 copay), and prescription drugs. Seriously Emotionally Disturbed (SED) Benefit (Counties Provide) Supplemental mental health benefit for children with SED that is managed by County Mental Health Plans. Children who are determined by the Department to be SED will be provided the full range of medically necessary services to the extent resources are available. The CIMH Healthy Families SED benefit Brochure: http://www.cimh.org/healthy_families.html Overall program information, including lists of certified application assistants who assist families with the application: http://healthyfamilies.ca.gov/ In This Issue: Welcome! HF Mental Health benefits at a glance County MH Administrators: Overview of county responsibilities Health Plans: Overview of plan responsibilities County MH Staff: Healthy Families Basics Everyone: Healthy Families Enrollment Data General: 1 3 4 5 6 Healthy Families Update January 2001 PAGE 1 CIMH Healthy Families Update Defining “Seriously Emotionally Disturbed” In CIMH’s work around the State, we have learned that some confusion exists regarding the proper definition of “Seriously Emotionally Disturbed (SED)” for purposes of the Healthy Families Mental Health benefit. Definitions of SED differ in different systems and for different funding sources. For Healthy Families enrollees, according to WIC 5600.3, in order to meet the criteria for “seriously emotionally disturbed,” a youth must: Have a DSM-IV Diagnosis, excepting V-codes, substance abuse, or developmental disorders and meet at least one of the following criteria: A. As a result of the mental disorder have severe impairment in two of the following areas: self-care, school functioning, family relationships, or ability to function in the community and either of the following occur: Wait! There’s More! On the following pages you will find three sections that will always appear in this newsletter: County Mental Health Administrators Healthy Families Update Health Plans Healthy Families Update County Mental Health Staff Healthy Families Update This month, we focus on responsibilities under Healthy Families. Suggestions? Questions? Contact us with your suggestions for future newsletter topics, comments on this issue, and questions: email Mary Jane Alumbaugh, Ph.D., at mjalumbaugh@cimh.org. The child is at risk of removal from home or has already been removed from the home. The mental disorder and impairments have been present for more than six months or are likely to continue for more than one year without treatment. B. The child displays one of the following: psychotic features, risk of suicide, or risk of violence due to a mental disorder. C. The child meets special education requirements. Healthy Families Update January 2001 PAGE 2 County MH Admin County Responsibilities Under Healthy Families According to the Memorandum of Understanding (MOU), promulgated by the Managed Risk Medical Insurance Board (MRMIB) and signed by most counties and Health Plans, both Counties and Health Plans have a number of specific responsibilities under Healthy Families. This page summarizes the MOU’s content regarding County responsibilities in the areas of assessment, benefits, coordination, and medical necessity. Assessment The County will assess or arrange to assess children referred for a mental health evaluation and will determine if the child meets SED criteria (WIC Code 5600.3). Evaluations will be performed within five (5) days of referral if the child is receiving inpatient services. CIMH Healthy Families Update Benefits Children accepted for treatment by the County Mental Health Department as SED will be eligible for: Medically necessary outpatient services for treatment of the child’s serious emotional disturbance. Medically necessary outpatient medication and laboratory services that are part of the child’s outpatient treatment plan with the Mental Health Department. Inpatient services including professional and ancillary services associated with inpatient days, when Plan inpatient benefits are exhausted and such services meet Short-Doyle Medi-Cal medical necessity. Coordination The County Mental Health Department will: Evaluations will be performed within thirty (30) days in all other cases (providing all necessary information is included in the referral). Consult with the plan as they determine when non-inpatient care may be substituted for inpatient benefits to shorten inpatient stays. Counties will be liable for inpatient costs incurred by the Plan when the child’s discharge is delayed by County failure to meet these timelines. When the County Mental Health Department is responsible for inpatient care, it will utilize the Short-Doyle Medi-Cal medical necessity and emergency admission to an acute psychiatric hospital. The County shall develop a procedure for identifying Plan beneficiaries already receiving SED services. Medical Necessity Healthy Families Update January 2001 PAGE 3 Health Plans Health Plan Responsibilities for Children with SED Under Healthy Families Health Plans, like counties, have clearly defined responsibilities as a result of the MOU in the areas of assessment, benefits, coordination, and medical necessity. Assessment The Health Plan will obtain or arrange to obtain a mental health screening and assessment of any enrollee they suspect may have a serious emotional disturbance. The Health Plan will then refer the child to the County Mental Health Department for evaluation if the Health Plan has reason to believe the following: A. The child has a serious emotional disturbance as defined in WIC 5600.3. B. The disorder cannot be effectively managed with relatively short-term therapy. Benefits As noted on Page 1, Health Plans provide basic mental health benefits to all children. However, they also retain responsibility for certain benefits to children with SED. According to the MOU, children [with SED] being treated by the County Mental Health Department