Autopsy Manual
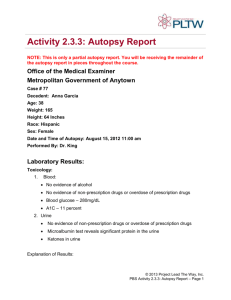
advertisement

1 THE AUTOPSY MANUAL The Beth Israel Deaconess Medical Center- Department of Pathology Revised and Adopted: June 2003 / WCQ October 2003 / JLH June 2004 / JLH June 2006 / JLH Updated by: Jonathan L. Hecht MD PhD; Jeffery Joseph MD, PhD; (Original version by Peter Ciano MD; William C. Quist MD PhD; Melissa Upton MD) Phone/pager Numbers (75)4-XXXX, (63)2-XXXX, (66)7-XXXX, (outside page) 632-7243: East Morgue 667-5783 West Morgue 632-9018 Jonathan Hecht, M.D., Ph.D. (Director) Beeper # 39030 Jeffery Joseph, M.D., Ph.D.(Neuropath.) Beeper # 35290 Autopsy secretary (Chris Sturdivant) 667-5759 Autopsy supervisor (Gail Howe) Beeper # 31426 Deiner (Emerson Springer) Beeper # 92588 2 Autopsy Check list: Autopsy # : A____-_________ Pt. Name:____________________________________MRN:_________________ The following things must be done prior to beginning an autopsy: Check off every box after it has been performed and sign below: Log in the case into the autopsy log under the next sequential number. Speak with an involved clinician and discuss the case. Write down the major questions for autopsy on the permit. Ask if any additional doctors need a copy of the report, and list them on your PAD. Go over the permission with attending (Is this an ME case? Do the organs have to be returned to the body? Who needs a copy of the report?) Go over the restrictions and major questions with attending Consult relevant staff (IS for medical renal, JJ for Neuro issues). Make extra copies of the following and take them with you to the autopsy suite 1. Permission form 2. Certificate of death Compare all of the deceased IDs with the permission form and certificate of death making sure they match before beginning the autopsy Return the signed original report of death and permit to Admitting, after you complete the autopsy. I have performed the above: _________________________________________________________ Name (Resident) date Return this completed form along with copies of the permission form to Chris Sturdivant. Return the chart to medical records when you have finished your review. 3 Basics: 1) Follow the above checklist (most items precede the dissection). 2) If you have any questions or complications before during or after the autopsy page your assigned attending, chief resident or director of autopsy. You should never feel like you’re working on your own. 3) Document findings in detail (the form on the next page may be helpful). Photograph all abnormalities before they are sectioned/destroyed. Perinatal photographs are required on all cases (abnormal or not). 4) Start promptly; do not spend more than 30 minutes with the chart and getting hold of clinicians. The Deiner does not determine the start of the autopsy. If he is not available at the appointed time, report him to his supervisor (Gail Howe) and begin on your own. 5) Do not take chances with your safety, and call for back-up early if you get confused (there is no such thing as a 5 hr post). 6) Be prompt with your PAD/FAD. These documents must not be vague, but also must address clinical questions directly- describe what is seen and try to make conclusion in the final summary Autopsy Service Coverage 1) Every day 8:00am - 3:00pm unless you make special arrangements. Weekends 8:00am - 3:00pm. The weekend staff member on-call is responsible for any autopsy done on a weekend. They are responsible for supervising the dissection and signing out the PAD/FAD unless they make other arrangements. That attending is requested to attend or to send a representative to autopsy conference on the following Thursday 2) We accept outside cases if the patient has a BIDMC number and a contact clinician either here or at a nursing facility. Do not accept any other outside cases (i.e. death at home) without involving the autopsy director. 3) The deiner is usually available, but should not be the source of delay – if you need to eviscerate, do so (ask your chief or senior for help). If possible, arrange the autopsy start time with his supervisor (Gail Howe). 4) Talk to clinicians, not families (get your attending involved if this comes up) Examination of the Autopsy Permission FormDo not accept a form from Admitting that lacks signature of family/next-of-kin, or the signature of the pronouncing physician. All cases of a medical-legal nature should be cleared by the Medical Examiner, who may accept or waive the case. If you call the medical examiner, document the interaction on the report of death in the appropriate section of the Report of Death. Be clear on restrictions. These may be specific and written in the “SPECIFIC RESTRICTIONS OR REQUESTS” section of the Permit or generic (check-boxes on form) in the “Disposition of organs” section of the Permit. Division of Labor 1) The resident performs an external exam as the deiner is transferring the body to the table. 2) The deiner usually eviscerates, but the resident must supervise and verify his work (i.e. forgetting to take the prostate is the resident’s fault). The resident MUST be in the room during the entire autopsy. 3) The deiner cleans the autopsy room each week, but not after each case. You will be cleaning up your dissection area. 4) For West Campus cases, the deiner is expected to transport the organs to the East morgue within 24 hrs. Associated conferences (Thursday 11AM Gross and monthly Gross-micro). 