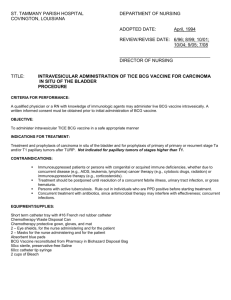
1: J Urol
advertisement

1: J Urol. 2004 Feb;171(2 Pt 1):561-9. Neoadjuvant chemotherapy for transitional cell carcinoma of the bladder: a systematic review and meta-analysis. Winquist E, Kirchner TS, Segal R, Chin J, Lukka H; Genitourinary Cancer Disease Site Group, Cancer Care Ontario Program in Evidence-based Care Practice Guidelines Initiative. London Regional Cancer Centre, Ontario, Canada. eric.winquist@lrcc.on.ca PURPOSE: Despite local therapy most patients with muscle invasive transitional cell carcinoma (TCC) of the bladder die of systemic relapse, indicating a need for effective adjunctive systemic treatment. We determined whether neoadjuvant chemotherapy improved overall survival. MATERIALS AND METHODS: A systematic review and meta-analysis were performed of all known randomized controlled trials (RCTs) of neoadjuvant chemotherapy for stages II and III TCC conducted between 1984 and 2002. RESULTS: A total of 16 eligible RCTs (3,315 patients) were identified. Of these trials 11 (2,605 patients) provided data suitable for a meta-analysis of overall survival and the pooled HR was 0.90 (95% CI 0.82 to 0.99, p = 0.02). Eight trials used cisplatin based combination chemotherapy and the pooled HR was 0.87 (95% CI 0.78 to 0.96, p = 0.006), consistent with an absolute overall survival benefit of 6.5% (95% CI 2 to 11%) from 50% to 56.5%. Reported progression-free survival data were insufficient for meta-analysis but they appeared concordant with overall survival results. Mortality due to combination chemotherapy was 1.1%. A major pathological response was associated with improved overall survival in 4 trials.CONCLUSIONS Neoadjuvant cisplatin based chemotherapy improves overall survival in muscle invasive TCC. The size of the effect is modest and combination chemotherapy can be administered safely without adverse outcomes resulting in delayed local therapy. An optimal chemotherapy regimen was not identified and newer regimens have not been tested in RCTs in this setting. Further efforts to identify the patients most likely to benefit from neoadjuvant therapy are necessary to optimize its use. Publication Types: Meta-Analysis Review Review, Academic PMID: 14713760 [PubMed] 2: Am J Clin Oncol. 2003 Aug;26(4):402-7. Impact of intravesical chemotherapy versus BCG immunotherapy on recurrence of superficial transitional cell carcinoma of the bladder: metaanalytic reevaluation. Huncharek M, Kupelnick B. Division of Radiation Oncology, Department of Clinical Oncology, Marshfield Clinic Cancer Center, Wisconsin, USA. Bacille Calmette-Guerin (BCG) immunotherapy is currently considered the most effective agent in the management of superficial bladder cancer. Prior work suggests that the efficacy of intravesical chemotherapy in preventing tumor recurrence may be greater than previously suggested. This latter finding, therefore, brings into question the currently perceived superiority of BCG treatment for this disease. A metaanalysis was performed to rigorously examine existing data relevant to this relationship and to quantify the relative efficacy of both treatment modalities on tumor recurrence. A prospective protocol outlining the above-noted metaanalysis was initially developed followed by a thorough search of the existing published literature using strict eligibility criteria. Nine randomized trials were found that met protocol specifications. These reports contained data on 2,261 patients that were statistically combined using a fixed effects model (Peto). The outcome of interest was the proportion of patients with recurrence at 1, 2, and 3 years following intravesical therapy (i.e., a summary odds ratio, ORp). Combining all nine trials using 1-year recurrence as the endpoint demonstrated significant statistical heterogeneity, although the ORp favored BCG over intravesical chemotherapy (0.89 [0.74-1.07]). This precluded statistical pooling of the data and sensitivity analyses were performed to determine the source of heterogeneity. These tests showed that the prior chemotherapy treatment in a large number of the randomized trials biased study results in favor of the BCG arms. Once the data were stratified on presence or absence of prior drug treatment, intravesical chemotherapy reduced 1-, 2-, and 3-year recurrence by 21% to 82% versus BCG, depending on the endpoint of interest. The available data suggest that clinical trials directly comparing intravesical BCG to intravesical chemotherapy must stratify on the presence or absence of prior chemotherapy. Recurrences following prior intravesical chemotherapy appear less responsive to drug therapy than those in chemotherapy-naive patients. The currently perceived superiority of BCG therapy may therefore be an artifact of this phenomenon, since most randomized trials include chemotherapy failures in their chemotherapy treatment arms. Publication Types: Meta-Analysis PMID: 12902895 [PubMed] 3: Lancet. 2003 Jun 7;361(9373):1927-34. Comment in: Lancet. 