nevirapine SPC
advertisement

Nevirapine SPC Recommended Text
version 2.0
Recommended Text Nevirapine
SUMMARY OF PRODUCT CHARACTERISTICS
Wordings between <> to be selected or deleted as appropriate;
Wordings between {} provide advice or example text.
1.
NAME OF THE MEDICINAL PRODUCT
<product name> <dose> <pharmaceutical form>
{Example: Nevirapine 200 mg tablets}
2.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each <pharmaceutical form> contains <dose> of <product name>
{Example: Each tablet contains 150 mg nevirapine anhydrate.}
For excipients see 6.1
3.
PHARMACEUTICAL FORM
<Hard capsule> or
<Tablet> or
<Film-coated tablet> or
<Powder for oral solution> or
<Oral suspension>
{Include here a description of the visual appearance of the product pharmaceutical form as marketed.
Example: The tablets are white, diamond-shaped and marked with ‘XX’ in black.}
November 2006
WHO Prequalification of Medicines Programme
Page 1 of 8
Nevirapine SPC Recommended Text
4.
CLINICAL PARTICULARS
4.1
Therapeutic indications
version 2.0
Nevirapine is indicated for the treatment of HIV-1 infection in combination with other antiretroviral
agents.
4.2
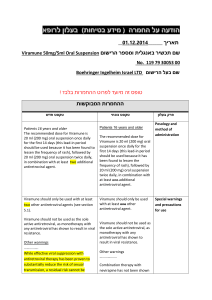
Posology and method of administration
Oral use.
Therapy should be prescribed by a physician experienced in the management of HIV-1 infection.
Patients 16 years and older:
200 mg once daily for the first 14 days followed by one 200 mg tablet twice daily.
<Pediatric patients 2 month to 16 years:> <a different formulation e.g. solution must be chosen>.
{text below not applicable for fixed dose preparations}
<4 mg/kg once daily for the first 14 days followed by 7 mg/kg twice daily thereafter. The total daily
dose should not exceed 400 mg for any patient.>
The lead-in period allows for induction of drug-metabolizing hepatic enzymes and has been found to
lessen the frequency of rash.
Nevirapine may be taken with or without food.
Liver Disease:
Nevirapine should not be used in patients with severe liver disease (e.g. Child-Pugh Classification
Score >
or pre-treatment liver enzymes > 5 upper limit of normal (ULN).
Renal Impairment:
In subjects with end-stage renal disease requiring haemodialysis an additional 200 mg dose of
nevirapine following each haemodialysis treatment should be given to offset the effects of dialysis on
nevirapine clearance. Patients with creatinine clearance ≥ 20 ml/min do not require an adjustment in
nevirapine dosing.
4.3
Contraindications
Nevirapine is contraindicated in patients with clinically significant hypersensitivity to nevirapine or to
any of the components contained in the formulation.
Nevirapine is contraindicated in patients with severe hepatic impairment (e.g. Child-Pugh
Classification Score > 7).
Nevirapine must not be re-administered to patients who have required permanent discontinuation for
severe rash, hypersensitivity reactions or liver toxicity due to nevirapine.
Nevirapine should not be used for post-exposure prophylaxis in HIV-1 negative individuals.
4.4
Special warnings and special precautions for use
Skin reactions
Rash is a common adverse reaction to nevirapine. Cases are usually mild to moderate but severe and
life-threatening skin reactions including cases of Stevens-Johnson syndrome and toxic epidermal
necrolysis have occurred (1-3). These have mainly occurred during the initial 6 weeks of therapy, but
may occur up to 18 weeks after start of nevirapine. Patients should be warned to report symptoms of a
hypersensitivity reaction immediately (e.g. fever, rash, arthralgias or myalgias). Nevirapine must be
permanently discontinued in any patient experiencing severe rash or a rash accompanied by systemic
symptoms.
November 2006
WHO Prequalification of Medicines Programme
Page 2 of 8
Nevirapine SPC Recommended Text
version 2.0
Prednisone (4-6) or antihistamine (cetrizine) (7, 8) does not decrease the incidence of nevirapineassociated rash.
Factors associated with nevirapine-associated rash are higher baseline CD4 count, higher baseline HIV
RNA level, female sex, higher age and higher nevirapine concentration (4, 6, 7, 9). Once daily dosing
(400 mg) is associated with a higher rate of rash than twice daily dosing (10, 11).
Patients with rash should be assessed for liver toxicity.
Nevirapine must not be restarted following severe skin reactions.
If fever or other features of hypersensitivity develop during the 200 mg dose-induction period, the
dose should not be increased to 200 mg twice daily at 14 days unless all features of hypersensitivity
have resolved – patients should be advised that recurrence of these symptoms is likely at the increased
dose.
