Prescription and administration charts (completion procedure)

Portfolio
Document name:
Document type:
Staff group to whom it applies:
Distribution:
How to access:
Issue date:
Next review:
Approved by:
Developed by:
Director leads:
Contact for advice:
D:\726946881.doc
Medicines Management
Prescription and Administration Chart
Guidelines
Procedure for the completion of prescription and administration charts
Pharmacy
Procedure
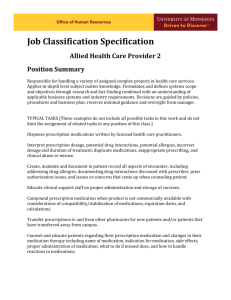
All staff who prescribe, dispense or administer medication.
Ward folders
Intranet
Ward folders
Intranet
PA to Chief Pharmacist
May 2007
May 2009
Drug and Therapeutics Trust Action
Group
Chief Pharmacist
Dr N H Booya
Medical Director
Lynn Haygarth
Chief Pharmacist
01422 281351
Lynn.haygarth@swyt.nhs.uk
1
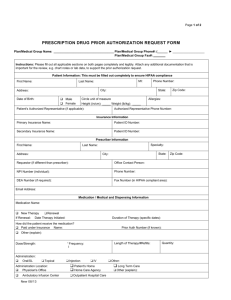
PROCEDURE FOR COMPLETION OF PRESCRIPTION AND ADMINISTRATION
CHART
LOCALITY: Trustwide
OBJECTIVE: To ensure that all prescription and administration records are completed correctly and consistently.
SCOPE: This standard operating procedure details the approved method of completing all sections of the prescription and administration record sheet by authorised prescribers, doctors, nurses and pharmacists.
GENERAL GUIDANCE
Only use accepted codes for routes of administration.
Ext External use
IM Intramuscular
PR Per Rectum
Inh Inhalation
IV Intravenous
PV Per Vagina
Top Topical
Neb Nebulisation
PO Oral
Only use generic drug names except drugs that are brand specific eg. Lithium,
Fentanyl Patches.
Drug names to be written in block capitals or clear print.
Write Micrograms in full. Prescribe doses of less than 1mg in MICROGRAMS .
Prescribers to complete chart in permanent black ink.
The prescriber’s signature should be identifiable or the name should be clearly printed next to the signature.
Pharmacists to sign and annotate entries in permanent green ink. o A pharmacist ’s initials in green next to a medication on the chart usually indicate that they have seen the chart and can see no clinical reason to deem the medication inappropriate. Supplies should therefore be available. o If a chart is not signed by a pharmacist then the appropriateness of the medication has not been assessed.
VERBAL ORDERS CANNOT BE TAKEN BY NURSES (Drug and
Therapeutics Policy Action Group November 2004).
Any request for a compliance aid must be supported by a completed Multi-
Compartment Compliance Aid assessment form and 2 working days notice is required by pharmacy to process this. o NB consider why the aid is required –would a clear instruction chart be of value?
D:\726946881.doc 2
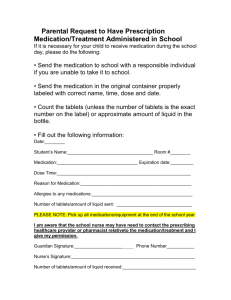
FRONT SHEET
Affix Addressograph to patient details box, if not available complete by hand.
Complete HOSPITAL and WARD section.
Complete CONSULTANT section.
Complete MENTAL HEALTH ACT STATUS.
Allergy box must be completed o Allergies entry to be signed and state where information is from, i.e. patient, GP, notes. Adverse effect suffered to be entered e.g. rashpenicillin. If nil, write
‘nil known’.
o Pharmacy are unable to supply medication if the allergy box is not complete.
Complete PRECAUTIONS section, this may be ‘chart 1 of 2’ or ‘patient with similar name’, high dose antipsychotic monitoring required, diabetic etc.
Make sure the patients name is also inside the front cover
ONCE ONLY MEDICATION SECTION
This is to be used, for example, for test doses of depot medication, enemas, pessaries and zuclopenthixol acetate injection.
Responsibility of prescriber
Complete DATE section, this is date written.
Complete NAME and STRENGTH of medication in ‘once only medication’ box.
Complete DATE and TIME to be given.
Complete ROUTE section and
PRESCRIBER’S SIGNATURE section.
Responsibility of nurse
On administration initial the GIVEN BY section and complete the TIME GIVEN section.
SHORT COURSES
Usually used, for example, for chlordiazepoxide reducing regimens, increasing doses, antibiotics, short courses of hypnotics and anxiolytics and the introduction of drugs requiring titration e.g. quetiapine, lamotrogine.