2003 Jun 7;361(9373):1922-3. Neoadjuvant chemotherapy in invasive bladder cancer: a systematic review and meta-analysis. Advanced Bladder Cancer Meta-analysis Collaboration. BACKGROUND: Controversy exists as to whether neoadjuvant chemotherapy improves survival in patients with invasive bladder cancer, despite randomised controlled trials of more than 3000 patients. We undertook a systematic review and meta-analysis to assess the effect of such treatment on survival in patients with this disease. METHODS: We analysed updated data for 2688 individual patients from ten available randomised trials. FINDINGS: Platinum-based combination chemotherapy showed a significant benefit to overall survival (combined hazard ratio [HR] 0.87 [95% CI 0.78-0.98, p=0.016]; 13% reduction in risk of death; 5% absolute benefit at 5 years [1-7]; overall survival increased from 45% to 50%). This effect was observed irrespective of the type of local treatment, and did not vary between subgroups of patients. The HR for all trials, including those using single-agent cisplatin, tended to favour neoadjuvant chemotherapy (HR=0.91, 95% CI 0.83-1.01) although this tendency was not significant (p=0.084). Although platinum based combination chemotherapy was beneficial, there was no evidence to support the use of single-agent platinum; indeed, there was a significant difference in the effect between these groups of trials (p=0.044). INTERPRETATION: This improvement in survival encourages the use of platinum-based combination chemotherapy for patients with invasive bladder cancer. Publication Types: Meta-Analysis Review Review, Academic PMID: 12801735 [PubMed] 4: J Urol. 2003 Jun;169(6):1975-82. Tumor markers in the diagnosis of primary bladder cancer. A systematic review. Glas AS, Roos D, Deutekom M, Zwinderman AH, Bossuyt PM, Kurth KH. Department of Clinical Epidemiology and Biostatistics, Academic Medical Center, OLVG, Amsterdam, The Netherlands. PURPOSE: We systematically reviewed the available evidence, and obtained and compared summary estimates of the sensitivity and specificity of cytology and the urine based markers bladder tumor antigen, BTA stat (Polymedco, Redmond, Washington), BTA TRAK (Polymedco), NMP22 (Matritech, Cambridge, Massachusetts), telomerase and fibrin degradation product in detecting primary bladder cancer. MATERIALS AND METHODS: Studies on the diagnosis of primary bladder cancer published from 1990 through November 2001 in English and German were retrieved from MEDLINE and EMBASE data bases. In our research we included studies that evaluated 1 or more of the markers, used cystoscopy as the reference standard and allowed the construction of a 2 x 2 contingency table for a per patient analysis. The data plus items on study and clinical characteristics were extracted by 2 observers. Sensitivity and specificity for each marker were estimated using a bivariate random effect meta-analysis. A multivariable analysis was performed to explain study variation. RESULTS: A total of 42 studies were included in our review. Only 2 studies were available on fibrin degradation product, hence a meta-analysis was not possible. Cytology had the best specificity at 94% (95% CI: 90% to 96%). This figure was significantly better than that of the other markers except for telomerase (specificity 86% [71% to 94%]). Telomerase had the best sensitivity (75% [71% to 79%]) but it was not significantly better than that of BTA stat (70% [66% to 74%]). Case control designs yielded lower values for sensitivity for the tumor markers cytology, bladder tumor antigen and BTA stat. CONCLUSIONS: Cytology has the best specificity and telomerase the best sensitivity. However, none of the markers studied here is sensitive enough to be recommended for daily routine. Publication Types: Meta-Analysis Review Review, Academic PMID: 12771702 [PubMed] 5: J Urol. 2003 Jan;169(1):90-5. Intravesical bacillus Calmette-Guerin versus mitomycin C for superficial bladder cancer: a formal meta-analysis of comparative studies on recurrence and toxicity. Bohle A, Jocham D, Bock PR. Department of Urology, Medical University of Lubeck, Lubeck, Germany. PURPOSE: We compare the therapeutic efficacy and toxicity of intravesical bacillus Calmette-Guerin (BCG) with mitomycin C on recurrence of stages Ta and T1 bladder carcinoma. MATERIALS AND METHODS: Combined published and unpublished data from comparative studies on BCG versus mitomycin C for superficial bladder carcinoma considering possible confounding factors were analyzed. Odds ratio (OR) and its 95% CI were used as primary effect size estimate. Toxicity data were evaluated descriptively. RESULTS: In 11 eligible clinical trials 1,421 patients were treated with BCG and 1,328 were treated with mitomycin C. Within the overall median followup time of 26 months 38.6% of the patients in the BCG group and 46.4% of those in the mitomycin C group had tumor recurrence. In 7 of 11 studies BCG was significantly superior to mitomycin C, in 3 studies no significant difference was found, while in 1 study mitomycin C was significantly superior to BCG. An overall statistically significant superiority of BCG versus mitomycin C efficacy in reducing tumor recurrence was detected (OR 0.56, 95% CI 0.38 to 0.84, p = 0.005). In the subgroup treated with BCG maintenance all 6 individual studies showed a significant superiority of BCG over mitomycin C (OR 0.43, 95% CI 0.35 to 0.53, p <0.001). In 4 of the 5 studies with reported data on toxicity BCG associated cystitis was significantly