will retain eligibility for Plan benefits including: CIMH Healthy Families Update Coordination and Medical Necessity The referral for an evaluation for SED to County Mental Health shall be in writing and may include a locally agreed upon referral packet that includes material the Health Plan and the County Mental Health Department believe will facilitate timely, thorough referrals. The Health Plan may identify procedures for referral from primary care physicians. The Health Plan will provide inpatient services within the following parameters. The Health Plan will: A. When considering admission of SED children to an inpatient facility utilize inpatient benefit approval criteria that are the same as Health Plan processes for inpatient benefit approval for non-SED/HF children. B. Determine with the County Mental Health Department how ongoing care for SED children can be coordinated when inpatient services are required. C. The Health Plan, in consultation with the County Mental Health Department, will determine when non-inpatient care may be substituted for inpatient benefits to shorten inpatient stays. A. Inpatient treatment of an acute phase of a mental health condition in a participating hospital for up to 30 days per benefit year as per benefits under this Health Plan, including professional and ancillary benefits associated with inpatient days. Healthy Families Update January 2001 PAGE 4 County MH Staff What is Healthy Families? The Healthy Families Program is a state and federally funded health coverage program for children with family incomes above the level eligible for no cost Medi-Cal and below 250% of the federal income guidelines ($35,376 for a family of three). Healthy Families provides health (including mental health), dental, and vision benefits. Healthy Families members pay a small premium (which can also be paid by other community organizations) and some copayments. Healthy Families is a key part of California’s effort to reduce the number of children without health insurance. How Does Healthy Families Affect Mental Health Services? Children enrolled in Healthy Families can get basic mental health services through their Healthy Families Health Plan. However, if they have SED, they will be referred to the County Mental Health Department. Sometimes, a child and family will enter the County system for services and the County will determine that they are already enrolled in Healthy Families. Counties can then bill for these services through the SD/MC claims processing. What Rules Affect Healthy Families? CIMH Healthy Families Update There are also certain forms and protocols for coordination designed to ensure continuity of care. Contact your County’s Healthy Families Liaison or Children’s System of Care (CSOC) Coordinator for additional information. Many of the procedures and rules affecting Healthy Families Mental Health will be summarized in the upcoming Healthy Families Mental Health Reference Guide from CIMH. How Can I Tell if Someone is Enrolled in Healthy Families? Your County Mental Health Department’s administrative staff may have noted their Healthy Families Program enrollment when they first came to the County for service. They may have a Card from their Health Plan. Some cards will say “Healthy Families,” but others will not. If someone presents a Health Plan card, make sure to check carefully to determine if they are in the Healthy Families Program. (An upcoming issue of this newsletter will review Healthy Families Health Plan cards for easier identification.) They may have been referred by their Health Plan for SED services. If you get a referral, contact your Healthy Families Liaison or CSOC coordinator for information regarding the proper referral forms. Healthy Families members have specific rights to services. If your County Mental Health Department receives a referral from a Health Plan, the County must evaluate the child within 5 days if he or she is hospitalized, and within 30 days otherwise. Healthy Families Update January 2001 PAGE 5 Everyone CIMH Healthy Families Update What’s Next in This Newsletter? How Can I Refer an Uninsured Family to the Healthy Families Program? In upcoming issues, this newsletter will provide additional detail for mental health staff on: The Healthy Families Program can provide important benefits to uninsured families, including health, dental, and vision coverage. Your County Mental Health Department’s intake office may have people trained to assist clients who wish to enroll in Healthy Families. If they do not, a wide range of community agencies in each County also can assist people with the Healthy Families enrollment process. Healthy Families referral procedures; How to identify a Healthy Families enrollment card; Explaining Healthy Families benefits to clients… …and more. If you would like to suggest a topic, please email: mjalumbaugh@cimh.org. For an up-to-date list in your County, you can visit the Healthy Families web site at: http://healthyfamilies.ca.gov/ SED Healthy Family Plan (9H) and Medi-Cal Bridge to HFP (7X) Approved Claims By County Fiscal Year 1999-2000 HFP Aid Code Statewide Alameda Butte Contra Costa El Dorado Fresno Humboldt Kern Kings Los Angeles Marin Mariposa Mendocino Nevada Orange Riverside Sacramento San Bernardino San Diego San Francisco San Joaquin San Luis Obispo Santa Barbara Santa Clara Santa Cruz Sonoma Stanislaus Tulare Sutter/Yuba Medi-Cal Bridge to HFP Approved Amount 1,554,795 8,746 88,022 1,336 13,901 Unduplicated Clients 644 1 29 1 9 3,733 256,421 2 89 88,076 98 4,577 4 6,547 7 111,868 183,753 120,247 49 49 70 114,860 34,559 2,692 198,388 68 34 2 37 115,202 108,359 36,697 56,697 115 15 22 27 30 1 Approved Amount 57,623 447 3,024 5,306 Unduplicated Clients 94 1 1 5 74 2 94 3,407 467 1 8 1 1,219 1 14,959 557 383 792 2,769 907 740 13,459 2,552 1,526 1,164 30 3 2 2 8 3 3 5 2 3 4 3,374 402 6 3 Healthy Families Update January 2001 PAGE 6