Responsibility of prescriber
Complete DRUG section with medication name, strength and form of preperation.
Complete DOSE section with specific dose or ‘Variable’ and then state specific doses in VARIABLE DOSES section in line with relevant time.
State route, start date and length of treatment or stop date and sign .
Put a TICK in the box next to the required time of day (24hr clock)
Complete the SPECIAL INSTRUCTION section if required.
Responsibility of nurse:
Complete DATES at top of each administration column.
Complete administration record.
If dose is omitted the relevant code, as below should be written in red ink
D:\726946881.doc 3
CODE
X
NBM
MEANS
Refused
Nil by Mouth
L
S
On Leave
Self-administration supervised
O Omitted (for another reason documented in nursing notes)
Nurses initials Dose administered
REGULAR PRESCRIPTIONS
Responsibility of prescriber
Complete as per SHORT COURSE section except for stop date, this need not be filled in until a decision has been made to stop the medication.
A change in dose requires a rewrite. A stop date should be added, a line should be drawn through the prescription section and a vertical line drawn at the end of the administration column.
When a chart is full it is the responsibility of the prescriber to transfer the current prescription to a new chart and cancel the completed chart.
Responsibility of nurse:
Ensure patient details on the front of the chart are correct and complete.
Complete the correct dates across the top of the administration chart.
Take into account any special instructions.
Check MHA status and forms 38/39 if necessary. Form 38/39 forms should be attached to card.
Complete the administration chart with the above codes, also found on the front cover of the chart.
LEAVE SECTION
Responsibility of prescriber
Each medication required for leave should be written separately stating
START and END dates of leave
Do not request compliance aids for leave unless one is currently in use for the patient
Any PRN medication that is required should be written in full on the leave section and numbers of tablets required should be written clearly eg.
Zopiclone 7.5mg, one at night if required, send 3 tablets o Do not expect pharmacy staff to guess
The maximum number of days allowed for leave medication is seven
If more is required please get advice from the ward pharmacist
Controlled drugs e.g. morphine or methadone must be prescribed separately on the CD prescription (as well as on the leave section of the chart) for the period of the leave
D:\726946881.doc 4
AS REQUIRED MEDICATION (PRN)
Responsibility of prescriber
Complete as previously stated for the Once Only Medication and Regular
Prescription Sections with the addition of a frequency e.g. every 6 hours.
The MAXIMUM dose allowed in 24 hours must be stated.
‘As Required’ medication should be reviewed regularly with special consideration given to hypnotics and anxiolytics.
Responsibility of nurse:
Ensure PRN medication is indicated.
Check when the medication was last given (including regular medication) and ensure frequency and maximum dose have not been exceeded.
Initial the administration section using the codes above and on the front sheet of the chart.
A new section should be completed by the doctor if all the administration boxes are full, do not continue into the next section.
If medication is prescribed either oral or by injection the route must be completed on the administration section of the chart.
SYMPTOMATIC RELIEF See approved policy for full detail
This policy allows the administration of the following medications:
Simple Linctus - One 5ml spoonful, every 4 hours, three doses allowed.
Paracetamol tablets - One or two 500mg tablets, every four to six hours, three doses allowed.
Antacid mixture - One or two 5ml spoonful after meals three doses allowed.
Glycerin suppository - One daily per rectum, one dose allowed.
Throat lozenge - One every four hours, three doses allowed.
Senna tablets/liquid - Two tablets or two 5ml spoonfuls at night, one dose allowed.
Nicorette 2mg chewing gum. Buccal -chew slowly for one minute, then place between the gum and cheek (8 to 12 pieces per day) 15 pieces allowed.
Responsibility of prescriber
Check the symptomatic relief section on the reverse of the inpatient prescription chart.
Insert the names of any medicines for symptomatic relief which are not appropriate for the patient and then sign and date the symptomatic relief section.
Responsibility of nurse:
Administer only the medicines as specified.
Complete the chart in vertical order.
Inform doctor and ensure prescription written if further doses necessary
RESPONSIBILITY: Doctors, Nurses, Pharmacists, Pharmacy Technician
RISKS: New Staff, Illegible Handwriting, Poor Spelling, Time Constraints
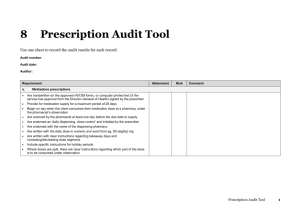
REVIEW / AUDIT
Updated May 2007
This procedure will be reviewed when there are any major changes to the law affecting the dispensing process or any changes to the prescription stationary.
In absence of any of these events it will be reviewed every 2 years.
D:\726946881.doc 5