HEPATITIS C VIRUS GENOTYPES AND VIREMIA IN ANTI
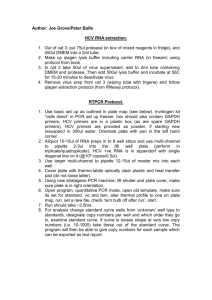
advertisement

HEPATITIS C VIRUS GENOTYPES AND DETECTION OF VIRAL RNA BY PCR IN SERUM SAMPLES FROM EAST AFRICA BY PAUL KATO KITANDWE BSc. (Mak) REG.NO. 2006/HD17/6770U A RESEARCH REPORT SUBMITTED IN PARTIAL FULFILMENT OF THE REQUIREMENTS FOR THE AWARD OF MASTERS IN BIOMEDICAL LABORATORY SCIENCE AND MANAGEMENT DEGREE OF MAKERERE UNIVERSITY DECEMBER 2011 i DECLARATION I Paul Kato Kitandwe do hereby declare that “Hepatitis C Virus Genotypes and Detection of Viral RNA by PCR in Serum Samples from East Africa” is entirely my original work, except where acknowledged, and that it has not been submitted before to any other University or institution of higher learning for the award of a degree. Signed………………………………………… Date……………………………...... This research report has been submitted for examination with the approval of the following supervisors: 1. Dr. Anne Nanteza Faculty of Veterinary Medicine Makerere University Kampala, Uganda Date:............................................... 2. Dr. Nicaise Ndembi Genetic Sequencing Unit Institute of Human Virology Abuja, Nigeria Date:............................................... Signature:........................................ Signature:....................................... ii DEDICATION I dedicate this research work to my wife Rose Nabatanzi Kitandwe for being supportive and patient as I put in the extra time and effort necessary to complete this work. iii ACKNOWLEDGEMENTS I would like to thank the following people who helped me to conduct this work. The International AIDS Vaccine Initiative (IAVI) that funded the research work in particular I thank Leslie Nielsen, Claudia Schmidt, Pat Fast and Helen Thomson. I also thank the Medical Research Council (MRC) Uganda Research Unit on AIDS specifically the Basic Science Section for providing the facilities from where I conducted the PCR and genotyping assays. I would also like to thank Dr. Ann Nanteza and Dr. Nicaise Ndembi for supervising me. I also thank Dr. Josephine Birungi for allowing me to conduct this research work as well as Dr. Pontiano Kaleebu who encouraged me to complete it. I also thank the staff of MRC Uganda Basic Sciences Section in particular Brian Magambo for training me in PCR, and Jamila Nazziwa and Fred Lyagoba for training me in sequencing. I also thank Dr. Eduard Sanders of Kilifi, Kenya, Dr. Anatoli Kamali of Uganda, and Dr. Etienne Karita of Kigali, Rwanda for providing samples from the different sites for this study. Last but not least, I thank my family especially my parents for the efforts they have made to support my education. iv TABLE OF CONTENTS DECLARATION ........................................................................................................................ i DEDICATION .......................................................................................................................... iii ACKNOWLEDGEMENTS ...................................................................................................... iv LIST OF TABLES ................................................................................................................... vii LIST OF FIGURES ................................................................................................................ viii LIST OF ABBREVIATIONS ................................................................................................... ix ABSTRACT .............................................................................................................................. xi CHAPTER ONE: INTRODUCTION ........................................................................................ 1 1.1 Background ................................................................................................................... 1 1.2 Statement of the problem .............................................................................................. 4 1.3 Aim of the study ........................................................................................................... 5 1.4 Specific objectives of the study .................................................................................... 6 1.6 Scope............................................................................................................................. 6 1.7 Justification and significance of the study .................................................................... 7 CHAPTER TWO: LITERATURE REVIEW ............................................................................ 9 2.1 The Hepatitis C virus infection ..................................................................................... 9 2.2 The Hepatitis C virus structure ................................................................................... 10 2.3 HCV genome variability ............................................................................................. 11 2.4 HCV genotype distribution ......................................................................................... 11 2.5 HCV genotyping methods .......................................................................................... 13 2.6 HCV diagnosis ............................................................................................................ 15 2.7 HCV nucleic acid testing ............................................................................................ 17 2.7.1 The COBAS Ampliprep/Cobas Taqman HCV Test ........................................... 17 2.7.2 RNA extraction ................................................................................................... 18 2.7.3 Reverse transcriptase PCR .................................................................................. 18 CHAPTER THREE: METHODOLOGY ................................................................................ 20 3.1 Research design .......................................................................................................... 20 3.2 Ethical considerations ................................................................................................. 20 3.3 Sample population ...................................................................................................... 20 3.4 Sampling procedure .................................................................................................... 22 3.5 Laboratory data collection .......................................................................................... 23 3.5.1 RNA extraction ................................................................................................... 23 3.5.2 Polymerase chain reaction analysis ..................................................................... 24 3.5.3 Visualisation of the PCR products ...................................................................... 27 3.5.4 Purification of PCR products .............................................................................. 27 v 3.5.5 DNA sequencing ................................................................................................. 28 3.5.6 Phylogenetic analysis .......................................................................................... 29 3.5.7 HCV viral load testing ........................................................................................ 30 3.6 Data quality control .................................................................................................... 30 CHAPTER FOUR: RESULTS ................................................................................................ 32 4.1 Comparison of anti-HCV EIA results with RT-PCR results ...................................... 32 4.2 Comparison of anti-HCV EIA results with the real-time PCR results ....................... 33 4.3 Types of HCV genotypes ............................................................................................ 34 CHAPTER FIVE: DISCUSSION ............................................................................................ 35 CHAPTER SIX: CONCLUSIONS AND RECOMENDATIONS .......................................... 41 6.1 Conclusions................................................................................................................. 41 6.2 Recommendations ....................................................................................................... 41 CHAPTER SEVEN: REFERENCES ...................................................................................... 43 vi LIST OF TABLES Table 1: Sample selection across the different sites…………………………………… 22 Table 2: Reaction components for RT, primary and secondary PCR…………………. 25 Table 3: Thermo cycling conditions used for RT, primary and secondary PCR………. 26 Table 4: Contingency table of anti-HCV EIA results against PCR results……………. 32 Table 5: HCV Viral loads of PCR positive samples by country of origin……………... 34 vii LIST OF FIGURES Fig. 1: Schematic representation of the Hepatitis C virus genome........................................ 10 Fig. 2: Global distribution of Hepatitis C virus genotypes.................................................... 11 Fig. 3: Agarose gel showing results of PCR products for samples from Rwanda................ 32 Fig. 4: Phylogenetic analysis of Hepatitis C virus non-structural region 5b sequences........ 33 viii LIST OF ABBREVIATIONS AIDS Acquired Immune Deficiency Syndrome ALT Alanine Aminotransferase Anti-HCV Hepatitis C Virus Antibodies bDNA Branched Chain DNA Assay CAP/CTM Cobas Ampliprep/Cobas Taqman cDNA Complimentary DNA ddNTP Dideoxynuclelotide triphosphate DNA Deoxyribose nucleic acid dNTP Deoxyribonucleotide triphosphate EIA Enzyme Immunosorbent Assay GCLP Good Clinical Laboratory Practise HCV Hepatitis C Virus IAVI International AIDS Vaccine Initiative ISO International Standards Organisation IU International Units MRC Medical Research Council NATs Nucleic Acid Tests ORF Open Reading Frame PCR Polymerase Chain Reaction QS Quantitation Standard RFLP Restriction Fragment Length Polymorphism RIBA Recombinant Immunoblot Assay ix RNA Ribonucleic acid RT-PCR Reverse Transcriptase Polymerase Chain Reaction SANAS South African National Accreditation Scheme UGX Uganda Shillings USD United States Dollar UTR Untranslated Region UV Ultra Violet Light UVRI Uganda Virus Research Institute WHO World Health Organisation x ABSTRACT Over 170 million people worldwide are infected with the hepatitis C virus (HCV). Several generations of Enzyme immunoassays (EIAs) have been developed to detect HCV antibodies mostly using HCV genotype 1 antigens. In East Africa, there is limited information about the circulating genotypes and EIA reactive results are rarely confirmed. Some studies suggested that genotype differences affect serological reactivity while others have differed. This study aimed to confirm EIA reactive serum samples from East Africa through the detection and quantification of HCV RNA and to establish the HCV genotypes of these samples. One hundred fifty one (151) EIA reactive and 16 randomly selected negative control samples from Uganda, Kenya and Rwanda collected from clinically healthy participants of a haematology and biochemistry laboratory reference range study were used in this study. An in-house RT-PCR using non-structural region 5B genomic region targeting primers was performed on the HCV RNA extracted from these