4 NAME:___________________________________________________ AUTOPSY#______________ Length/Height: Weight: Hair (color/length): Skin: Eyes (pupils/color): Ears: Teeth: Nose: Genitals: Extermities: Personal Objects: Brain wt (g)/findings: NECK & THORAX Pleural: L(ml): Type of fluid: Adhesions: R (ml): Thyroid (g): Breasts: ABDOMEN Peritoneal (ml): Type of fluid: Adhesions: GI TRACT Esophagus: Adrenals: L(g): R(g): Stomach: (contents): Gallbladder: (Contents(ml/stones)): Liver (g): (Parenchyma): Trachea Lungs: L(g): Parenchyma: Bronchi: Arteries: Nodes: Small intestine: R(g): Spleen (g): Pancreas: Kidneys: L(g): Cortex: Medulla: Ureters/bladder: Prostate (size): R(g): Colon/rectum: Pericardium (ml): Adhesions/open: Diverticula: Testes: L (g): Heart (g): Dominance (L/R): Walls (cm): LV: Valves: TV: PV: Atherosclerosis: Systemic: Coronary(%): RT: Lt. Main: LAD: Circ: Lymph nodes: Muscle/skeletal: RV: MV: AV: R(g): Uterus & Cervix: Tubes: Ovaries: L: R: Appendix: BABIES (cm) CR: Foot: Head circum: Cord: CH: 5 TABLE OF CONTENTS PAGE 1. Introduction 6 2. Autopsy Service Coverage 7 3. Preparation for the Autopsy- Review of Permit and Restrictions 7 4. Safe Performance of Autopsies and Handling of Tissues and Formalin 10 5. Infection Control Guidelines 11 6. Autopsy Room: General Overview and Division of Labor 13 7. Autopsies on Patients Who Die Outside the Beth Israel Deaconess Medical Center 14 8. Medical Examiner’s Cases 15 9. Ancillary Studies 17 10. Organ Donation 21 11. The Complete Adult Autopsy- detailed procedure 21 11a. Cardiac Exam 23 12. Stock Bottle & sections. 29 13. Autopsy Neuropathology 29 14. Recording the Cause of Death 32 15. Reviewing the Case with Staff pathologist, Sectioning, and Photography 33 16. Preparation of Autopsy Documents 34 17. Communication of Autopsy Findings 34 18. Infectious Autopsy 36 19. Severe Acute Respiratory Syndrome (SARS) Patients 39 20. Fetal/Neonatal Autopsy 41 20. Autopsy Conferences 53 21. Observers 53 22. Requests for Tissues for Research Purposes 53 23. Quality assurance 53 24. Templates (adult and fetal) 25. Appendices 46 6 Introduction This manual outlines the procedures and regulations pertaining to the various aspects of the Autopsy Service. While the manual is not meant to be exhaustive, it addresses most of the specific issues that relate to the autopsy. We have delineated in detail the entire autopsy process from the reception of the postmortem permission to completion of the final autopsy report. Questions not specifically answered by this manual may be addressed to the Chief Resident(s), the Staff pathologist responsible for that case, or the Directors of the Autopsy Service, as indicated by the particular problem. This manual will be amended or updated as needed. Your suggestions/comments are welcomed. The Autopsy Service performs ~150 postmortem examinations per year (representing ~20% of the deaths at the Hospital). The autopsy at this institution ranges from unrestricted cases in which all the internal organs, including the brain and spinal cord, are examined and removed, to autopsies limited by specific restrictions delineated in the autopsy permission. The majority of our cases are complete adult examinations. A percentage are fetal/neonatal or restricted cases. In addition to their value in epidemiologic studies, detecting or elucidating previously unknown disease processes or complications of therapy, providing a basis for reassurance or genetic counseling of the patient's family, and provision of materials for research purposes, the autopsy represents a critical mechanism for assessing the accuracy of clinical diagnosis and quality of care (reviewed in Cameron et al., Br Med J 281:955, 1980; Goldman et al., N Engl J Med 308:1000, 1983; Landefeld et al., N Engl J Med 318:1249, 1988). Indeed, a large number of wellperformed studies indicate that 1) roughly 25% (at a minimum) of autopsies reveal important diagnoses not detected before the patient's death and which, if detected clinically, probably would have resulted in a change in treatment which might have cured the patient or prolonged his/her survival, and 2) physicians are unable to predict which autopsies are most likely to reveal clinically unsuspected, important new findings. As a result, it is the position of both this Department and the Hospital Administration that every attempt should be made to secure autopsies on every patient dying at the Beth Israel Deaconess Medical Center. Quite clearly, the value of the autopsy is greatest when it is performed properly and the results of the examination are communicated to the patient's physician effectively and promptly. 7 Autopsy Service Coverage Postmortem examinations are performed seven days per week between the hours of 8:00am and 3:00pm. Limited autopsies (brain only) may be started later since. The cases are performed by pathology residents, assisted by a Deiner (Emerson Springer), under the supervision of a staff pathologist. A pathology resident and staff pathologist are on-call at all times to deal with questions and problems that relate to autopsy pathology. On rare occasions, families or physicians will request an autopsy to be done after usual working hours. In virtually all instances, a postmortem examination can wait until the next morning, but exceptional cases are those in which the funeral home may need the body the evening of the patient's death or in which prompt dissection is needed for specialized studies (e.g., viral cultures, electron microscopy). Dr. Hecht or Dr. Connolly must approve delays/after-hour posts. The resident should contact the autopsy supervisor (Gail Howe) to determine if an autopsy assistant is available; however, the resident may be required to perform the autopsy without the autopsy assistant. Preparation for the Autopsy A. Protocol for Autopsies – 1. EAST and WEST CAMPUS (Resident assignments are to one/either or both) a) Admitting should contact the resident regarding autopsies through the AP administrator or directly (weekends), but it would be prudent for the resident to call or walk to the admitting department to see if there are any autopsies pending (754-2212) b) At the Admitting Department: Pick up the Report of Death Form and expiration worksheet Pick up the charts, if available, or check with the floor or with medical records c) Make sure that the Report of Death Form is properly filled out and that the right hierarchy of consent was used in giving the permission for the autopsy. Spouse -> ALL children or designated representative child -> BOTH parents or designated representative parent -> other relative or caretaker with a statement of their relationship to the deceased d) RESTRICTIONS (specified on the permit): Two sections of the permit pertain to restrictions on pathology. 