Liver disease
Severe and life-threatening liver toxicity, including fatal fulminant hepatitis, has occurred in patients
treated with nevirapine. This has mainly occurred during the initial 6 weeks of therapy but may occur
up to 18 weeks after start of nevirapine. Symptoms are a hypersensitivity reaction that may be
accompanied by rash, eosinophilia and systemic symptoms (fever, rash, arthralgias or myalgias).
Factors associated with nevirapine-associated liver toxicity are female sex, higher baseline CD4
counts, higher baseline levels of alanine aminotransferase, hepatitis C co-infection and alcohol abuse
(12-15). Women with CD4 cell counts >250 cells/mm3 had a 12-fold higher risk of symptomatic liver
toxicity compared to women with CD4 counts <250 cells/mm3. A 5-fold increased risk was observed
in men with CD4 counts > 400 cells/mm3.
Monitoring of liver transaminases should be performed if the patient experiences signs or symptoms
(e.g. anorexia, nausea, jaundice, bilirubinuria, acholic stools, hepatomegaly or liver tenderness)
suggestive of liver toxicity.
Hepatic laboratory abnormalities are more frequent with once daily dosing (400 mg) than with twice
daily dosing (10).
Patients developing signs or symptoms of liver toxicity and/or hypersensitivity should promptly seek
medical evaluation. Nevirapine must be permanently discontinued in any patient experiencing severe
liver toxicity.
Discontinuation and reintroduction of nevirapine.
Because nevirapine is an inducer of the drug-metabolizing hepatic enzymes, administration of full
therapeutic doses of nevirapine without a two-week, low-dose escalation phase will result in excess
plasma drug levels and potentially increase the risk for toxicity. Therefore, in a patient who has
interrupted treatment with nevirapine for more than two weeks and is to be restarted later, nevirapine
should be reintroduced with a dose escalation period of 200 mg once daily for 14 days, then a 200 mg
twice-daily regimen.
Perinatal Transmission
Single-dose use of nevirapine leads to a high rate of nevirapine resistance (16).
Post-exposure prophylaxis (PEP)
Serious liver toxicity, including liver failure requiring transplantation, has been reported in HIV-1
uninfected individuals receiving nevirapine in the setting of PEP (17, 18).
4.5
Interaction with other medicinal products and other forms of interaction
Nevirapine is a mild to moderate inducer of the hepatic enzyme CYP3A; therefore, it is possible that
co-administration of nevirapine with protease inhibitors may result in an alteration in the plasma
concentration of either agent (19-21).
Nevirapine decreases plasma concentrations of methadone (22). Methadone-maintained patients
beginning nevirapine therapy should be assessed for evidence of withdrawal and methadone dose
should be adjusted accordingly.
November 2006
WHO Prequalification of Medicines Programme
Page 3 of 8
Nevirapine SPC Recommended Text
version 2.0
Ketoconazole levels are reduced >60% and is therefore not recommended to be used with nevirapine.
Rifampicin may significantly decrease levels of nevirapine and is not recommended used together
(23).
Exposure to nevirapine can be reduced by concomitant use of the herbal preparation St John's Wort
(Hypericum perforatum). Herbal preparations containing St John’s Wort must therefore not be
combined with nevirapine.
4.6
Pregnancy and lactation
Pregnancy: Nevirapine is assigned FDA Pregnancy Category C status, i.e. risk cannot be ruled out. No
increased risk of birth defects have been reported for nevirapine (www.apregistry.com).
Nursing Mothers: Nevirapine crosses the placenta and is found in breast milk of lactating mothers
(24). Because of the potential for postnatal HIV transmission and adverse effects caused by nevirapine
in nursing infants, HIV-infected mothers should be instructed not to breast-feed.
4.7
Effects on ability to drive and use machines
No studies on the effects on the ability to drive and use machines have been performed.
4.8
Undesirable effects
The following adverse events have been reported in controlled clinical trials and case series during
treatment of HIV-1 infection with nevirapine.
The adverse events considered at least possibly related to the treatment are listed below by body
system, organ class and absolute frequency. Frequencies are defined as very common (>1/10),
common (>1/100, <1/10), uncommon (>1/1000, <1/100), rare (>1/10,000, <1/1000), very rare
(<1/10,000).
Blood and lymphatic systems disorders
Common: Neutropenia (25).
Immune system disorders
Common: Allergic reactions
Rare: Hypersensitivity syndrome.
Nervous system disorders
Common: Headache (26-28).
Gastrointestinal disorders
Common: Nausea (26).
Hepatobiliary disorders
Common: Liver transaminase abnormalities (25-27, 29, 30).
Uncommon: Jaundice.
Rare: Liver failure.
Skin and subcutaneous tissue disorders
Common: Rash (25, 26, 28-30).
Uncommon: Stevens Johnson syndrome.
Rare: Toxic epidermal necrolysis.
General disorders:
Uncommon: Fatigue and fever (26, 27).