samples. Viremia was measured using the automated specimen extraction and real-time PCR. The HCV RNA positive samples were sequenced using the Dye terminator cycle sequencing quick start kit. Generated sequences were aligned with references from the Los Alamos HCV sequence database and phylogenetic analysis done using the MEGA Version 4.0 software. Nine samples (6%) had detectable HCV RNA by both the in-house RT-PCR and the CAP/CTM HCV test. Viral loads ranged from 19 to 1,058,000IU/ml. All 16 anti-HCV EIA negative control samples were HCV RNA negative. Only HCV genotype 4 was identified. There was poor correlation between EIA reactivity and HCV RNA detection. Genotype 4 is the most common HCV genotype of anti-HCV EIA reactive samples from East Africa. xi CHAPTER ONE INTRODUCTION 1.1 Background Hepatitis C virus (HCV) infection is a leading cause of chronic hepatitis and primary hepatocellular carcinoma in most parts of the world (Lionis et al., 2000). Approximately 170 million people worldwide are believed to be infected with HCV with about 3-4 million infections occurring annually (WHO and the Viral Hepatitis Prevention Board, 1999). In Africa, HCV like many other chronic infections has been overshadowed by the HIV pandemic. However, a critical review of the literature on HCV infection shows that this disease is as prevalent in Africa as tuberculosis, malaria, and sexually transmitted infections. The regions with high HCV prevalence are Asia, Middle-Orient, Africa, and South America. Sub-Saharan Africa remains the highest endemic region with a seroprevalence of 5% to 15% (Pawlotsky et al., 1998; Menendez et al., 1999; Laurent et al., 2001). However, these estimates need to be clearly established through cohort studies. Studies in some other African countries reported an HCV prevalence of 8.4% in Lagos, Nigeria (Ayolabi et al., 2006); and 1.2% in Madagascar (Ramarokoto et al., 2008). In Cameroon, a prevalence of 5.5% in pregnant women in Yaoundé (Ndumbe and Skalsky, 1993) and 6.8% among pregnant women in the rural zones of the Centre Province (Ndumbe et al., 1994) was reported. Also an HCV prevalence of 1.9% was reported again among pregnant women in Yaoundé-Cameroon (Njouom et al., 2003). 1 The screening for HCV infection depends primarily on serological assays that detect HCV antibodies (anti-HCV) by enzyme immunoassays (EIAs). Like other viral infections during the acute infection window period, HCV-specific antibodies are not detectable even though the virus is present in the blood. For this reason, antibody tests are unable to detect the virus in the early stages of infection. This seronegative period may last up to 2 months in immunocompetent and from 6 to 12 months in immunodeficient patients (Van der Poel et al., 1994; Schreiber et al., 1996, Muerhoff et al., 2002). To reduce the number of false negative results therefore, a highly sensitive assay able to detect low levels of HCV antibodies must be used for HCV screening during the window period when the risk of transmission through blood transfusion is high. Several generations of HCV EIAs have been developed to detect HCV infections. The first generation anti-HCV EIAs (EIA-1) were developed using recombinant HCV C100-3 peptides from the non-structural region 4 (NS4) genomic region of HCV (Kuo et al., 1989). The EIA-1 had relatively poor specificity and sensitivity (Alter, 1992) and the lengthy seronegative window period in some blood donors resulted in HCV transmission. The second generation EIA (EIA-2) which was introduced in 1991 incorporated recombinant antigens from nonstructural regions NS3 and NS4 and an antigen from the core region of HCV (Alter, 1992, Nakagiri et al., 1993). The EIA-2 was more specific and sensitive than the EIA-1 and the length of the seronegative window period was consequently reduced by an average of 5 weeks (Majid & Gretch, 2002). The use of this kit in low risk populations such as blood donors, however, resulted in a high number of false positive and false negative results (Courouce & 2 Janot, 1991; Hayashi et al., 1993). The third generation EIA (EIA-3) that added an NS5 epitope and reconfigured core antigens slightly improved the sensitivity and reliability of the test (Courouce et al., 1994) but not as much as that observed between the change from EIA-1 to EIA-2. The EIA-3, however, did increase detection of HCV antibodies earlier in the course of infection (Colin et al., 2001). The fourth generation HCV ELISA kit (EIA-4) incorporates carefully selected antigens derived from the core, NS3, NS4A, NS4B, and NS5A regions of the HCV genome. Even though sensitivity increases as newer generations of EIAs are developed for diagnosis of HCV infection, the specificity and sensitivity has varied between the different anti-HCV generation kits (Callahan et al., 1993; Abdel-Hamid et al., 2002; Galel et al., 2002). For this reason, supplemental tests like the recombinant immunoblot assay (RIBA) which possess high specificity and are useful in identifying false-positive test results, have been used (Schroter et al., 2001). However, the RIBA is an expensive test. Also, samples giving discordant results in multiple EIAs of different generations are often indeterminate with the RIBA (Abel-Hamid et al., 2002). As a result, quantitative HCV RNA methods have been used to detect active infection (Lunel et al., 1996; Colin et al., 2001), thus confirming samples with positive or indeterminate EIA results. In East Africa, few studies have been done to evaluate the performance of anti-HCV EIAs. During an HIV vaccine trial, IAVI 009, conducted in Entebbe Uganda in 2003, varied sensitivities were observed between two EIAs used to screen for HCV infection namely the fourth generation Innotest HCV Ab IV EIA kit (Innogenetics) and the second generation 3 Cobas Core anti-HCV EIA II kit (Roche). Out of 15 samples that were positive on the EIA-4, only 3 were positive with the EIA-2 kit. Supplemental testing of the 15 positives by HCV RNA branched chain DNA assay (bDNA) was not concordant with either of the EIA kit. Similar findings were observed by Callahan et al., (1993) while working with samples from a Ugandan population in which two EIA-2 kits and two supplemental assays, second generation RIBA and line immunoassay (Innogenetics) exhibited a significant degree of discordance. Most anti-HCV EIAs being used today are predominantly based on antigens derived from HCV genotype 1. For EIA-4, HCV genotypes 1a, 1b, 2 and 3a were used. In Africa, genotypes 4 and 5 are the most prevalent (Forns & Bukh, 1998; Zein, 2000) but in East Africa, few studies have been done to determine the most prevalent genotypes. Nevertheless, genotype 4 has been commonly identified in some selected populations in East Africa (Biggar et al., 2006, Muasya et al., 2008). HCV genotype specific serological activity has been previously reported (Dhaliwal et al., 1996; Neville et al., 1997), affecting the sensitivity of HCV EIAs. 1.2 Statement of the problem Infection with HCV is a public health problem with approximately 3% of the world’s population infected with this virus (WHO, 1999). It is estimated that this infection accounts for 27% of liver cirrhosis and 25% of primary hepatocellular carcinoma worldwide (Alter, 2007). 4 In East Africa, EIA reactive (EIA-positive) samples are rarely confirmed with more specific tests (Biggar et al., 2006, Hladik et al., 2006). Furthermore, few countries in this region routinely screen blood for HCV mainly because of the high costs involved (Madhava et al., 2002). In Uganda for example, the cost of screening blood for HCV was estimated to be 112 times higher than that of hepatitis B screening, which is routinely done (Hladik et al., 2006). Whereas immunoblot assays can be used as confirmatory HCV tests, they have major limitations including not detecting HCV in the window period of infection and frequently producing indeterminate results (Abdel-Hamid et al., 2002). The use of more specific antiHCV EIAs can therefore drastically reduce the cost of HCV screening in East Africa by reducing the number of samples requiring confirmatory testing. Most of the EIAs being used today were made using HCV genotype 1 antigens and to a lesser extent genotypes 2 and 3. These genotypes (1-3) are the most prevalent ones in Europe and North America. Studies done in some parts of Africa have identified genotypes 4 and 5 as the most prevalent (Forns & Bukh, 1998; Zein, 2000). In East Africa, the few studies done so far have reported genotype 4 (Biggar et al., 2006; Muasya et al., 2008). Some studies reported that there exists differences in serological re-activities among the different HCV genotypes (Neville et al., 1997, Dhaliwal et al., 1996). It is, therefore, possible that current generation EIAs do not optimally detect the HCV genotypes found in East Africa. 1.3 Aim of the study The purpose of this study was to verify the results of hepatitis C virus antibody reactive serum samples from East Africa through viral RNA detection and to determine their genotypes. 5 1.4 Specific objectives of the study 1. To determine the percentage of anti-HCV EIA reactive samples with detectable HCV RNA using an in-house RT-PCR. 2. To measure viral loads in the anti-HCV EIA reactive samples irrespective of the inhouse RT-PCR results. 3. To establish the HCV genotypes in the HCV RNA-positive samples. 1.5 Study questions 1. What is the correlation between anti-HCV EIA reactivity and the detection of HCV RNA in serum samples from East Africa? 2. What are the HCV genotypes of anti-HCV EIA reactive samples from East Africa? 1.6 Scope This study was conducted using archived serum samples from sites in three East African countries i.e. Uganda (Masaka and Entebbe), Kenya (Kilifi), and Rwanda (Kigali). These samples had been collected during the screening phase of a laboratory reference range study conducted in 2005 to determine the normal haematology and biochemistry values of East and Southern African populations. They were from clinically healthy adult volunteers screened for HCV infection using two anti-HCV EIAs. All anti-HCV EIA positive samples identified during this screening process and a few negative samples were shipped on dry ice from the above mentioned countries to the Uganda Virus Research Institute (UVRI) where RNA 6 extraction, in-house RT-PCR and HCV genome sequencing were done. Samples were also shipped to the National Health Laboratory Services (NHLS) in Johannesburg, South Africa for HCV viral load measurement. This viral load testing was done by the NHLS staff following established procedures. 