1) “SPECIFIC RESTRICTIONS OR REQUESTS”: These are specific prohibitions regarding dissection (i.e. No head, chest only, etc). 2) “DISPOSITION OF ORGANS FOLLOWING AUTOPSY” (section is reproduced below): These are directions on how the organs are to be treated once they are removed. a) In section one, if the family chooses the second box (“I do not authorize…”), the organs must be returned with the body in a bag within the abdominal cavity. 1. The case will not be presented at Gross conference. 2. The brain should be cut in the fresh state with guidance as needed by a neuropathologist. 3. The organs are reviewed in the fresh state by the attending before they are returned to the body. Histologic sections should be taken liberally (more than the usual 7 cassettes) at the discretions of the attending. 4. You may keep small chunks of organs if their fixation will add value (i.e. a bowel lesion may be kept/fixed with an associated short segment, heart values with vegetations may be detached for fixation and later sectioning), but this privilege should not be abused to accommodate an attending who wishes to view the organs on the next day. The vast majority of each organ must be returned. b) In section one, if the family chooses the first box (“I authorize…”) then a statement of which organs have been kept for fixation must be included in the PAD/FAD. That line is part of the proscribed template (included at the end of this manual). c) In section 3, if the family chooses the second box (“I do not authorize…”) then organs cannot be permanently donated to the medical school for teaching. The resident must notify neuropathology that the brain cannot be donated to Harvard Medical School. 8 This permission covers the removal of internal organs and tissues as may be deemed necessary by the examining physician for analyzing disease processes and determining the cause of death except as specified above by the person authorizing the autopsy. It is understood that due care will be taken to avoid disfiguring the body. The person authorizing the autopsy has the right to control the final disposition of the organs. Beth Israel Deaconess Medical Center will return all organs with the body of the decedent at the time the body is released, except for those organs for which prolonged fixation or complete detailed examination is required in order to complete the autopsy, unless the authorizing person designates an alternative disposition below. The organs retained for detailed examination will be specified in the final autopsy report. The results of the autopsy will be available from the deceased’s physician in approximately 8 weeks. 1) Disposition of organs (choose one): I authorize Beth Israel Deaconess Medical Center to retain any organs for further examination to determine the cause of death or understand the effects of therapy. I do not authorize Beth Israel Deaconess Medical Center to retain any organs. All organs will be returned with the body for burial and a limited report of the findings will be issued to the deceased’s physician. Skip items 2 & 3 below. 2) Disposal of tissue and organs. Tissues and organs taken at autopsy must be disposed of in a lawful way. The person authorizing the autopsy may arrange for disposal or the Medical Center will dispose of the organs. (choose one): The hospital may dispose of retained organs. I will arrange for the retained organs to be retrieved by a funeral home. I understand that organs not retrieved within one week of the signing of this permission will be disposed of by Beth Israel Deaconess Medical Center. 3) Medical research and education (choose one): I authorize Beth Israel Deaconess Medical Center and/or Harvard Medical School to retain organs for purposes of medical research and education. I do not authorize organs being retained for purposes of medical research and education. e) Go to the autopsy log next to the autopsy secretary and obtain an autopsy number. Be sure to fill ALL the information (brain?, date, Resident, attending, etc). f) Review the chart (30-40 min. only), and call the patient’s clinician to discuss the clinical issues and discuss the case with the autopsy staff pathologist. Make sure that the Medical Examiner has been called in cases which fulfill the appropriate criteria to be reported g) During the work week (Monday-Friday), at your request, the autopsy supervisor (Gail Howe) will page the deiner (Emerson Springer) to inform him of the autopsy and will arrange to have him meet the resident at a specific time. h) On weekends, the resident must page the deiner directly (pager #92588) i) As soon as possible after the autopsy is completed, the resident will sign the expiration worksheet and return the original to the Admitting Department so that the body can be released to the funeral home. The resident will call the patient’s clinician to report the preliminary results. j) The patient chart should be returned to Medical records as soon as possible (48 hours max). B. Examination of the Autopsy Permission Form- The Report of Death Form must be accurately and completely filled out before the autopsy can begin. Do not accept a