4.9
Overdose
November 2006
WHO Prequalification of Medicines Programme
Page 4 of 8
Nevirapine SPC Recommended Text
version 2.0
There is no known antidote for nevirapine over dose. Cases of nevirapine overdose at doses ranging
from 800 to 6000 mg per day for up to 15 days have been reported. Patients have experienced oedema,
erythema nodosum, fatigue, fever, headache, insomnia, nausea, pulmonary infiltrates, rash, vertigo,
vomiting, increase in transaminases and weight decrease. All of these effects subsided following
discontinuation of nevirapine.
5.
PHARMACOLOGICAL PROPERTIES
5.1
Pharmacodynamic properties
Pharmacotherapeutic group: {group}, ATC Code {code}
Example: Antiretroviral, ATC code: J05A G01
Nevirapine is a non-nucleoside reverse transcriptase inhibitor (NNRTI) of HIV-1. Nevirapine binds
directly to reverse transcriptase and blocks the RNA-dependent and DNA-dependent DNA polymerase
activities by inducing a conformational change that causes a disruption of the enzyme's catalytic site.
The activity of nevirapine does not compete with template or nucleoside triphosphates. HIV-2 reverse
transcriptase and eukaryotic DNA polymerases (such as human DNA polymerases α, β, γ, or δ) are not
inhibited by nevirapine.
Clinical efficacy:
Nevirapine has been investigated in several randomized, prospective clinical trials combined with
other antiretroviral drugs (10, 25, 29, 31-34). These studies have demonstrated significant decreases in
plasma HIV RNA and increases in CD4 cell counts when used in combination with other nucleoside
analogue(s) and/or a Protease Inhibitor. In recent studies by intention-to-treat analysis > 70% of
subjects have achieved plasma HIV RNA < 50 copies/ml after 48 weeks of combination antiretroviral
treatment (10).
HIV-1 resistance to nevirapine involves the development of mutations in the reverse transcriptase gene
at positions 100, 103, 106, 108, 181, 188 and 190 (www.iasusa.org). The K103N or Y188L mutation
alone prevents the clinical utility of nevirapine. The V106M mutation is more common in HIV-1
subtype C than subtype B and confers cross-resistance to nevirapine and efavirenz.
Rapid emergence of resistance to NNRTIs, including nevirapine, is likely to occur in case of
virological failure.
Patients who are infected with known nevirapine-resistant HIV or patients who have previously
experienced virological failure on a nevirapine- or efavirenz-containing regimen may not respond
sufficiently to further treatment with a combination regimen containing nevirapine or efavirenz.
Perinatal Transmission
Nevirapine, given to pregnant mothers in labour who have not received standard combination
antiretroviral therapy during pregnancy, prevents vertical transmission of HIV-1 infection. A single
dose of 200 mg of nevirapine given at the onset of labour to the mother and 2 mg/kg given to the
infant within 72 hours of birth is highly effective in reducing mother-to-child transmission of HIV-1
(35-37). No benefit from additional intra-partum / newborn nevirapine was demonstrated when
women received prenatal care and antenatal ART, and elective caesarean section was made available
(38).
Single-dose use of nevirapine leads to a high rate of nevirapine resistance (16).
5.2
Pharmacokinetic properties
Absorption and Bioavailability:
Nevirapine is rapidly absorbed following oral administration. Bioavailability is > 90%. Peak plasma
concentrations of 2.0 µg/ml occur within 4 hours after dosing. At a therapeutic dose of 200 mg twice
daily, mean steady-state Cmax and Cmin of nevirapine in plasma were 5.7 µg/ml and 3.7 µg/ml,
respectively. The area under the curve (AUC) is 109 µg.h/ml.
November 2006
WHO Prequalification of Medicines Programme
Page 5 of 8
Nevirapine SPC Recommended Text
version 2.0
Distribution
The estimated volume of distribution is 1.2 l/kg. The observed half-life is 25 to 30 hours following
multiple dosing. Protein binding is approximately 60%.
Metabolism / Elimination
Nevirapine is actively biotransformed primarily via cytochrome P450 isozyme CYP3A. Cytochrome
P450 metabolism, glucuronide conjugation and urinary excretion of glucuronidated metabolites
represent the primary route of nevirapine elimination in humans. Less than 5% is excreted through the
kidneys.
5.3
Preclinical safety data
Preclinical data revealed no special hazard for humans other than those observed in clinical studies
based on conventional studies of safety, pharmacology, repeated dose toxicity, and genotoxicity. In
reproductive toxicology studies, evidence of impaired fertility was seen in rats. In carcinogenicity
studies, nevirapine induced hepatic tumours in rats and mice. In rats these findings are most likely
related to nevirapine being a strong inducer of liver enzymes, and not due to a genotoxic mode of
action. The mechanism of tumours in mice is not yet clarified and therefore their relevance in humans
remains to be determined.