1.7 Justification and significance of the study This study will help in the development of a cost effective and reliable in-house RT-PCR that can be used to confirm anti-HCV EIA-positive samples in East Africa. Two HCV RNA detection methods namely, an in house RT-PCR and a commercial real time RT-PCR Cobas Ampliprep/Cobas Taqman (CAP/CTM) were used in this study. Whereas both methods are very sensitive and specific, the CAP/CTM HCV assay is more robust and reproducible because it is fully automated (Majid and Gretch, 2002). On the other hand, the in-house RTPCR is less expensive costing about USD30 (UGX. 76,320) per test as opposed to the USD150 (UGX. 381,600) required for the CAP/CTM HCV test. This makes the former method more cost effective than the latter for use in the resource-limited countries of East Africa. With increasing access to antiretroviral therapy across Sub-Saharan Africa, HCV/HIV coinfection is an issue of concern. As HIV-infected individuals live longer, the effects of coinfection with chronic hepatitis C becomes more relevant. Indeed, HIV adversely affects the natural history of HCV, both of which are endemic across the African continent (Apurva & Jordan, 2007). Patients infected with both viruses have been reported to progress to cirrhosis 7 faster than those infected with HCV alone (Benhamou et al., 1999; Puoti et al., 2001). Therefore, it is important that HCV infection be accurately confirmed especially in HIVpositive patients in order to better manage hepatotoxicity issues that are commonly associated with highly active anti-retroviral treatment. This study will also help determine the reliability of current generation anti-HCV EIAs in detecting HCV in samples from East Africa. It will also ascertain whether HCV genotypes found in East Africa are readily detected by the current anti-HCV EIAs that were designed using antigens from genotypes commonly found in the developed world. Consequently, this study will help to determine whether it is it is important to design anti-HCV EIAs using HCV antigens from genotypes commonly found in their intended region of use. 8 CHAPTER TWO LITERATURE REVIEW 2.1 The Hepatitis C virus infection Hepatitis C is an infectious disease of the liver caused by the hepatitis C virus (Choo et al., 1989). Acute infection is rarely detected because the majority of newly infected people develop only mild or no clinical symptoms. Approximately 75% to 85% of those infected do not clear the virus and develop chronic HCV infection marked by the persistence of serum HCV antibodies for at least 6 months after the onset of acute HCV infection (Chen & Morgan, 2006). The rate of chronic infection is affected by a person’s age, gender, race and viral immune response (Seef, 2002). An estimated 10% to 15% of infected persons advance to liver cirrhosis within the first 20 years of infection (Chen & Morgan, 2006). Transmission of HCV is mainly through direct contact with blood. Other routes of infection are less efficient (Macdonald et al., 1996). In countries where routine screening of donated blood is not done, blood transfusions are a major route of infection. For example, in Benin where routine blood screening is not done, an HCV antibody prevalence of 17% was reported in sickle cell patients who had at least three life-time transfusions verses 0% in those without that history (Jeannel et al., 1998). At present, there is no vaccine against HCV for a number of reasons. The virus is highly mutable with escape mutations undermining vaccine-induced virus-specific immunity. Lack of a small animal model and cell culture systems have also posed problems for vaccine 9 development and testing (Abrignani, et al., 1999). Due to the limited tissue tropism and host selection, HCV could be generated in vitro in tissue culture systems only very recently (Chevaliez & Pawlotsky, 2006). In the absence of tissue culture techniques, adequate number of viruses could not be generated for vaccine antigen development. 2.2 The Hepatitis C virus structure The hepatitis C virus is an enveloped positive-sense single-stranded RNA virus with a diameter of about 50 nm (Choo et al., 1989). It is classified as a separate genus Hepacivirus within the Flaviviridae family. The HCV genome contains approximately 9400 nucleotides with a single open reading frame (ORF) flanked by 5’ and 3’ untranslated regions (UTR) that are important for the translation and replication of the viral RNA. The polyprotein precursor encoded by the open reading frame is cleaved by viral and host proteases into the core (C) protein, envelope 1 and 2 (E1 and E2) glycoproteins, as well as 6 non-structural proteins (NS2, NS3, NS4A, NS4B, NS5A and NS5B) (Choo et al., 1989). A seventh non-stuctrual polyprotein, p7 was discovered later on (Lin et al, 1994; Mizushima et al., 1994). See figure 1 below. Figure 1: Schematic representation of the HCV genome (Adapted from Chevaliez & Pawlotsky, 2006) 10 2.3 HCV genome variability Different isolates of HCV show substantial nucleotide sequence variability distributed throughout the viral genome. Regions encoding the envelope proteins El, E2 and the nonstructural protein NS-1 are the most variable (Weiner et al., 1991), whereas the 5' untranslated region (5'UTR) is the most conserved (Han et al., 1991; Okamoto et al., 1990). Nucleotide sequence variability in the 5’UTR also differs from that found in the coding regions in that there are no reliable sequence polymorphisms in this region to allow for the differentiation of HCV subtypes. The HCV subtypes 1a, 1b and 1c show essentially the same sequences in the 5’UTR as do subtypes 2a and 2c for example (Simmonds et al., 1993). Variability of the sub genomic region of NS5 is generally representative of the virus as a whole; therefore, sequencing larger pieces of the genome is not necessary in order to subtype the virus (Mellor et al., 1995). 2.4 HCV genotype distribution According to a WHO report of 2009, the global distribution of hepatitis C virus genotypes indicates that the hepatitis C virus is genetically diverse (Figure 2). Several typing methodologies have led to a consensus nomenclature of six major HCV genotypes and over 80 subtypes distributed across the world (Kuiken et al., 2005). Genotypes differ at more than 30% of nucleotides across the entire genome while subtypes vary at more than 20% of the sites (Simmonds et al., 1995). Genotypes 1, 2 and 3 have a worldwide distribution predominating in Northern Europe and North America, Southern and Eastern Europe and in Japan (McOmish et al., 1994, Davidson et al., 1995, Zein, 2000). In Central and North Africa, the most prevalent genotype is 4 (McOmish et al., 1994; Ndjoumu et al., 2003), 11 whereas in West Africa, genotypes 1, 2 and 4 have been isolated (Oni & Harrison, 1996; Jeannel et al., 1998). Genotype 5 has been identified mostly in South Africa accounting for about 40% of all infections whereas genotype 6 is found mainly in Eastern Asia (Smuts & Kannemeyer, 1995). Figure 2: Global distribution of Hepatitis C virus genotypes (WHO, 2009) In East Africa, few studies have been conducted to identify the circulating genotypes. A study that was done in Uganda among sickle cell children and their mothers identified only genotype 4 (Biggar et al., 2006). Another study conducted in Kenya among a high-risk cohort 12 of illicit drug users identified both genotypes 1 and 4 (Muasya et al., 2008). More studies using samples from the general population are required to confirm these findings. The clinical significance of HCV genotyping is that it guides clinicians in determining the course and duration of antiviral therapy when treating HCV infected patients. For example, patients with genotype 2 or 3 require on average 24 weeks of treatment, while those with genotype 1 require 48 weeks (Zuezem et al., 2009). 2.5 HCV genotyping methods The gold standard of HCV genotyping is to amplify viral nucleic acid and perform direct nucleic acid sequence analysis of the region of the viral genome to be classified (Majid & Gretch, 2002). Most commercial methods target the 5′UTR because of its high degree of conservation among different subtypes. However, this region does not allow sufficient discrimination between closely related subtypes within the same genotype. As a result, sequencing of an appropriate coding region enables better discrimination of HCV types and subtypes. The chain termination method introduced in 1975 by Sanger and co-workers became the sequencing method of choice owing to its relative ease and reliability. In this method, PCR is conducted in the presence of dideoxynucleotides (ddNTPs) which are the chain-terminating nucleotides lacking a 3'-OH group required in the formation of a phosphodiester bond between two nucleotides. This results in the termination of DNA elongation leading to the formation of DNA strands of varying lengths. The newly synthesized and labelled DNA 13 fragments are heat denatured and separated by size using gel electrophoresis on a denaturing polyacrylamide gel. The DNA bands are then visualized by autoradiography or ultraviolet (UV) light and the DNA sequence can be directly read off the X-ray film or gel image (Sanger et al., 1977). Today, sequencing is frequently done using the dye-terminator sequencing method introduced by Hood and co-workers (Smith et al., 1986). This method employs four ddNTP chain terminators, tagged with dyes of different fluorescent emission wavelengths in a single sequencing reaction. Detection is done using a laser fluorescence detector combined with a computer. Using specialised software, generated sequences are cleaned up and then compared to those in sequence databases to deduce phylogenetic relationships. The main disadvantage of genotyping by direct nucleic acid sequencing is that it is very expensive and complex to be used on a large scale or routine clinical basis. Its major advantage is its robustness and speed (Majid & Gretch, 2002). Another method that can be used to genotype HCV is by use of PCR using type-specific oligonucleotide primers for core, NS5 and E1 regions of the HCV genome. This qualitative PCR methodology is prone to technical issues related to conventional qualitative PCR namely contamination, optimization for sensitivity, specificity and standardization. Development of new automated real time PCR genotyping platforms using genotype/subtype specific probes has greatly minimized the limitations of this method (Nakatani et al., 2010). 14 Restriction fragment length polymorphism (RFLP) analysis on the PCR products of 5'UTR and NS5 has also been used to genotype HCV (Nakao et al., 1991). Specific restriction endonucleases are used to cleave amplicons containing conserved mutations in these regions relative to other HCV genotypes. Only certain genotypes are cleaved by specific restriction enzymes and unique RFLP patterns are observed on ethidium bromide-stained gels. Whereas this technique is useful in the high-throughput setting, its limitations include PCR dependency and potential partial digestions of amplicons leading to unclear RFLP patterns (Majid & Gretch, 2002). Commercial methods are also available for genotyping HCV. These include the DNA hybridization method INNO-LiPAHCV II (Innogenetics, Ghent, Belgium) and the direct sequencing method using the TRUGENE HCV 5’NC genotyping kit (Visible Genetics, Ontario, Canada). In the INNO-LiPAHCV II method, biotinylated PCR amplicons bind to type-specific DNA probes immobilized on nitrocellulose strips. Positive reactions are then identified using a streptavidin-colorimetric reaction. Although both methodologies are reliable at genotyping HCV, the TRUGENE HCV 5’NC genotyping is more superior at the sub typing level (Zekri, et al, 2007). 2.6 HCV diagnosis The laboratory diagnosis of HCV infection is usually made on the basis of detection of HCV antibodies using anti-HCV EIAs. Whereas these assays are useful in diagnosing exposure to HCV, they neither provide evidence of active viremia nor identify persons in the window period. In such circumstances, nucleic acid testing to detect HCV RNA is recommended. 