form from Admitting that lacks signature of family/next-of-kin, or the signature of the pronouncing physician. Questions about the validity of the form or its approval can be addressed to the autopsy staff pathologist and, if additional questions remain, to Dr. Hecht. All cases of a medical-legal nature (see Appendix 1&3) should be referred to the Medical Examiner, who may accept or waive the case. Most of the ME cases which are accepted are done by the ME on their premises. If the ME wishes to accept the case to be done at the BIDMC, the case must be discussed with Drs. Connolly or 9 Hecht. It is the responsibility of the pronouncing physician (not the pathology resident) to contact the Medical Examiner; however, if the resident finds, during the chart review, that the case must be reported, he/she may make the call to the ME to discuss the circumstances of the case. Document that conversation on the report of death form in the appropriate section of the Report of Death. C. Medical Chart Review- The patient's chart must be reviewed prior to performing the postmortem examination. This should not take more than 30-40 min (read the summary and transfer notes first). On rare instances, a chart is delayed in transit (outside cases). In order to prevent a significant delay and inconvenience to the family of the deceased, it is acceptable in such cases to obtain an outline of the patient's history either by telephone or in person from the patient's physician, in lieu of reviewing the entire chart (Charts must be returned to Medical Records within two working days after completion of the autopsy- no exceptions.) D. Consultation with Staff Pathologist- It is mandatory to discuss the case with the staff pathologist prior to starting the autopsy. The extent of such discussion will depend on many things, such as the level of experience of the resident, the complexity of the case, etc. Consultation should occur after the examination of the permission from and review of the chart. During the weekend, the resident may contact the staff pathologist anatomic pathologist on-call if there are any questions or problems. Residents may contact the staff anatomic pathologist again if additional questions are raised during the dissection of the case. Specific questions for autopsy are listed by the pronouncing physician on the permit (in the “SPECIFIC QUESTIONS FOR AUTOPSY” section on the last page of the Permit. Otherwise, The resident should speak with the clinical attending physician or surgeon and the patient's house officer prior to beginning. The clinicians sometimes identify areas of clinical concern that are not mentioned in the chart. Note: While we encourage clinicians to attend autopsies on their patients, in no case should a physician or student from another department actually perform the dissection. On rare occasions, and with the permission of our staff, a clinical physician may assist in a dissection, but in no instance should they be allowed to take over the case. When clinicians or students from other departments attend autopsies, they must wear the standard protective equipment and clothing mandatory for all Pathology personnel attending and performing autopsies — no exceptions (see below). A pathology resident, who is feeling pressured by a clinician either to perform a specific dissection other than that initially planned, or to permit the clinician to "assist" in the case, should stop immediately and contact the staff pathologist, Dr Connolly or Dr. Hecht before the situation gets out of hand. Once a patient has been transferred to the Pathology Department, we bear ultimate responsibility for how the autopsy is to be performed 10 Safe Performance of Autopsies and Handling of Tissues and FormalinWhile some patients coming to autopsy will be known to have infectious diseases, ALL PATIENTS' BLOOD AND BODY FLUIDS ARE CONSIDERED POTENTIALLY INFECTIOUS; THEREFORE, GUIDELINES/PROCEDURES ARE STANDARDIZED TO APPLY TO ALL CASES The following regulations are intended to minimize the risks of contracting an infectious disease during the performance of an autopsy and to minimize exposure to formalin. In the event of a formalin spill, please refer to the Department of Pathology, formalin safety manual (SOP) available in all lab areas. The following are minimum regulations. While these minimum regulations have been determined to be adequate for all autopsies (including AIDS cases) by Dr. Kenneth Sands of our Infectious Disease Unit, our Department has decided to use additional measures in certain known infectious cases (see Infectious Autopsy) A. Attire for the Properly Dressed Prosector (Standard Precautions) Any personnel dealing with autopsies in progress or with fresh organs (including residents, staff, fellows, students, pathology assistants/associates and visitors from other departments) must wear gowns, scrubs, plastic aprons, double sets of gloves (metal mesh gloves are provided in addition), masks, goggles, splash shields, and shoe covers. Upon completion of the autopsy and presentation of organs to the staff pathologist, the apron, gloves, masks and shoe covers must be discarded into hazardous waste containers. Scrub suits and gowns are placed in the soiled laundry area. B. Demonstration of Organs at Conferences Fresh organs are not to be shown at Thursday gross conferences. All organs must be formalin-fixed for at least 24 hours, and then washed before the conference. In order to minimize formalin exposure at Autopsy Conferences, all organs must be washed thoroughly. See “handling of tissues and formalin” for washing instructions. C. Preparation of Blocks for Microscopic Slides Fixed specimens from autopsies are to be cut into blocks only in the autopsy room. Appropriate attire includes gloves, gown, mask, eye