more frequent than in the mitomycin C group (53.8% versus 39.2%). The combined cystitis OR was 1.81 (95% CI 1.48 to 2.23, p <0.001). The OR for cystitis in the BCG maintenance group did not significantly differ from that in the nonmaintenance therapy group. CONCLUSIONS: The results suggest superiority of BCG over mitomycin C for prevention of tumor recurrences in the combined data and particularly in the BCG maintenance treatment subgroup, irrespective of the actual (intermediate or high) tumor risk status. The toxicity with BCG is higher but does not differ between BCG maintenance and nonmaintenance groups. Publication Types: Meta-Analysis PMID: 12478111 [PubMed] 6: J Urol. 2002 Nov;168(5):1964-70. Intravesical bacillus Calmette-Guerin reduces the risk of progression in patients with superficial bladder cancer: a meta-analysis of the published results of randomized clinical trials. Sylvester RJ, van der MEIJDEN AP, Lamm DL. European Organisation for Research and Treatment of Cancer Data Center, Brussels, Belgium. PURPOSE: We determine if intravesical bacillus Calmette-Guerin (BCG) reduces the risk of progression after transurethral resection to stage T2 disease or higher in patients with superficial (stage Ta, T1 or carcinoma in situ) bladder cancer. MATERIALS AND METHODS: A meta-analysis was performed of the published results of randomized clinical trials comparing transurethral resection plus intravesical BCG to either resection alone or resection plus another treatment other than BCG. RESULTS: We identified 24 trials with progression information on 4,863 patients. Based on a median followup of 2.5 years and a maximum of 15 years, 260 of 2,658 patients on BCG (9.8%) had progression compared to 304 of 2,205 patients in the control groups (13.8%), a reduction of 27% in the odds of progression on BCG (OR 0.73, p = 0.001). The percent of patients with progression was low (6.4% of 2,880 patients with papillary tumors and 13.9% of 403 patients with carcinoma in situ, reflecting the short followup and relatively low risk patients entered in many of the trials. The size of the treatment effect was similar in patients with papillary tumors and in those with carcinoma in situ. However, only patients receiving maintenance BCG benefited. There was no statistically significant difference in treatment effect for either overall survival or death due to bladder cancer. CONCLUSIONS: Intravesical BCG significantly reduces the risk of progression after transurethral resection in patients with superficial bladder cancer who receive maintenance treatment. Thus, it is the agent of choice for patients with intermediate and high risk papillary tumors and those with carcinoma in situ. Publication Types: Meta-Analysis PMID: 12394686 [PubMed] 7: Anticancer Res. 2001 Jan-Feb;21(1B):765-9. Impact of intravesical chemotherapy on recurrence rate of recurrent superficial transitional cell carcinoma of the bladder: results of a meta-analysis. Huncharek M, McGarry R, Kupelnick B. Division of Radiation Oncology, Department of Clinical Oncology, Marshfield Clinic Cancer Center, Marshfield, WI, USA. metaresearch@hotmail.com BACKGROUND: The impact of in tranvesical chemotherapy on preventing recurrence of superficial transitional cell carcinoma of the bladder is controversial. The objective of this report is to present a meta-analysis of the available clinical trial data to quantify the effect of intravesical chemotherapy on tumor recurrence following trans-urethral resection (TURB) in patients with recurrent superficial bladder cancer. METHODS: A prospective study protocol outlining a meta-analysis was developed followed by a thorough search of the existing published literature using strict eligibility criteria. Eight randomized trials were found which met protocol specifications. These studies contained data on 1,609 patients which were statistically combined using a fixed effects model (Peto). The outcome of interest was the proportion of patients with tumor recurrence at one, two and three years post-TURB. RESULTS: Combining all 8 studies using 1 year recurrence as the outcome measure yielded a Peto odds ratio (ORp) of 0.62, demonstrating a 38% reduction in one year recurrence among patients treated with intravesical chemotherapy versus TURB alone. Using 2 and 3 year recurrence as the outcome measure yielded ORp's of 0.46 and 0.35 respectively, favoring TURB + intravesical chemotherapy versus TURB alone. A statistical test for heterogeneity (Q) showed the 2 and 3 year outcome data to be heterogeneous (i.e. the studies are not measuring an effect of the same magnitude). Sensitivity analyses showed that drug type appeared to account for the observed heterogeneity with a stratified analysis demonstrating that adriamycin is less effective in reducing subsequent tumor recurrences than all other drugs studied. CONCLUSION: Intravesical chemotherapy appears to have a major impact on decreasing the chance of recurrence of recurrent superficial bladder cancer. Three year recurrence is decreased by as much as 70% when compared with TURB alone. These data are in contrast to prior analyses suggesting only modest efficacy of such treatment in this clinical setting. Publication Types: Meta-Analysis PMID: 11299841 [PubMed]