15 Hepatitis C Virus RNA becomes detectable 7-14 days after exposure as opposed to the antibodies which may take between 4-10 weeks to develop (Caruntu & Benea, 2006). Serological tests used to detect HCV antibodies are generally classified as screening tests or confirmatory tests. Screening tests provide the presumptive identification of antibody positive specimens, while confirmatory tests are used to confirm that specimens found reactive with a particular screening test contain antibodies specific to HCV. When several screening tests are used in a testing algorithm to determine a final sero-status, these second and/or third line tests are generally referred to as supplemental tests (WHO, 2001). Confirmatory assays that are commercially available for the diagnosis of HCV include line/strip immunoassays and assays using Nucleic acid tests (NATs). Line/strip immunoassays have individual recombinant or synthetic antigens applied as separate lines to the solid phase. In this way the different antigens to which antibodies in a specimen are reacting can be distinguished. The application of established confirmation patterns of reactivity observed permits greater specificity. Examples of line/strip immunoassays include RIBA HCV 3.0 SIA (Chiron Corporation) and Inno-LIA HCV antibody III (Innogenetics). For screening and supplemental tests to be used in an HCV confirmatory strategy, they must be carefully selected to ensure that common false reactivity between these assays does not occur. In developing countries, supplemental tests are often omitted because of their high cost therefore, the reliability of the anti-HCV EIAs becomes very important (Abdel-Hamid et al, 2002). 16 2.7 HCV nucleic acid testing Nucleic acid tests (NATs) that detect HCV RNA can also be used as supplemental tests for anti-HCV EIAs. They are commonly used in clinical practice to confirm HCV diagnosis and to assess viremia in patients undergoing antiviral treatment (Zuezem et al., 2009). Nucleic acid tests are based on the PCR technique and can either be qualitative or quantitative. 2.7.1 The COBAS Ampliprep/Cobas Taqman HCV Test The COBAS Ampliprep/Cobas Taqman (CAP/CTM) HCV test is a real time PCR test for the quantification of HCV RNA in human serum or plasma. Specimen preparation, reverse transcription, PCR amplification and detection are all automated. The method relies on amplification of viral nucleic acids in the presence of a specific competitor molecule called the Quantitation Standard (QS). The HCV QS contains HCV sequences with identical primer binding sites as the HCV target RNA and a unique probe binding region that allows HCV QS amplicon to be distinguished from HCV target amplicon. The quantity of HCV RNA is measured by comparing the ratio of amplification products derived from the viral RNA and the HCV QS. A known amount of QS RNA is titrated directly into the sample and is extracted together with the target HCV RNA before analysis by competitive reverse transcription PCR. Adding the QS directly into the clinical specimen allows the assay to be internally controlled for variations in efficiency of RNA extraction, complementary DNA synthesis and PCR because the QS is present at all steps. The CAP/CTM HCV test is very sensitive with a reported lower limit of detection of 7.4 IU/ml and similar detection rates across all HCV genotypes (Sarrazin et al, 2008; Vermehren et al., 2008). 17 2.7.2 RNA extraction In order to successfully detect HCV RNA, an effective HCV RNA isolation method needs to be used. Traditionally, RNA extraction utilised phenol chloroform separation of nucleic acids from proteins. Whereas this method is very effective in RNA isolation, its major downside is the use of hazardous chemicals in addition to being laborious. As an alternative, isolation of viral RNA may be done using commercial RNA extraction kits for example the QIAamp viral RNA mini kit (Qiagen, Hilden, Germany). This kit makes use of microspin technology and the selective binding properties of silica-gel based membrane to isolate RNA. Buffer is used to provide highly denaturing conditions to inactivate RNases. Carrier RNA is also added to enhance binding of the RNA to the QIAamp mini membrane and to reduce the chance of viral RNA degradation. This kit has been found to be very efficient in the extraction of HCV RNA when compared to other kits of a similar nature (Read, 2001). 2.7.3 Reverse transcriptase PCR Reverse transciptase and primary PCR may be done using a OneStep PCR approach whereby reverse transcription and amplification of the generated complimentary DNA (cDNA) are carried out sequentially in the same tube. Reverse transcriptase and DNA polymerase enzymes are used within the same reaction mix to enable reverse transcription and DNA amplification to take place. During reverse transcription, chemically modified DNA polymerase is completely inactive and does not interfere with the reverse transcription reaction. After reverse transcription is complete, the reactions are heated to 950C for 15 18 minutes to activate the DNA polymerase and to simultaneously inactivate the reverse transcriptase. This OneStep PCR method has been found to be superior to the two step PCR approach where reverse transcription is done separately from cDNA amplification (Sergio, et al, 2004). The RT-PCR is capable of detecting RNA in samples of low level viremia with the most sensitive and optimized PCR assays detecting HCV RNA in serum at levels of less than 100 copies per ml or 40IU/ml (Majid & Gretch, 2002). In order to increase the sensitivity and specificity of the PCR, a nested approach is used. In this method, primary PCR is done followed by secondary PCR using different primers inner to those of the primary PCR. The new primers hybridise to a sequence internal to the first round (primary) PCR primer target sequence. As a result, only specific first round RT-PCR products are amplified in the secondary PCR (Alberts, 2007). 19 CHAPTER THREE METHODOLOGY 3.1 Research design This was a cross sectional study that utilised stored serum samples previously tested for HCV antibodies using two anti-HCV EIAs. 3.2 Ethical considerations Ethical approval for this study was obtained at various levels and stages of the study. Before the start of the study, ethical approval was sought from the UVRI Science and Ethics Committee where most of the analysis and data collection was done. In addition, approval was sought and obtained and from the Uganda National Council of Science and Technology (UNCST). In order to obtain samples from the various sites in East Africa, ethical approval also was sought and obtained from the Science and Ethics Committees of each of these sites. Informed consent had been previously obtained from participants allowing the conduct of research on their samples. 3.3 Sample population The serum samples used in this study were obtained from another study whose objective was to establish the normal haematology and biochemistry laboratory reference ranges for East and Southern African populations (Stevens et al., 2008). In the reference range study, clinically asymptomatic volunteers were recruited from various sites namely; Masaka and 20 Entebbe (Uganda); Kilifi, Mtwpa, Kangemi, Nairobi (Kenya); Kigali (Rwanda) and Lusaka (Zambia). Individuals who were acutely ill, pregnant, menstruating, or had significant clinical findings were not included. Those enrolled were tested for various infections including HCV and all had tested HIV negative within three months prior to screening. Below is a breakdown of the characteristics of the population for those sites where samples were obtained for this evaluation. Zambian samples and those from some Kenyan sites were not included because all sample aliquots from these sites had been used up. Masaka-Uganda. Eligible volunteers were selected from a rural general population cohort enrolled into prospective HIV incidence studies in preparation for HIV vaccine trials. A total of 52 samples from this area were obtained from individuals identified to have splenomegaly and subsequently screened out. These 52 volunteers were later tested for anti-HCV and found to be positive. Entebbe-Uganda. Volunteers were drawn from community members who either had expressed interest to participate in future clinical trials, or were pre-screened for a previous HIV vaccine phase 1 clinical trial but were not enrolled because the trial had completed enrollment. Kilifi-Kenya. Half of this site’s study volunteers were from an HIV prevalence study in Kilifi Town, and half were selected from individuals who were enrolled in HIV incidence studies in preparation for HIV vaccine trials. Kigali-Rwanda. Half of the volunteers were drawn from large prospective studies of longterm, stable sexually active couples of HIV discordant status (the volunteer’s partner was HIV positive), and half were drawn from couples identified during couples’ voluntary counseling and testing as concordant HIV-negative (both partners HIV negative). 21 3.4 Sampling procedure Convenience sampling was used to arrive at the sample size used in this study. All samples that were anti-HCV EIA-positive in the aforementioned laboratory reference range study and a few negatives were used for this evaluation. The total sample size was 167 of which 151 were anti-HCV EIA positive and 16 were anti-HCV EIA negative (Table 1). Table 1: Sample selection across the different sites Site EIA Used Kigali, Rwanda Murex anti HCV Version 4.0 (Abbot) Entebbe, Uganda Innotest HCV Ab IV (Innogenetics) Masaka, Uganda Innotest HCV Ab IV (Innogenetics) Kilifi, Kenya Innotest HCV Ab IV (Innogenetics) Total Number of Positives 13 Number of Negatives 2 Total 10 98 30 151 1 10 3 16 11 108 33 167 15 HCV antibody testing had been done using two anti HCV EIAs, namely, the Innotest HCV Ab IV (Innogenetics NV, Gent, Belgium) and Murex anti-HCV Version 4.0 (Abbott Laboratories, Chicago, IL) following the manufacturers’ instructions in the kit. Samples from the Ugandan and Kenyan sites had been tested using the former EIA while those from Rwanda were tested using the latter EIA. The testing was done from the site of origin of these samples by the staff of these sites. Sample aliquots archived after completion of the laboratory reference range study where later shipped on dry ice to UVRI to undergo evaluation for this study. The samples used for this study do not represent a true random sample of the local population because volunteers had been selected from participants of ongoing research, or those with a 22 previous interest in participating in research studies. The Masaka site was an exception because volunteers from there were recruited from the general population after the entire adult population of three villages had been informed of upcoming research activities. 3.5 Laboratory data collection 3.5.1 RNA extraction All serum samples were extracted using the QIAamp Viral RNA extraction kit (Qiagen, Hilden, Germany) following the manufacturer’s instructions. The spin protocol was used. In summary, 140µl of serum sample was added to 560µl of viral lysis buffer dissolved with 5.6µl carrier RNA (1µg/ml). The mixture was then vortexed for 15 seconds. After 10-minute incubation at room temperature to allow for viral particle lysis and inactivation of RNases, 560µl of 96% ethanol was added to the sample to facilitate the release of RNA. The solution was then vortexed for a further 15 seconds and then applied onto the QIAamp mini spin columns into two aliquots of 630µl each. A centrifugation at 6000g for 1 minute was done in between the two aliquots with the filtrate being discarded. After centrifugation, two wash buffers AW1 and AW2 (500µl each) were then added in succession with a 1-minute centrifugation at 6000g and 20,000g, respectively, in between additions. Finally, the RNA bound to the membrane was eluted into a clean 1.5ml micro centrifuge tube by addition of 80µl of elution buffer AVE (RNase free water containing 0.04% sodium azide) to the mini spin column followed by a 1 minute centrifugation at 6000g. The extracted RNA was then temporarily stored at -200C awaiting RT-PCR which was done within a week from extraction. 