protection (chemical safety-type glasses or goggles or splash shields), and apron at a minimum D. Storage of Fixed Tissues All fixed or fixing tissue should be kept in heavy-duty plastic containers with lids. These containers can be stored in vented cabinets. Uncovered fixed tissue of any kind should not be stored in morgue coolers or left out on counters. No tissue containers should be stored out on the floor at any time E. Discarding Fixed Specimens It is the responsibility of staff pathologists and residents to discard tissues promptly; only specimens from ME or potential medical-legal cases will be saved indefinitely; specimens from other cases will be discarded quarterly after gross diagnosis is completed, unless the staff pathologist specifically asks that the save period be extended F. Autopsy Worksheets are NEVER to Leave the Autopsy Room All autopsy worksheets are to be transcribed onto clean paper before leaving the autopsy room; the original worksheets (whether obviously blood-stained or apparently "clean") are not to leave the autopsy room under any circumstances G. Autopsy Procedure 1. The tags on door and on the body are checked for the patient's name to see if they match the autopsy request. The body is then taken from the cooler; all outside sheets are removed and sent to the Laundry in designated laundry collection bags. THE RESIDENT WILL DOUBLE-CHECK THE BODY TAG TO CONFIRM IDENTIFICATION 2. The body is put onto the autopsy table. At this time, the plastic morgue sheet is removed and put into a disposable garbage bag; all bandages are removed at this time and are also put into the same garbage bag 3. A 2% bleach solution is used to wash off visible blood on body surfaces 11 4. During autopsy, interns, residents and pathology assistants wear personal protective equipment: goggles or splash shields, gloves, masks, and aprons. Complete change of clothing (scrub suit) and morgue shoes are also worn 5. After evisceration, the body is washed with an EPA-approved detergent disinfectant (Phenex solution and bleach), then completely stitched up after a proper amount of cellulose batting is placed in the brain, thorax and abdominal cavity 6. The body is then removed from the autopsy table and wrapped in a new morgue sheet; the proper tags are placed back onto the body, which is then put back into the cooler 7. Area is washed down with bleach and an EPA-approved detergent disinfectant (Phenex). Instruments are immersed in the same for 30 minutes. The autopsy assistant will clean his instruments and will clean and disinfect the autopsy table. He/she will also close and tape-up the biohazard boxes. The resident is responsible for (i) cleaning the cutting board; (ii) washing all his/her instruments, (iii) cleaning the sinks and counter areas; (iv) replacing dirty chux, (v) disposing of all blades, including the long blade, from the knife handle; (vi) cleaning all spills on the floor H. Washing of organs before conference1. Formalin is discarded into the waste containers, and the organs are rinsed for 10 minutes in a large bucket of water. 2. Two such buckets will be prepared and used/shared for ALL the cases before each conference. This “first rinse” water (2 buckets/conference) will be discarded as formalin waste after all cases have been rinsed. 3. After the initial “bucket rinse”, the organs will be rinsed in running water from the tap. 4. There is NOT a specific formalin sink, but drain formalin levels should be kept to a minimum by NEVER dumping formalin directly into the sink and pre-rinsing the organs in the bucket. Infection Control Guidelines THE PURPOSE OF THESE GUIDELINES IS TO DETAIL SPECIFIC INFECTION CONTROL PRACTICES FOR AUTOPSY STAFF TO REDUCE THE RISK OF OCCUPATIONAL EXPOSURE TO BLOODBORNE PATHOGENS, TB AND OTHER INFECTIOUS DISEASES THROUGH A PROGRAM OF INFECTION CONTROL QUALITY ASSESSMENT AND IMPROVEMENT STANDARDS ARE BASED ON CURRENT KNOWLEDGE AND INCORPORATE THE CENTERS FOR DISEASE CONTROL (CDC) "RECOMMENDATIONS FOR PREVENTION OF HIV TRANSMISSION IN HEALTHCARE SETTINGS" AND THE NATIONAL COMMITTEE FOR CLINICAL LABORATORY STANDARDS "PROTECTION OF LABORATORY WORKERS FROM INFECTIOUS DISEASE TRANSMITTED BY BLOOD AND TISSUE" AND OCCUPATIONAL HEALTH AND SAFETY ADMINISTRATION STANDARD "OCCUPATIONAL EXPOSURE TO BLOODBORNE PATHOGENS." Remember that all patient specimens are considered potentially infectiouS, and handwashing is the single most important factor in the prevention of disease transmission A. General: 1. All patients' blood, body fluid, and tissues are considered infectious and must be handled according to the principles of Standard precautions. Therefore, all autopsy procedures should be performed under the guidelines of Standard Precautions. 2. Work practice controls: There will be no hand-to-eye/-nose/-mouth action (i.e., eating, drinking, applying lipbalm or cosmetics, adjusting retainers or contact lenses) in any autopsy area 3. Thorough handwashing with soap is an important method of preventing infection. A sink should be designated for handwashing. Soap (not bar soap) and paper towels dispensers must be at this sink 4. Handwashing must be done: 12 a) Immediately if hands are soiled with blood, body fluids, or tissues b) Immediately after removing gloves c) Before leaving the autopsy area, and at the end of each day B. Personal Protective Equipment: Personal protective equipment, gloves, clothing, facewear, should be located in a designated area readily accessible to all staff. 