Acetylcysteine in Pulmonary Fibrosis
advertisement

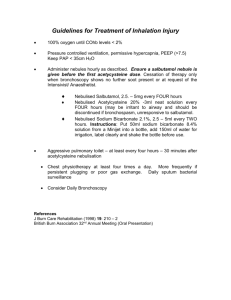
Guidance for the use of Acetylcysteine in patients with Pulmonary Fibrosis Acetylcysteine is unlicensed in the UK and any doctor who prescribes the medication legally assumes clinical responsibility for the drug, and the consequences of its use. Introduction: Acetylcysteine is a precursor of glutathione, an antioxidant, and so prevents cellular damage. It is thought to inhibit glutathione depletion and thus reduce fibroproliferation1. Acetylcysteine has been shown to delay the decline in lung function in patients with idiopathic Pulmonary Fibrosis. Its use (Acetylcysteine 600 mg three times daily) added to Prednisone and Azathioprine, showed preservation of vital capacity and carbon monoxide diffusing capacity better than did Azathioprine and Prednisolone alone2. Use of this combination (Acetylcysteine, Prednisolone and Azathioprine) has now been discontinued due to poorer patient outcomes in clinical trials by the National Heart, Lung and Blood Institute. As a result, the British Thoracic Society3 (BTS) has recommended against its use. Monotherapy with Acetylcysteine remains safe in idiopathic Pulmonary Fibrosis and the BTS recommends its use. With respect to a definite diagnosis for idiopathic Pulmonary Fibrosis, the BTS recommends3: Patients with definite, newly diagnosed idiopathic Pulmonary Fibrosis should not be initiated on a regimen containing Prednisolone plus Azathioprine Patients currently receiving ‘triple’ therapy and who experience disease progression (declining lung function), should have Azathioprine, in particular, withdrawn. Patients established on ‘triple’ therapy who do not experience disease progression (i.e. ‘stable’ disease) should be discussed on an individual basis with respect to continuation of therapy. The decision to withdraw should be on a case by case basis but the threshold for withdrawing azathioprine from elderly patients should be low. Contraindications4,5: Hypersensitivity to Acetylcysteine (or any of the other ingredients in the tablet) including bronchospasm, rash, pruritus, angioedema, flushing, nausea, vomiting; this list is not exhaustive and is more common with the intravenous use of Acetylcysteine. Children under the age of 14 years (high dose oral Acetylcysteine). First presentation of severe skin and mucous membrane reactions. Very rare incidences of Stevens-Johnson syndrome and Lyell’s syndrome have been reported. Active Gastrointestinal ulceration. Use with caution in the presence of any of the following4,5: Bronchial asthma- risk of bronchospasm and exacerbation of asthma, however, this is most common with the intravenous formulation. Previous stomach or intestinal ulceration- drug-induced nausea and vomiting may lead to GI haemorrhage in this patient group. Mucolytics may disrupt the mucosal barrier. Hepatic impairment- leads to reduced clearance. Histamine intolerance (symptoms leading to headaches, runny nose, itching) - avoid long term use. BHNFT October 2013 Drug interactions5 Antitussives The combined action of a reduced cough reflex with antitussives and the use of acetylcysteine can lead to a dangerous build-up of mucus secretions. Advise patients on the use of over the counter preparations. Antibiotics Acetylcysteine may reduce the efficacy of certain antibiotics (particularly; tetracycline’s, aminoglycosides, and penicillin’s). Allow a 2 hour gap between Acetylcysteine and these antibiotics to prevent the interaction. Dosage, administration and treatment duration: Treatment with Acetylcysteine will be initiated by a specialist. The dosing schedule is as follows: Acetylcysteine effervescent tablets 600mg TDS The patient should be advised to take the tablets by dissolving them in one glass of water or by swallowing them whole with plenty of water. They should be taken after meals. Treatment will be reviewed periodically by the initiating specialist and therapy should be continued with the instruction of the specialist. Excipients: BHNFT currently uses ACC 600mg brand tablets, made by Hexal (imported from Germany). The inactive ingredients in the tablets are microcrystalline stearate, maize starch, sodium cyclamate, sodium saccharin and flavourings (lemon). Monitoring: The only monitoring routinely required whilst on Acetylcysteine is respiratory function and evidence of adverse effects. Liver and renal function need only be monitored if the patient has pre-existing dysfunction. Adverse effects: The most common side effects of treatment include; headache, fever, allergic reactions (breathing difficulties, rash, pruritus, tachycardia, hypotension), nausea, vomiting, diarrhoea, abdominal pain and inflammation of mucous membranes in the mouth. Worsening of these symptoms should warrant medical attention and withdrawal from therapy. Rarely bronchospasm, mostly in asthmatic patients, may occur. Very rarely anaphylactic reactions and shock may occur. Hypersensitivity reactions, with bleeding, may very infrequently occur, at which point therapy should be stopped. Pregnancy and Lactation: Due to insufficient knowledge of use, Acetylcysteine is contraindicated during pregnancy and lactation. Immediate advice and support Contact Details Medicines Information BHNFT Dr H A Mahdi Dr M J Malik Telephone No 01226 432857 01226 730000 01226 730000 Fax No 01226 434431 Email Gilliansmith2@nhs.net References: 1. 2. 3. 4. 5. Oral N-acetylcysteine for Idiopathic Pulmonary Fibrosis: unlicensed and off-label medicines report number 4 (2011), Wessex Drug and Medicines Information Centre, UK Medicines Information, pp. 1-10 (accessed from www.nelm.nhs.uk) Demedts, M. et. al (2005) High Dose Acetylcysteine in Idiopathic Pulmonary Fibrosis, The New England Journal of Medicine;353:pp 2229-42 British Thoracic Society. Accessed online ( 03/10/2013) http://www.brit-thoracic.org.uk/Guidelines/Interstitial-Lung-Disease-DPLDGuideline.aspx Martindale. Accessed online (04/10/2013) www.medicinescomplete.com ACC 600mg tablets- Patient information leaflet (translated in to English by Durbin Plc.) BHNFT October 2013