23 3.5.2 Polymerase chain reaction analysis Primary and secondary PCR were performed on the extracted RNA following a nested PCR approach. Reverse transcription and primary PCR were done in a ‘one step’ reaction using the Qiagen Onestep RT-PCR Kit (Qiagen, Hilden, Germany) which uses specially formulated reverse transcriptase and DNA polymerase enzymes for reverse transcription and PCR amplification, respectively. Primers targeting the NS5B region of the HCV genome (See figure 1) were used with the sequences 5’-TAT GAY ACC CGC TGY TTT GAC TC-3’ and 5’-GCN GAR TAY CTV GTC ATA GCC TC-3’ for reverse transcription and primary PCR and 5’-CAT AGC CTC CGT GAA GRC TC-3’ and 5’-TAT GAY ACC CGC TGY TTT GAC TC-3’ for the secondary PCR (Mejri et al., 2005). They were manufactured by Eurogentec S.A, Belgium. Secondary PCR was done using the Qiagen Taq PCR master mix kit (Qiagen, Hilden, Germany). Components for both primary and secondary PCR and the thermocyling conditions that were used are outlined in tables 2 and 3. The thermo cycling program recommended in the kit insert was used. 24 Table 2: Reaction components for RT, primary and secondary PCR mixtures Volume/reaction (µl) Final concentration Component RT & Primary PCR Water 5X Qiagen OneStep RT-PCR buffer containing 12.5Mm MgCl2 dNTP mix (containing 10mM of each dNTP) Forward primer (50µM) Reverse primer (50µM) Qiagen OneStep RT-PCR Enzyme Mix RNase inhibitor (5units/µl) RNA template Total Volume Secondary PCR Master Mix Water DNA template from 10 PCR Forward primer (50µM) Reverse primer (50µM) Total Volume 8.3 - 10.0 1X 2.0 400µM of each dNTP 0.6 0.6 2.0 1.5 25.0 50.0 0.6 µM 0.6 µM 7.5units/reaction - 50.0 43.0 5.0 1.0 1.0 100 0.5µM 0.5µM - 25 Table 3: Thermo cycling conditions used for RT, primary and secondary PCR Temperature (0C) Process Time RT & Primary PCR Reverse Transcription 50 30 minutes Initial PCR activation step 95 15 minutes 3- Step Cycling 1 (5 cycles) Denaturation Annealing Extension 3- Step Cycling 2 (30 cycles) Denaturation Annealing Extension 3- Step Cycling 3 (5 cycles) Denaturation Annealing Extension/Elongation 94 62 72 30 seconds 45 seconds 1 minute 94 55 72 30 seconds 45 seconds 1 minute 94 52 72 30 seconds 45 seconds 1 minute Final Extension Hold 72 4 10 minutes 1-16 hours Secondary PCR Denaturation 95 5 minutes 3-step cycling (35 cycles) Denaturation Annealing Extension 95 55 72 30 seconds 30 seconds 30 seconds Final extension/Elongation Hold 72 4 10 minutes 1-16 hours 26 3.5.3 Visualisation of the PCR products The PCR amplicons were visualised using a 1.5% agarose gel stained with 5µl ethidium bromide. The gel was prepared by dissolving 1.5 grams of agarose powder in 100ml of 0.5X Tris-Borate-EDTA buffer (pH8). The solution containing the partially dissolved powder was heated in a microwave oven for 3 minutes to enable complete dissolution and then 5µl of ethidium bromide (10mg/ml) added to it and gently swirled. The solution was then poured onto an electrophoresis tray. Combs were then inserted into the liquid gel to create wells for sample addition. After solidification of the gel, the combs were removed and approximately 100ml of the 0.5X Tris-Borate-EDTA buffer poured onto the electrophoresis tray completely immersing the gel. A mixture of 8µl of sample and 2µl of gel loading buffer dye (5X) was then loaded into the agarose gel wells using a micropipette. In addition to sample, positive and negative control samples obtained from the WHO HCV reference laboratory were also added in the same manner as the samples. A 100bp DNA molecular weight marker (New England Biolabs) was added to an adjacent well to enable size estimation of the resolved bands. The gel was left to run for 45 minutes at 100 volts. At the end of the 45 minutes, the gel was placed on an ultra violet (UV) illuminator to visualise the bands and a digital image of the gel captured. 3.5.4 Purification of PCR products The PCR amplicons were purified using the QIAquick PCR Purification kit (Qiagen, Hilden, Germany) following manufacturer’s instructions. In summary, 500µl of buffer PB was mixed with approximately 92µl of amplicon left after electrophoresis. A QIAquick column was then 27 placed in a 2ml collection tube and to this was added the sample mixture followed by centrifugation at 17,900g for 1 min. The flow through was discarded and the QIAquick column placed back into the emptied collection tube. Buffer PE (750µl) was added to the QIAquick column and centrifuged at 17,900g for one minute. The flow through was discarded again and the QIAquick column placed in a 1.5ml centrifuge tube. Elution buffer EB (30µl), provided in the kit insert, was then added to the center of the QIAquick column, incubated for 1 minute and then centrifuged at 17,900g for one minute. The purified product was then sequenced. 3.5.5 DNA sequencing Sequencing was done using the Beckman Coulter 8000 genetic analysis system machine and sequences analysed using the sequencher software version 4.6. In summary, reaction mix was made by mixing 1.0µl of the cleaned DNA template with 1.0µl of the secondary PCR primers 5’-CAT AGC CTC CGT GAA GRC TC-3’ and 5’-TAT GAY ACC CGC TGY TTT GAC TC-3’(5µM) and 8.0µl of DTCS Quick start Master mix (Beckman Coulter, Fullerton, CA). This mix was then placed in a PCR thermocyling machine. The program used was denaturation at 96oC for 30 seconds, annealing at 50 oC for 15 seconds and extension at 60oC for 4 minutes. This cycle was repeated 29 times cycles after which samples were held at 4oC for up to 16 hours. The PCR reaction mixture was cleaned by ethanol precipitation. In summary, the PCR reaction was first stopped using a mixture of 2µl of 3M Sodium acetate (pH 5.2), 2µl of 100 28 mM Na2-EDTA (pH 8.0) and 1µl of 20 mg/ml of glycogen. This was followed by the addition of 70µl of 95% ethanol. The plate containing the samples was sealed using aluminum foil lids and vortexed for 5 seconds. It was then centrifuged at 3000g for 10 minutes after which the plate was gently tapped on tissue paper to remove excess ethanol. While still inverted and covered with tissue, the plate was centrifuged at 300g for 20 seconds. After this, 0.2ml of ice cold 70% ethanol was added and the sample centrifuged at 3000g for 3 minutes at 40C to repellet the DNA. The plate was then inverted on tissue paper to remove excess supernatant. The process of addition of 70% ethanol and centrifugation at 300g for 20 seconds was repeated. The samples were then dried under a vacuum for 30 minutes. 40µl of sample loading solution was then added to the pellet and mixed thoroughly for about 5 minutes. A drop of mineral oil was then added to the sample which was thereafter loaded on to the sequencing analyzer machine and the capillary electrophoresis program started. On completion of the program, the generated sequences were exported to the sequencher software version 4.6 from where they were edited. 3.5.6 Phylogenetic analysis Using the Clustal W software, NS5B gene sequences were aligned together with reference sequences obtained from the Los Alamos HCV sequence database. These sequences were manually edited to remove gaps and trimmed to identical sequences using BioEdit Version 7.0.5.3. Phylogenetic analysis was performed using the MEGA Version 4.0 software. The phylogenetic trees were estimated with the neighbour-joining methodology using the Tamura’s 3-parameter model of evolution. This model was selected using the jModelTest 29 software. The robustness and reliability of the tree was determined using bootstrap analysis with 1000 replicates. 3.5.7 HCV viral load testing HCV viral load testing was done by the staff of the National Health Laboratory Services (NHLS) in Johannesburg South Africa using the COBAS Ampliprep/Cobas Taqman analyser (Roche Diagnostics, Pleasanton, USA). This is an automated HCV RNA extraction instrument (COBAS AmpliprepTM) that is combined with a real time PCR machine, COBAS TaqManTM 48 analyzer. The HCV RNA extraction and PCR amplification and detection using the CAP/CTM HCV assay were done following manufacturer’s instructions. In brief, after setting up the Cobas Ampliprep instrument, it was loaded with the reagent cassettes and disposable items namely tips, sample processing units and sample tubes. The instrument was then started to begin the RNA extraction process. After extraction, the tubes containing the extracted RNA were transferred onto the Cobas Taqman 48 analyser to conduct the DNA amplification and detection procedures. At the end of the detection process, results are displayed on the computer in international units (IU). 3.6 Data quality control In all the assays used in this study, negative and positive quality control samples were included to validate the run. This applied to PCR, sequencing and viral load testing. Any runs in which these controls failed were repeated. 30 Samples used in this study were stored, shipped and handled in a way that ensured their integrity was not compromised at any stage. They were stored in -800C freezers that are temperature controlled and continuously monitored. The same applied to the freezers and fridges that stored the reagents and kits. The laboratories that conducted EIA testing are accredited in Good Clinical Laboratory practice (GCLP) by Qualogy Ltd, (UK) while the lab that conducted the viral load testing is also accredited in the International Standards Organization Standards (ISO) by the South African National Accreditation Scheme (SANAS). Extraction of RNA, PCR and sequencing were conducted in a laboratory accredited by the World Health Organisation. 3.7 Data analysis Enzyme immunoassay results were compared with both the PCR and HCV viral load results. Results were tabulated in a 2x2 contingency table. The Fisher’s exact test of association was used to compare antibody results to those of the in-house RT-PCR and the CAP/CTM HCV test. 31 CHAPTER FOUR RESULTS 4.1 Comparison of anti-HCV EIA results with RT-PCR results The figure below shows the agarose gel image of one of the PCR runs. Fig. 3: Agarose gel showing results for samples from Rwanda. The gel contained two rows of wells. The first row contained the samples while the second row contained the controls. Letters M, N and P represent the marker, negative control, and positive control, respectively. The numbers 1-15 represent the different samples run on this gel. Samples 1-5, 11, and 12 were HCV RNA positive. The amplified band product was 384bp. Out of the 151 anti-HCV EIA samples, only 9 samples (6%) were positive by the in-house RT-PCR assay. All the 16 anti-HCV EIA negative samples were RT-PCR negative (Table 4). Table 4. Contingency table of anti-HCV EIA results against PCR results PCR Positive PCR Negative EIA Positive 9 142 EIA negative 0 16 Total 9 158 Total 151 16 167 32 Using Fisher’s exact test of association to measure the correlation between EIA reactivity and in house RT-PCR positivity, the p-value at 5% level of significance was 0.603. 