6.
PHARMACEUTICAL PARTICULARS
6.1
List of excipients
{Product specific}
6.2
Incompatibilities
<Not applicable.>
6.3
Shelf life
{Product specific}
6.4
Special precautions for storage
{Product specific}
6.5
Nature and contents of container
{Product specific}
6.6
Instructions for use and handling and disposal
<No special requirements.>
7.
<SUPPLIER>
{Product specific}
8.
<WHO REFERENCE NUMBER (PREQUALIFICATION PROGRAMME)>
{Product specific}
November 2006
WHO Prequalification of Medicines Programme
Page 6 of 8
Nevirapine SPC Recommended Text
9.
version 2.0
DATE OF <FIRST PREQUALIFICATION> <FIRST AUTHORISATION>
<RENEWAL> OF THE <PREQUALIFICATION><AUTHORISATION>
{Product specific}
10.
DATE OF REVISION OF THE TEXT
{month year}
November 2006
WHO Prequalification of Medicines Programme
Page 7 of 8
Nevirapine SPC Recommended Text
version 2.0
Reference List
1. K. J. Warren, D. E. Boxwell, N. Y. Kim, B. A. Drolet, Lancet 351, 567 (1998).
2. J. P. Fagot et al., AIDS 15, 1843 (2001).
3. F. Bonnet et al., Clin. Infect. Dis. 35, 1231 (2002).
4. F. W. Wit et al., AIDS 15, 2423 (2001).
5. H. Knobel et al., J. Acquir. Immune. Defic. Syndr. 28, 14 (2001).
6. J. S. Montaner et al., J. Acquir. Immune. Defic. Syndr. 33, 41 (2003).
7. H. Knobel et al., J. Acquir. Immune. Defic. Syndr. 37, 1276 (2004).
8. O. Launay et al., Clin. Infect. Dis. 38, e66 (2004).
9. M. M. de Maat et al., Eur. J. Clin. Pharmacol. 59, 457 (2003).
10. F. van Leth et al., Lancet 363, 1253 (2004).
11. J. Ananworanich et al., AIDS 19, 185 (2005).
12. E. Martinez et al., AIDS 15, 1261 (2001).
13. D. Gonzalez de Requena, M. Nunez, I. Jimenez-Nacher, V. Soriano, AIDS 16, 290 (2002).
14. L. Martin-Carbonero, M. Nunez, J. Gonzalez-Lahoz, V. Soriano, HIV. Clin. Trials 4, 115 (2003).
15. I. Sanne et al., J. Infect. Dis. 191, 825 (2005).
16. S. Palmer et al., Proc. Natl. Acad. Sci. U. S. A 103, 7094 (2006).
17. S. Johnson, J. Chan, C. L. Bennett, Ann. Intern. Med. 137, 146 (2002).
18. S. M. Patel et al., J. Acquir. Immune. Defic. Syndr. 35, 120 (2004).
19. R. L. Murphy et al., J. Infect. Dis. 179, 1116 (1999).
20. C. Solas et al., Br. J. Clin. Pharmacol. 57, 436 (2004).
21. D. M. Burger, J. M. Prins, M. E. van der Ende, R. E. Aarnoutse, J. Acquir. Immune. Defic. Syndr.
35, 97 (2004).
22. S. M. Clarke et al., Clin. Infect. Dis. 33, 1595 (2001).
23. E. Ribera et al., J. Acquir. Immune. Defic. Syndr. 28, 450 (2001).
24. M. Mirochnick et al., J. Infect. Dis. 178, 368 (1998).
25. D. Podzamczer et al., Antivir. Ther. 7, 81 (2002).
26. D. Havlir et al., J. Infect. Dis. 171, 537 (1995).
27. S. H. Cheeseman et al., J. Acquir. Immune. Defic. Syndr. Hum. Retrovirol. 8, 141 (1995).
28. A. Carr et al., AIDS 10, 635 (1996).
29. R. T. D'Aquila et al., Ann. Intern. Med. 124, 1019 (1996).
30. J. S. Montaner et al., JAMA 279, 930 (1998).
31. J. S. Montaner et al., JAMA 279, 930 (1998).
32. R. van Leeuwen et al., AIDS 17, 987 (2003).
33. G. K. Robbins et al., N. Engl. J. Med. 349, 2293 (2003).
34. R. W. Shafer et al., N. Engl. J. Med. 349, 2304 (2003).
35. J. B. Jackson et al., Lancet 362, 859 (2003).
36. T. E. Taha et al., JAMA 292, 202 (2004).
37. M. Lallemant et al., N. Engl. J. Med. 351, 217 (2004).
38. A. Dorenbaum et al., JAMA 288, 189 (2002).
November 2006
WHO Prequalification of Medicines Programme
Page 8 of 8