1. Skin integrity — Autopsy staff with hand cuts, abrasions, areas of dermatitis, etc., should report to employee/occupational health services for evaluation of the appropriateness to work and to determine the need for other protective measures (e.g., cotton gloves, skin cream barriers). All skin defects should be covered with a water-impermeable occlusive bandage 2. All autopsies shall be performed while wearing cap, mask, gown, scrub suit, morgue shoes, goggles or splash shields and gloves (see Procedure: Autopsy) 3. Contaminated personal protective equipment should be discarded in the appropriate biohazard receptacle C. Specimen Handling: 1. Care will be taken to avoid glove tears, puncture wounds and cuts by sharp bone edges, scalpel and needles from all autopsy cases. 2. Splashing of any body wash fluids shall be avoided 3. Fresh tissues should be immediately placed in a suitable fixative 4. All specimens are either received in or placed in formaldehyde or other fixative 5. All tissue specimens are disposed of in the appropriate biohazard incinerator receptacle (see procedure: Disposal of surgical tissue/biological waste) 6. Specimen storage refrigerators/cold rooms must be clearly labeled for that purpose and must not contain any food items D. Equipment: 1. Contaminated disposables are discarded either into infectious waste receptacles or are disposed of along with tissue in special incinerator boxes. 2. Reusable equipment (i.e., specimen-testing equipment) must be disinfected by a 1:10 dilution of bleach prepared daily, or by a phenolic-Phenex 3. Equipment that has been contaminated with blood or other fluids should be disinfected before being repaired in the department or transported to maintenance or the manufacturer E. Needles, Syringes and Other Sharps: Needles must not be recapped, purposely bent or broken by hand; rather, after use, needles, syringes, and other sharps should be placed directly into puncture-resistant receptacles specified for this purpose for disposal F. Environmental: 1. Detergents/disinfectants- A detergent solution should be available for cleaning and a disinfectant, such as a 1:10 dilution of bleach, should be prepared daily (or a phenolic-Phenex). 2. Accidental spillage of specimens should be cleaned up with a 1:10 dilution of bleach prepared daily (or a phenolic-Phenex). The appropriate protective equipment should be utilized for the clean-up (e.g., utility gloves, especially in the case of broken glass) 3. The autopsy table, all instruments, sinks, floors and any other involved surfaces shall be thoroughly cleaned immediately following each autopsy with an EPA-approved detergent disinfectant and a 1:10 dilution of bleach or a phenolic-Phenex 4. Environmental Services will perform a through cleaning of the autopsy spaces weekly G. Employee Occupational Health and Safety: 1. Autopsy staff should take care to minimize the formation of droplets, spatters, splashes and spills of blood 13 and body fluids through work practice controls 2. Autopsy staff should take precautions to prevent accidental injuries caused by needles, scalpels, and other sharp instruments or devices during procedures when cleaning used instruments, during disposal of used needles, and when handling sharp instruments after procedures. 3. Autopsy staff should report IMMEDIATELY all blood and body fluid exposures defined as percutaneous inoculation of blood and body fluids via a needle puncture, open cuts on hands, or splashing into the eyes, nose or mouth. All exposures should be reported to the supervisor and the employee should report to employee/occupational health services (Emergency/Walk-In Units off shift) for appropriate follow-up. 4. Exposed area should be washed immediately, if a needle or sharps puncture occurs; bleeding should be forced. 5. The hepatitis B vaccine is available free of charge through Employee/Occupational Health Services. It is recommended that all personnel working with human blood, body fluids and tissues be vaccinated. 6. Semi-annual TB skin testing is performed in Employee/Occupational Health Services. It is important for all employees 7. Autopsy supervisors will monitor adherence to the use of personal protective equipment, and work practice controls in the autopsy area. When monitoring reveals a failure to use personal protective equipment and work practice controls, counseling, education and/or retraining will be provided H. Training and Education: (Infection Control, HIV, HBV, and TB): New staff receive an infection control lecture as part of hospital orientation. Initial education regarding the risk of occupational exposure to bloodborne pathogens takes place during the Pathology Department Orientation Program. There is an annual review of the risks of bloodborne exposure and other infectious diseases. Other infection control information is disseminated through infection control bulletins, updates, and reports I. Quality Assessment and Improvement: Collaboration with the management and staff of the unit for the purpose of quality assessment and improvement for patient care and employee health and safety is on-going. AUTOPSY ROOM: General Overview and Division of Labor A. At the end of the autopsy, the resident is responsible for spot cleaning: 1. cleaning the cutting board w/disinfectant; 2. washing all instruments w/disinfectant; 3. cleaning the sinks and counter tops w/disinfectant; 4. disposing dirty chux; 5. disposing of all blades, including the long blade, from the knife handle; 6. cleaning all spills on the floor C. The autopsy assistant will get the body out of the cooler and into the morgue. If the patient is obese, the autopsy assistant will ask the resident to help move the body onto and off of the table. Security needs to be called to open the cooler door when the pathology assistant is not available D. The resident is responsible for doing the gross examination E. The resident is responsible for any cultures or sampling that needs to be done and should tell the autopsy assistant beforehand that these samples will be obtained prior to