4.2 Comparison of anti-HCV EIA results with the real-time PCR results The real-time PCR results were similar to those obtained from the in-house RT-PCR. Only 9 out of 152 anti-HCV EIA positive samples had detectable HCV viral loads. All the 16 antiHCV EIA negative samples had undetectable HCV viral loads. Samples that were positive by the in-house RT PCR were those previously detected by the real-time PCR. The viral loads ranged from 19 IU/ml to 1,058,000 IU/ml as shown in table 5 below. The majority (seven) of the samples with detectable HCV RNA were from Rwanda. Table 5. HCV Viral loads of PCR positive samples by country of origin Agarose gel IDa Viral load (IU/ml) Sample Origin b Not applicable 19 Uganda 4 3,740 Rwanda 1 4,420 Rwanda 12 16,300 Rwanda 2 35,200 Rwanda 5 71,400 Rwanda Not applicableb 102,400 Uganda 11 684,000 Rwanda 3 1,058,000 Rwanda a Represents position of the sample on the agarose gel shown in Figure 3 b Samples from Uganda were run on two different gels A total of 12 out of 167 samples were not tested by real-time PCR due to control failure. Repeat testing was not possible due to lack of extra sample aliquots. All the failed 12 samples were in-house RT-PCR negative. 33 4.3 Types of HCV genotypes Sequencing and phylogenetic analysis of the PCR positive samples only identified HCV genotype 4. The phylogenetic tree in Figure 4 below shows the subtypes identified. Fig. 4: Phylogenetic analysis of HCV NS5b sequences. A neighbour-joining phylogenetic tree was built from isolates and reference sequences for the various HCV genotypes from the Los Alamos HCV sequence database. The Tamura 3-parameter method was used to estimate the genetic distances. The samples that were genotyped in this study are highlited in bold with the code_HCV. The Ugandan samples are 7449_HCV and 4211_HCV while the rest of the samples were from Rwanda 34 CHAPTER FIVE DISCUSSION Results from this study demonstrated a very poor correlation between EIA reactivity and the detection of HCV RNA. Only 9 (6%) of the 151 EIA-positive samples were positive by both the in-house RT-PCR and the CAP/CTM HCV real time PCR. Using Fisher’s exact test of association, the p-value at 5% level of significance was 0.603, indicating a lack of association between EIA reactivity and HCV RNA detection. These results are suggestive of a high false positive rate of the anti-HCV EIAs within the study population that cannot not be fully explained by other factors as discussed below. The poor correlation between EIAs and confirmatory testing has previously been reported in East Africa and this study provides further evidence of this. For example, a study conducted in Uganda among hospital patients recently reported that out of 166 anti-HCV EIA-3 positive samples, only 48 (29%) had detectable HCV RNA (Seremba et al., 2010). An earlier study also done in Uganda amongst blood donors found that out of 107 EIA positive samples, only 15 (16%) were positive and 47 (50%) indeterminate on RIBA (Hladik et al., 2006). In Tanzania, a positive predictive value of only 18.8% for the third generation anti-HCV EIA was reported among the general population (Tess et al., 2000). In India, a false positive rate of 82.4% and 78.5% as confirmed by PCR and immunoblot respectively was reported (Thakur et al., 2008; Raghuraman et al., 2003). These results contrast sharply with those in the developed countries where the specificity anti-HCV EIAs is reported to be very high (greater than 98%) (Colin et al., 2001; WHO, 2001). 35 False positive results in earlier generations of anti-HCV EIAs were attributed to non-specific antibody binding or possibly to cross-reactivity with other tropical pathogens such as other flaviviruses (McFarlane et al., 1990; Sonmez et al., 1997). Samples used in this study were not tested for the presence of other flaviviruses. However, in one of the studies done in Uganda, samples were tested for the West Nile Virus one of the most common flaviviruses in tropical Africa. None of the samples were positive for the flavivirus suggesting that crossreacting antibodies at least to this virus were unlikely (Seremba et al., 2010) but suggested that antibodies resulting from antigens unique to Uganda may be cross reacting with the hepatitis C virus. Another reason that was advanced for the high false positive rates of the anti-HCV EIAs was the high levels of serum IgG that cross-react with the antigens used in the EIAs. This hypergammaglobulinemia has been reported in tropical countries due to the endemic parasitic and infectious diseases found in this region (Raghuraman et al., 2003). The study population from which samples for this study were obtained had a high rate of infectious diseases. This was characterised by the high number of clinically asymptomatic participants excluded due to laboratory diagnosed infections (Stevens et al., 2008). These infections may have contributed to the high number of anti-HCV EIA reactive samples that could not be confirmed by HCV RNA tests in this study. Another possibility is that these participants were originally infected with HCV but it was eventually completely cleared from their blood. According to literature the HCV clearance rates in the blood varies from 14% to 46% (Seef, 2002) and may go as high as 60% (Caruntu & Benea, 2006). In Egypt, where HCV genotype 4 is the most dominant genotype by far, 36 HCV clearance rates were reported to be averaging 38.5% with more clearance being seen in women (44.6%) as compared to the men (33.7%) (Bakr et al., 2006). Although the hepatitis C virus may be cleared from the blood, it is almost always still present in the hepatocytes (Hoare et al., 2008). In fact, non viremic patients exposed to HCV have chronic low-level probably hepatic viral replication that is associated with a lower risk of progressive liver injury (Hoare et al., 2008). The hepatitis C virus has also been detected in the peripheral blood mononuclear cells of the majority of healthy patients who test positive for anti-HCV antibodies and have normal alanine aminotransferase (ALT) levels but who do not have HCV RNA detected in sera (Carreno et al., 2006). Hepatitis C virus clearance rates vary depending on a number of factors including age at time of infection, race, gender and development of symptoms at the time of infection (Chen & Morgan, 2006). This study did not investigate the extent to which each of these factors could have affected HCV clearance rates and subsequently EIA specificity. Viremia levels of the 9 samples with detectable viral loads ranged from 19 IU/ml to 1,058,000 IU/ml. Majority (8 out of 9) of these samples may thus be categorized as having had ‘low’ viral loads because they were below 800, 000IU/ml the recommended threshold between low and high viremia (Zeuzem et al., 2009). These viremia levels cannot be used to determine whether the samples were from persons in the acute or in the chronic phase of infection. Both phases can have similar viremia levels although the acute phase is characterised by large fluctuations in viremia levels over time (Caruntu & Benea, 2006). In this study, samples were 37 collected from a single time point hence viremia level fluctuations overtime were not measured. It should be pointed out that viremia levels do not correlate with the severity of hepatitis or with a poor prognosis (Seef, 2002). Viral load measurements are more commonly done to help in the monitoring of response to anti-viral therapy (Majid & Gretch 2002). In East Africa where treatment for HCV infection is rarely done, viral load measurement for clinical management is still of little relevance. This study demonstrated a 100% agreement between viral load testing (Real time PCR) and RT-PCR. Samples that were RT-PCR positive also had detectable HCV RNA using viral load testing. Much as the two methodologies are based on similar principles, improvements in real time PCR have made this test very sensitive. Automation of RNA extraction and detection clearly makes this test more robust and efficient when compared to the manual qualitative RT-PCR. Nevertheless, results from this study showed that the qualitative RT-PCR which is significantly cheaper than the real time PCR (USD30 vs. USD150) was adequately optimised to detect HCV RNA even at very low concentrations. This is because the sample with the lowest viral load of 19 IU/ml as reported by the real-time PCR test was readily detected by the in-house RT-PCR. Qualitative in-house RT-PCR can therefore be used to confirm anti-HCV EIA results in resource limited countries like those of East Africa instead of using the more expensive real time PCR. The sample size used in this study was however too small to provide conclusive results in this respect. This study identified only genotype 4 in samples from Uganda and Rwanda. This finding is consistent with previous studies (Biggar et al., 2006; Muasya et al., 2008). The two samples 38 from Uganda clustered in the same subgroup with four samples from Rwanda (Figure 4). The remaining three Rwandese samples clustered in a different sub group. The identification of similar HCV genotypes in these two countries is not surprising. This can be attributed to their close proximity and substantial interaction amongst its people. The HCV subtypes that were identified clustered with those that have been found in Cameroon. Genotype 4 is commonly found in West and Central Africa where it is postulated to have spread eastwards (Ndjomou et al., 2003). Failure to identify other genotypes notably genotype 1 is also not suprising. This genotype which is prevalent in Europe was identified in Kenya amongst drug users (Muasya et al., 2008), a population different in nature from that used for this study. The small sample size used in this study might have been a factor that also limited the chances of identifying this or any other HCV genotypes. This study found that differences in the HCV genotype of the sample tested and the genotype of anti-HCV antigens used in the EIAs does not affect EIA performance. The anti-HCV EIAs that were used to screen these samples do not include antigens from genotype 4 whereas only genotype 4 was identified. This result is important because some authors suggested that antiHCV EIA sensitivity is affected by the genotype diversity of the antigens used in the immunoassays. Specifically, the core, NS3, NS4, and NS5 have been reported to show antigenic variation among the different genotypes (Neville et al., 1997). By comparing the serological reactivities of sera to type-homologous and type heterologous antigens, significant type-specific component to the reactivity to NS3 and NS5 was detected 39 (Neville et al., 1997). A fivefold weaker reactivity of sera from HCV type 2- and HCV type 3-infected blood donors in the EIA-3 has been previously reported, suggesting that this EIA was suboptimal for screening populations in which the predominant genotype is not type 1 (Dhaliwal et al., 1996). On the other hand, other studies have found that with the EIA-3, genotype differences do not significantly affect EIA performance (Maggi et al., 1995; Pawlotsky et al., 1995). The combination of core, NS3, NS4, and NS5 antigens in current EIA-3 assays have enough cross-reacting epitopes for all genotypes (Sheiblauer et al., 2006). In summary, this study has shown that the kits that were used to screen for HCV in the samples used for this study are adequate in detecting this infection in samples from East Africa even though giving a high number of potentially false positives. It is, therefore, not necessary to design anti-HCV EIAs using antigens from HCV genotype 4 in areas where this genotype is the most prevalent one. 40 CHAPTER SIX CONCLUSIONS AND RECOMMENDATIONS 6.1 Conclusions This study showed that there is a very poor correlation between anti-HCV EIA reactivity and the detection of HCV RNA in serum samples from East Africa. Only 6% of anti-HCV EIA reactive serum samples from East Africa contain detectable viral RNA. Genotype 4 is the most common HCV genotype in anti-HCV EIA reactive serum samples in East Africa. However, because of the small sample size of this study, (nine samples genotyped), this finding is not definitive. This study also suggested that HCV genotype 4 is readily detected by non-genotype 4 antigen HCV EIAs although with a very high number of potentially false positives. There is a perfect agreement between the in-house RT-PCR and real-time PCR. Either method could be used to detect HCV RNA in serum samples. The small sample size of this study however makes this conclusion not definitive. 