the evisceration F. The autopsy assistant will do the evisceration and bring the organs over to the sink for the resident, but the resident is expected to be present at the table during the evisceration and to perform at least two (2) eviscerations during the first year G. The autopsy assistant will fix the brain and spinal cord in a brain bucket for the resident. The resident should make sure that the weight is taken before placing the brain into fixative and double-check that the brain is correctly labeled with the autopsy number. The resident will perform two (2) brain removals during the first year H. The autopsy assistant will close and clean the body w/ disinfectant. He may ask the resident for help with 14 moving the body from the table back onto the cart I. The autopsy assistant will clean his instruments and will clean and disinfect the autopsy table. He will also close and tape-up the biohazard boxes J. After the resident has completed the autopsy and cleaned up his/her area, the resident needs to complete the expiration worksheet of the Report of Death Form and return all paperwork (Report of Death Form and completed expiration worksheet) to Admitting. Autopsies on Patients Who Die Outside Beth Israel Deaconess Medical Center A. There are four categories of potential autopsy cases from patients dying outside the hospital: 1. BIDMC patients dying elsewhere 2. Non-BIDMC patients dying at an institution which has a contract to have autopsies performed at BIDMC 3. ME cases transferred to BIDMC for autopsy 4. Non-BIDMC patients for whom the managing physician or family members want to have an autopsy done at BIDMC B. Charges: 1. If the patient has ever been a Beth Israel Deaconess Medical Center or Joslin Clinic patient, there is no hospital charge to the family for performing the autopsy at Beth Israel Deaconess Medical Center. Outside institutions which have contracts with BIDMC (Hebrew Rehabilitation Institute, New England Sinai, Emerson Hospital, BI Glover/Needham) are generally known to Admitting. 2. ME cases are accepted at the discretion of the BIDMC Medical Examiner, Dr. James Connolly or Dr. Jonathan Hecht. In any questionable or uncertain cases of this nature, please contact Dr. Hecht or Dr. Connolly. Additionally, in any case in which there is any concern regarding possible medical malpractice or allegations, neglect or criminal circumstances, the case must be discussed with Dr. Hecht or Dr. Connolly before proceeding with the autopsy. 3. If the patient has never been seen at BIDMC or in a BIDMC-affiliated practice, the case must be accepted by either, Dr. Jonathan Hecht (Director of Anatomic Pathology,) or Dr. James Connolly before the autopsy can be done at BIDMC. There is a charge for performing such a case at Beth Israel Deaconess Medical Center, and the referring physician, institution, or family must be informed of and agree to be responsible for the charges before we accept the transfer or the patient, and before we begin the autopsy. Dr. Hecht, or Dr. Connolly will discuss these charges with the referring physician or family member. The cost for a complete autopsy with neuropathological exam is $2,500; for a brain-only case, the charge is $700.00; for a limited case, the charge is ~$1,000, depending on the extent permitted. C. Report of Death-The referring clinician is responsible for completing the entire Report of Death form. The BIDMC Admitting Office can fax a copy of the Report of Death form to this physician if there is none available at the outside institution or practice. The referring physician is responsible for contacting the Medical Examiner's Office at 617-267-6767 in any case fulfilling the criteria as outlined on the BIDMC Report of Death form. D. Notification of the Pathologist- The funeral home must notify Admitting upon the arrival of the body at Beth Israel Deaconess Medical Center. The body must arrive properly identified, preferably with a toe tag or wrist/ankle identification band, in order for the autopsy to proceed. Admitting should notify the pathologist of the arrival of the body. The Admitting Coordinator must enter the name of the patient into the Death Log (outside the morgue) with the other pertinent information E. Expiration Worksheet and Death Certificate- The expiration worksheet is filled out by the pathologist after the autopsy has been completed and the cause of death determined. The Death Certificate will be typed in Admitting, and the BIDMC clinician will sign the Death Certificate. It is the responsibility of the funeral home to obtain the referring physician's signature when the patient comes from outside the Beth Israel Deaconess Medical Center 15 Medical Examiner's Cases (Cases reportable to the ME are listed in Appendix 3) A. Permit- All patients autopsied at Beth Israel Deaconess Medical Center must have a properly filled-out death report form signed and received from Admitting. In the event that the case is Medical Examiner's case, the physician caring for the patient must notify the Medical Examiner's Office (at 617-267-6767) to report the case. If the Medical Examiner accepts the case, the autopsy may be performed either at the 720 Albany Street facility or here at Beth Israel Deaconess Medical Center under the direction of the Medical Examiners or BIDMC staff. If the Medical Examiner has accepted the case, no permit is necessary from the family, and in fact, the legal requirements of the Commonwealth override the family's wishes in these cases, although where strong objections exist, they may be considered and weighed in performing the case B. Logbook- The name of the patient should be entered chronologically in the main Autopsy Log Books, where the case receives a BIDMC autopsy number. All ME cases will be performed at the