6.2 Recommendations A cost effective HCV testing algorithm should be developed for use in East Africa. Anti-HCV positive samples should be confirmed with more specific tests like HCV RNA detection/quantification assays. An in-house RT-PCR is a reliable confirmatory test that may be used in place of the more robust but more expensive commercial real time PCR assays. 41 The anti-HCV EIAs that were used to screen samples used in this study may not be specific enough to be recommended for use in this region. However, additional studies are required to confirm these findings using a larger sample size. Further investigations are required to examine the cause of the poor correlation between antiHCV EIA reactivity and HCV RNA detection in serum samples from East Africa. 42 CHAPTER SEVEN REFERENCES Abdel-Hamid, M., El-Daly, M., El-Kafrawy, S., Mikhail, N., Strickland, G.T. & Fix A.D. (2002). Comparison of second- and third-generation enzyme immunoassays for detecting antibodies to hepatitis C virus. Journal of Clinical Microbiology, 40(5), 1656-1659. Abrignani, S., Houghton, M. & Hsu, H.H. (1999). Perspectives for a vaccine against hepatitis C virus. Journal of hepatology, 31, 259-263. Alberts, B., Lewis, J., Raff. M., Roberts, K. & Walter, P (2007). Molecular Biology of the Cell. (5th ed.). New York, Garland Science. Alter, H.J. (1992). New kit on the block: Evaluation of second-generation assays for detection of antibody to the hepatitis C virus. Hepatology, 15, 350-353. Alter, M. J. (2007). Epidemiology of Hepatitis C Virus Infection. World Journal of Gastroenterology, 13(17), 2436-2441. Apurva, A. & Jordan, J. F. (2007). Viral hepatitis and HIV in Africa. AIDS Reviews, 9, 25-39 Ayolabi, C. I., Taiwo, M. A., Omilabu, S. A., Abebisi, A. O. & Fatoba, O. M. (2006). Seroprevalence of hepatitis C among blood donors in Lagos, Nigeria. African Journal of Biotechnology, 5(20), 1944-1946. Bakr, I., Rekacewicz, C., El Hosseiny, M., Ismail, S., El Daly, M., El-Kafrawy, S., Esmat, G., Hamid, M. A., Mohamed, M.K. & Fontanet, A. (2006). Higher clearance of hepatitis C virus infection in females compared with males. Gut, 55, 1183–1187. 43 Benhamou, Y., Bochet, M., Di Martino, V., Charlotte, F., Azria, F., Coutellier, A., Vidaud, M., Bricaire, F., Opolon, P., Katlama, C., Poynard, T. (1999). Liver fibrosis progression in HIV and HCV co-infected patients. The Multivirc Group. Hepatology, 30, 1054-8. Biggar, R. J., Oritz-Conde, B.A., Bagni, R.K., Bakaki, P.M., Cheng-Dian, W., Engels, E.A. & Mbulaiteye, S.M. (2006). Hepatitis C virus genotypes in Ugandan children and their mothers. Emerging Infectious Diseases, 12(9), 1440-1443. Callahan, J.D., Constantine, N.T., Kataaha, P., Zhang, X., Hyams, K.C. & Bansal, J. (1993). Second generation hepatitis C virus assays: performance when testing African sera. Journal of Medical Virology, 41(1), 35-8. Carreno, V., Pardo, M., Lopez-Alcorocho, J.M., Rodriguez-Inigo, E., Bartolome, J. & Castillo, I. (2006). Detection of hepatitis C virus (HCV) RNA in the liver of healthy, antiHCV antibody positive, serum HCV RNA-negative patients with normal alanine aminotransferase levels. Journal of infectious diseases, 194, 53-60. Caruntu, F.A. & Benea, L. (2006). Acute Hepatitis C Virus Infection: Diagnosis, Pathogenesis, Treatment. Journal of Gastrointestinal and Liver Diseases 15 (3), 249-256. Chen, L.S. & Morgan, R.T. (2006). The Natural History of Hepatitis C Virus (HCV) infection. International Journal of Medical Sciences, 3(2), 47-52. Chevaliez, S. & Pawlotsky, J.M. (2006). HCV genome and life cycle. In S.L. Tan (Ed.). Hepatitis C viruses: Genomes and molecular biology, Norfolk: Horizon Bioscience. 5-47. Choo, Q.L., Kuo G., Weiner, A.J., Overby, L.R., Bradley, D.W. & Houghton, M. (1989). Isolation of cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science, 244, 359-62. 44 Colin, C., Lanoir, D., Touzet, S., Meyaud-Kraemer, L., Bailly, F and Trepo, C. (2001). Sensitivity and specificity of third-generation hepatitis C virus antibody detection assays: analysis of the literature. Journal of Viral Hepatitis, 8, 87-95. Courouce, A.M, Janot C & The hepatitis Study Group of the French Society of Blood Transfusion. (1991). Recombinant immunoblot assay first and second generations on 732 blood donors reactive for antibodies to hepatitis C virus by ELISA. Vox Sang, 1: 177-180. Courouce, A.M., Le Marrec, N., Girault, A., Ducamp, S & Simon N. (1994). Anti-hepatitis C virus (anti-HCV) seroconversion in patients undergoing hemodialysis: comparison of secondand third-generation anti-HCV assays. Transfusion, 34(9), 790-5. Davidson, F., Simmonds, P., Ferguson, J. C., Jarvis, L. M., Dow, B.C., Follett, E.A.C., Keller, A.J., Krusius, T., Lin, C., Medgyesi, G.A., Kiyokawa. H., Olim, G., Duraisamy, G., Cuyvers, T., Saeed, A. A., Ted, D., Conradie, J., Kew, M. C., Lin, M., Nuchaprayoon, C., Ndimbie, O.K. & Yap, P.l. (1995). Survey of major genotypes and subtypes of hepatitis C virus using RFLP of sequences amplified from the 5' non-coding region. Journal of General Virology, 76, 119-1204. Dhaliwal, S.K., Prescott, L.E., Dow, B.C., Davidson, F., Brown, H., Yap, P.L., Follett, E.A. & Simmonds, P. (1996). Influence of viraemia and genotype upon serological reactivity in screening assays for antibody to hepatitis C virus. Journal of Medical Virology, 48,184-190. Forns, X. & Bukh, J. (1998). Methods for determining the hepatitis C virus genotype. Viral Hepatology. 4:1-19. Galel, S.A., Strong, D.M., Tegtmeier, G.E., Holland, P.V., Kuramoto, I.K., Kemper, M., Piertrelli, L & Gallarda, J. (2002). Comparative yield of HCV RNA testing in blood donors screened by 2.0 versus 3.0 antibody assays. Transfusion, 42(11), 1507-1513. 45 Han, J. H., Shyamala, V., Richman, K. H., Brauer, M. J., Irvine, B., Urdea, M. S., Tekamp Olson, P., Kuo, G., Choo, Q. L. & Houghton, M. (1991). Characterization of the terminal regions of hepatitis C viral RNA: identification of conserved sequences in the 5' untranslated region and poly (A) tails at the 3' end. Proceeding from the National Academy of Sciences of the USA 88, 1711-1715. Hayashi, J., Nakashima, K., Kishihara, Y Ohmiya, M., Yoshimura, E., Hirata, M. & Kashiwagi, S. (1993). Improved detection of antibodies to hepatitis C virus by second generation assay in patients with chronic non-A, non-B liver disease. Journal of Infectious Diseases, 26, 287-294. Hladik, W., Kataaha, P., Mermin. J., Purdy, M., Otekat, G., Lackritz, E., Alter, M.J. & Downing, R. (2006). Prevalence and screening costs of hepatitis C virus among Ugandan blood donors. Tropical Medicine and International Health, 11(6), 951-954. Hoare, M., Gelson, T.H.W., Rushbrook, S.M., Curran, M.D., Woodall, T., Coleman, N., Davies, S. E. & Graeme, J. M. A. (2008). Histological changes in HCV antibody positive, HCV RNA–negative subjects suggest persistent virus infection. Hepatology, 48, 1737-1745. Jeannel, D., Fretz, C., Traore, Y Kohdio, N., Bigot, A., Pê Gamy, E., Jourdan, G., Kourouma, K., Maertens, G., Fumoux, F., Fournel, J.J. & Stuyver, L (1998). Evidence for high genetic diversity and long-term endemicity of hepatitis C virus genotypes 1 and 2 in West Africa. Journal of Medical Virology, 55, 92–97. Kuiken, C., Yusmin, K., Boykin, L. & Richardson, R. (2005). The Los Alamos hepatitis C sequence database. Bioinformatics. 21(3), 379-384. Kuo, G., Choo, Q.L., Alter, H.J., Gitnick, G.L, Redeker, A.G., Purcell, R.H., Miyamura, T., Dienstag, J.L., Alter, M.J., Stevens, C.E. Tegteimer, G.E, Bonino. F., Colombo, M., Lee, W.S, Berger, K., Shuster, J.R, Overby, L.R, Bradley, D.W & Houghton, M. (1989). An assay 46 for circulating antibodies to a major etiologic virus of human non-A, non-B hepatitits. Science, 244, 362-364. Laurent, C., Henzel, D., Mulanga-Kabeya, C., Maertens, G., Larouze, B., Delaporte, E. (2001). Seroepidemiological survey of hepatitis C virus among commercial sex workers and pregnant women in Kinshasha, Democratic Republic of Congo. International Journal of Epidemiology, 30, 872–77. Lin, C., Lindenbach, B. D., Pragai, B. M., McCourt, D. W. & Rice, C. M. (1994). Processing in the hepatitis C virus E2–NS2 region: identification of p7 and two distinct E2-specific products with different C termini. Journal of Virology, 68, 5063–5073. Lionis, C., Vlachonikolis, I.G., Skliros, S., Symeonidis, A., Merkouris, B.P. Kouroumalis, E and the Hepatitis C working group of the Greek General Practitioners. (2000). Do undefined sources of hepatitis C transmission exist? The Greek Study in general practice. Journal of Viral Hepatitis, 7, 218-224. Lunel, F., Rosenheim, M., & Duneton P. (1996). Proposition pour une stratégie d'évaluation et d'utilisation des tests de déspistage de l'hépatite C. Transfusion Clinique et Biologique 5, 279-288. MacDonald, M., Crofts, N. & Kaldor, J. (1996). Transmission of hepatitis C virus: Rates, routes and cofactors. Epidemiologic Reviews, 18 (2), 137-148. Madhava, V., Burgess. C., Drucker, E. (2002). Epidemiology of chronic hepatitis C virus infection in sub-Saharan Africa. The Lancet infectious diseases, 2, 293-302. Maggi, F., Vatteroni, M.L., Pistello, M., Avio, C.M., Cecconi, N., Panicucci, F. & Bendinelli, M. (1995). Serological reactivity and viral genotypes in hepatitis C virus infection. Journal of Clinical Microbiology, 33(1), 209-211. 47 Majid, A.M. & Gretch, D.R. (2002). Current and future hepatitis C virus diagnostic testing: problems and advancements. Microbes and Infection, 4, 1227-1236. McFarlane. I.G., Smith. H.M., Johnson, P.J., Bray, G.P., Vergani, D.,Williams, R. (1990). Hepatitis C virus antibodies in chronic active hepatitis: Pathogenetic factor or false-positive result? Lancet, 335, 754–757. McOmish, F., Yap, P.L., Dow, B.C., Follett, E.A., Seed. C., Keller, A.J., Cobian, T.J., Krusius, T., Kolho, E., Naukkarinen, R., Lin, C., Lai, C., Leong, S., Mdyesi, G.A., Hejjas, M., Kiyokawa, H., Fukada, K., Cuypers, T., Saeed, A.A., Al-Rasheed, A.M., Lin, M. & Simmonds, P. (1994). Geographical distribution of hepatitis C virus genotypes in blood donors: an international collaborative survey. Journal of Clinical Microbiology, 32, 884–92. Mejri, S., Salah, B. A., Triki, H., Alaya, B.N., Djebbi, A., Dellagi, K. (2005). Contrasting patterns of hepatitis C virus infection in two regions from Tunisia. Journal of Medical Virology, 76, 185-193. Mellor, J., Holmes, E. C., Jarvis, L. M., Yap, P. L., Simmonds, P and The International HCV Collaborative Study Group. (1995). Investigation of the pattern of hepatitis C virus sequence diversity indifferent geographical regions: implications for virus classification. Journal of General Virology, 76, 2493-2507. Menendez, C., Sanchez-Tapias, J.M., Kahigwa, E., Mshinda, H., Costa, J., Vidal, J., Acosta, C., Lopez-Labrador, X., Omeldo, E., Navia, M., Tanner, M., Rhodes, J., Alonso, L.P. (1999). Prevalence and mother-to-infant transmission of hepatitis viruses B, C and E in Southern Tanzania. Journal of Medical Virology, 58 (3), 215-220. Mizushima, H., Hijikata, M., Asabe, S., Hirota, M., Kimura, K. & Shimotohno, K. (1994). Two hepatitis C virus glycoprotein E2 products with different C termini. Journal of Virology, 68(10), 6215-6222. 48 Morishma, C. & Gretch, D.R. (1999). Clinical use of hepatitis C virus tests for diagnosis and monitoring during therapy. Clinics in Liver Disease, 3(4), 717-40. Muasya, T., Lore, W., Yano, K., Yatsuhashi, H., Owiti, F.R., Fukuda, M., Tamada, M.Y., Kulundu, J., Tukei, J. & Okoth, F.A. (2008). Prevalence of hepatitis C virus and its genotypes among a cohort of drug users in Kenya. East African Medical Journal, 85(7), 318-25. Muerhoff, A.S., Jiang, L., Shah, D.O., Gutierrez, R.A., Patel, J., Garolis, C., Kyrk, C.R., Leckie, G., Frank, A., Stewart, J.L, & Dawson, G.J. (2002). Detection of HCV core antigen in human serum and plasma with an automated chemiluminescent immunoassay. Transfusion. 42(3), 349-56. Nakagiri, I., Ichihara, K., Ohmoto, K., Hirokawa, M. & Matsuda, N. (1993). Analysis of discordant test results among five second-generation assays for anti-hepatitis C virus antibodies also tested by polymerase chain reaction RNA assay and other laboratory and clinical tests for hepatitis. Journal of Clinical Microbiology, 31, 2974-2980. Nakao, T. N., Enomoto, N., Takada, A., Takada, & Date, T. (1991). Typing of hepatitis C virus (HCV) genomes by restriction fragment length polymorphisms. Journal of General Virology 72, 2105-2112. Ndumbe, P.M. & Skalsky, J. (1993). Hepatitis C virus infection in different populations in Cameroon. Scandinavian Journal of Infectious Diseases, 25, 689–692. Ndumbe, P.M., Skalsky, J. & Joller-Jemelka, H.I. (1994). Seroprevalence of hepatitis and HIV infection among rural pregnant women in Cameroon. Apmis, 102, 662–666. Nakatani, S.M., Santos. C.A., Riediger, I.N., Krieger, M.A., Duarte C.A.B, Lacerda, M.A., Biondo, A.W., Carilho, F.J. & Ono-Nita, S.K. (2010). Development of Hepatitis C Virus Genotyping by Real-Time PCR Based on the NS5B Region. PLoS ONE 5(4): e10150. doi:10.1371/journal.pone.0010150. 49 Ndjomou J., Pybus, O.G. & Matz, B. (2003). Phylogenetic analysis of hepatitis C virus isolates indicates a unique pattern of endemic infection in Cameroon. Journal of General Virology, 84, 2333-41. Neville, J.A., Prescott, L. E., Bhattacherjee, V., Adams, N., Pike, I., Rodgers, B., El-Zayadi, A., Hamid, S., Dusheiko, G.M., Saeed, A. A., Haydon, G.H. & Simmonds, P. (1997). Antigenic variation of core, NS3, and NS5 proteins among genotypes of hepatitis C virus. Journal of Clinical Microbiology, 35(12), 3062-3070. Njouom, R., Pasquier, C., Ayouba, A., Sandres-Saune´, K., Mfoupouendoun, J., Lobe, M.M., Tene, G., Thonnon, J., Izopet, J. & Nerrienet, E. (2003). Hepatitis C virus infection among pregnant women in Yaounde, Cameroon: Prevalence, viremia, and genotypes. Journal of Medical Virology, 69, 384–390. Okamoto, H., Okada, S., Sugiyama, Y., Yotsumoto, S., Tanaka, T., Yoshizawa, H., Tsuda, F., Miyakawa, Y. & Mayumi, M. (1990). The Y-terminal sequence of the hepatitis C virus genome. Japanese Journal of Experimental Medicine, 60, 167-177. Oni, A.O. & Harrison, T.J. (1996). Genotypes of hepatitis C in Nigeria. Journal of Medical Virology, 49(3), 178-86. Pawlotsky, J., Lonjon, I., Hezode, C., Raynard, B., Darthuy, F., Remire, J., Soussy, C. & Dhumeaux, D. (1998). What strategy should be used for the diagnosis of hepatitis C virus infection in clinical laboratories? Hepatology 27, 1700-1702. Pawlotsky, J., Roudot-Thoraval, F., Pellet, C., Aumont, P., Darthuy, F., Remire, J., Duval, J., Dhumeaux, D. (1995). Influence of hepatitis C virus (HCV) genotypes on HCV recombinant immunoblot assay patterns. Journal of Clinical Microbiology, 33(5), 1357-1359. Puoti, M., Bonacini, M., Spinetti, A., Putzolu, V., Govindarjan, S., Zaltron, S., Favret, M., Callea, F., Gargiulo, F., Donato, F., Carosi, G. (2001). Liver fibrosis progression is related to 50 CD4 cell depletion in patients co-infected with HCV and HIV. Journal of Infectious Diseases, 183, 134-7. Raghuraman, S., Subramaniam, T., Daniel, D., Sridharan, G. & Abraham, P. (2003). Occurrence of False Positives during Testing for Antibodies to Hepatitis C Virus among Volunteer Blood Donors in India. Journal of Clinical Microbiology, 41 (4) 1788–1790. Ramarokoto, C.E., Rakotomanana, F., Ratsitorahina, M., Raharimanga, V., Razafindratsimandresy, R., Randremanana, R., Rakoto-Andrianarivelo, M., Rousset, D., Andrianaja, V., Richard V, Soares, J.L. & Rabarijaona, L.P. (2008). Seroprevalence of hepatitis C and associated risk factors in urban areas of Antananarivo, Madagascar. BMC Infectious Diseases 2008, 8:25 doi:10.1186/1471-2334-8-25. Read, S.J. (2001). Recovery efficiencies of nucleic acid extraction kits as measured by quantitative LightCyclerTM PCR. Journal of Clinical Pathology, 54, 86-90. Sanger. F., Nicklen, S., Coulson, A.R. (1977). DNA sequencing with chain-terminating inhibitors. Proceedings of the National Academy of Sciences of the United States of America, 74(12), 5463–5467. Sarrazin, C., Dragan, A., Gärtner, B.C., Forman, M. S., Traver, S., Zeuzem, S. & Valsamakis, A. (2008). Evaluation of an automated, highly sensitive, real-time PCR-based assay (COBAS AmpliprepTM/COBAS TaqManTM) for quantification of HCV RNA. Journal of Clinical Virology, 43, 162–168. Schreiber, G., Busch, M., Kleinman, S. & Korelitz, J. (1996). The risk of transfusiontransmitted viral infections. New England Journal of Medicine, 334, 1685-1690. Schroter, M., Schafer, P., Zollner, B., Polywka, S., Laufs, R., & Feucht, H.H. (2001). Strategies for reliable diagnosis of hepatitis C infection: the need for a serological confirmatory assay. Journal of Medical Virology, 64, 320-324. 51 Seef, B.L. (2002). Natural History of Chronic Hepatitis C. Hepatology, 36, 35-46. Seremba, E., Ocama, P., Opio, C.K., Kagimu, M., Thomas, D.L., Yuan, H.J., Attar, N. & Lee W.M. (2010). Poor Performance of Hepatitis C Antibody Tests in Hospital Patients in Uganda. Journal of Medical Virology, 82, 1371–1378. Sergio, O., Lima, C., Torres, M.P., Pereira, M.R.G., Lopes da Fonsecaa, B.A. (2004). OneStep RT-PCR protocols improve the rate of dengue diagnosis compared to Two-Step RT-PCR approaches. Journal of Clinical Virology, 30(4), 297-301. Scheiblauer, H., El-Nageh, M., Nick, S., Fields, H., Prince, A. & Diaz, S. (2006). Evaluation of the performance of 44 assays used in countries with limited resources for the detection of antibodies to hepatitis C virus. Transfusion Complications, 46, 708-718. Simmonds, P. (1995). Variability of hepatitis C virus. Hepatology, 21, 570-583. Simmonds, P., Holmes, E. C., Cha, T. A., Chan, S. W., McOmish, F., Irvine, B., Beall, E., Yap, P. L., Kolberg, J. & Urdea M. S. (1993). Classification of hepatitis C virus into six major genotypes and a series of subtypes by phylogenetic analysis of the NS-5 region. Journal of General Virology, 74, 2391-2399. Smith, L.M., Sanders, J.Z., Kaiser, R.J., Hughes. P., Dodd, C., Connell, C.R., Heiner, C., Kent, S.B. & Hood, L.E. (1986). Fluorescence detection in automated DNA sequence analysis. Nature, 321 (6071), 674-9. Smuts, H.E. & Kannemeyer, J. (1995). Genotyping of hepatitis C virus in South Africa. Journal of Clinical Microbiology, 33(6), 1679-81. Sonmez, E., Ozerol, I.H., Senol, M., Kizilkaya, N., Sahin, K., Ozbilge, H. (1997). Falsepositive reaction between syphilis and hepatitis C infection. Israel Journal of Medical Sciences, 33,724–727. 52 Stevens, W., Kamali, A., Karita, E., Anzala, O., Sanders, E.J. Jaoko, W., Kaleebu, P., Mulenga, J., Dally, L., Fast, P., Gilmour, J., Farah, B., Birungi, J., Hughes, P., Manigart, O., Stevens, G., Yates, S., Thomson, H., Von-Lieven, A., Krebs, M., Price, A.M, Stoll-Johnson, L. & Ketter, N. (2008). Baseline morbidity in 2900 adult African volunteers recruited to characterise laboratory reference intervals for future HIV vaccine clinical trials. PLOS ONE 3(4): e20243: doi:10.1371/Journal.pone.0002043. Tamura, K., Dudley, J., Nei, M. & Kumar, S. (2007). MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Molecular Biology and Evolution 24, 15961599. Tess, B.H., Levin, A., Brubaker, G., Shao, J., Drummond, J. E., Alter, J.H. & O’brien, R.T. (2000). Seroprevalence of Hepatitis C Virus in the general population of Northwest Tanzania. American Journal of Tropical Medicine and Hygiene, 62(1), 138–141. Thakur, V., Guptan, R.C., Arankale, V. & Sarin, S.K. Low specificity of the third generation ELISA for HCV detection in voluntary blood donors in India. (n.d.). Journal of the international federation of clinical chemistry and Laboratory medicine, 14, (1). Retrieved on [July 31, 2008] from http://www.ifcc.org/PDF/140103200305.pdf. Van der Poel, C.L., Cuypers, H.T. & Reesink, H.W. (1994). Hepatitis C virus six years on. Lancet, 344, 1475-1479. Vermehren, J., Kau, A., Ga¨rtner, B. C., Go¨bel, R, Zeuzem, S. & Sarrazin, C. (2008). Differences between two real-time PCR-based hepatitis C virus (HCV) assays (Real-Time HCV and Cobas AmpliPrep/CobasTaqMan) and one signal amplification assay (Versant HCV RNA 3.0) for RNA detection and quantification. Journal of Clinical Microbiology, 46(12), 3880–3891. Weiner, A. J., Brauer, M. J., Rosenblatt, J., Richman, K. H., Tung, J., Crawford, K., Bonino, F., Saracco, G., Choo, Q.L., Houghton, M. & Han, J. H. (1991). Variable and hypervariable 53 domains are found in the regions of HCV corresponding to the flavivirus envelope and NS1 proteins and the pestivirus envelope glycoproteins. Virology, 180, 842-848. WHO (2001) Hepatitis C Assays: Operational Characteristics Phase 1 Report 2. [Electronic publication] Retrieved on [August 4 2008] from http://whqlibdoc.who.int/hq/2001/WHO_BCT_BTS_01.5.pdf. WHO (2009). Global distribution of HCV Genotypes. [Electronic publication] Retrieved on [June 10 2010] from http:// www.who.int/vaccine_research/documents/ViralCancer7.pdf. WHO and The viral hepatitis prevention Board (1999). Global Surveillance and control of hepatitis C. Journal of Viral Hepatitis, 6, 35-47. Zein, N.N. (2000). Clinical significance of hepatitis C virus genotypes. Clincal Microbiology Reviews, 13, 223-235. Zekri A.R.N, Alam, E.H.M, Bahnassy, A.A, El-Shehabi, A.M.R, El-Leethy H., Omar S., Khaled, H.M. (2005). TRUGENE sequencing versus INNO-LiPA for sub-genotyping of HCV genotype 4. Journal of Medical Virology, 75, 412-420. Zeuzem, S., Berg, T., Moeller, B., Hinrichsen, H., Mauss, S., Wedemeyer, H., Sarrazin, C., Hueppe, D., Zehnter, E., & Manns, M.P. (2009). Expert opinion on the treatment of patients with chronic hepatitis C. Journal of Viral Hepatitis, 16, 75–90. 54