East Campus morgue. In the space where clinical diagnoses are usually entered, there should be recorded "Medical Examiner's Case" with the CME number corresponding to the Medical Examiner's Office autopsy number for the case. No data regarding autopsy findings should be reported in our logbook. Any information released regarding the autopsy must be at the discretion of the supervising ME, as some cases may have legally sensitive issues that should not be released from the Medical Examiner's Office C. Autopsy Notes and Paperwork- Notes, measurements, weights and all records of observations should be recorded on forms provided by the ME office and available in the morgue. All provisional or final diagnosis information should be collated by the supervising Deputy Medical Examiner, who will forward these data to the ME office for transcription and final reporting. None of these data are given to our secretary at the BIDMC. There should be only one folder per case with all the relevant forms, section key and clinical data, and this folder should be locked in the office of the Attending ME. Once the final report has been generated and signed at the ME Office, all other notes and records must be destroyed, as they can be subpoenaed and may, on occasion, become the source of troublesome errors or conflicts, as, for instance, where an impression from the gross is recorded without subsequent modification after reviewing the microscopy D. Performing the Autopsy and Special Procedures for ME cases 1. External Examination- As in all autopsies, careful examination of the body should include records of height and weight, all scars, marks and evidence of treatment, violence or trauma. Records should be in centimeters (cm). Careful and extensive gross photos are particularly important to record evidence of trauma, burns or medical treatment, in order to resolve issues of size and extent, and to provide a visual record useful for court testimony. All jewelry should be removed, identified and put in the hospital safe, with the ME notified. 2. Internal Examination- It is essential to examine internal organs prior to evisceration to establish possible evidence of trauma or violence while the organs are in their natural anatomic position. This permits correlation of contusion sites on the skin with areas of hemorrhage or other injury involving internal organs or correlation of the track of a wound with organs underlying the wound. If radiologic studies have not been performed prior to death, a complete set of full-body x-rays should be considered to look for fractures, bullet or knife fragments. Careful examination of the pulmonary and coronary arteries in situ may permit observation of air emboli. 3. Bloodwork and Special Studies- Prior to evisceration, samples should be obtained for toxicology or other laboratory studies where necessary. The forms must be completely filled out, carefully specifying the type of sample and the source and type of blood drawn (location on body, i.e., femoral, heart, subdural, etc., affixing appropriately labeled stickers onto the specimen jars. Such samples must be handled using strict Chain of Custody principles and, thus, must be kept in the presence of or on the person of the pathologist or pathology assistant until they are picked up by a detective to be taken to the Massachusetts Police Laboratory. In the morgue, there are special vials and forms for the ME cases; these vials are NOT to be sent to our clinical laboratory. (In non-ME cases where drug levels are to be ascertained, call the Clinical Laboratory to determine the appropriate type of sample and container.) Notify the ME office at the time the samples are taken to expedite the notification of a detective to pick up the samples. 4. All Medical Examiner's cases dying within 48 hours of admission to a hospital should be considered as possible candidates for toxicology screening. In cases of motor vehicle accidents, blood and urine samples 16 for ethanol and other recreational drugs should be taken. In certain instances, gastric contents and/or bile samples should also be taken; these decisions are made on a case-by-case basis after discussion with the attending ME. In patients with coma of uncertain origin, vitreous humor should also be taken for glucose and ketone levels. In the case of patients who were on therapeutic drugs, drug levels may be considered in selected instances, such as to check the phenobarbitol level in a seizure patient involved in a motor vehicle accident 5. Microbiologic cultures should be obtained in all fetal autopsies, but only in those rare adult cases where infection is a major consideration as the cause of death and in which pre-mortem cultures were not obtained. The decision to culture is made with the attending pathologist. 6. Autopsy Dissection and Evisceration- The autopsy may be performed in the standard Rokitansky fashion or by using the modified Virchow approach. The latter is the method commonly used in ME cases in which the organs are not eviscerated en bloc; instead, they are removed organ by organ. The latter method is less familiar to most residents in the program and should only be used if the resident is able to dissect carefully, without damaging the carotid and femoral arteries, and only if he/she is able to maintain the dissection in context — i.e., looking carefully for trauma or disease involving contiguous structures and organs 7. All organs must be weighed, with standard measurements (e.g., ventricular thickness, heart valve circumferences) obtained. After breadloafing the organs, organs should be placed in a plastic bag to be returned to the body cavity and sent with the body to the funeral home. A representative slice or section of each organ shall be retained in your stock bottle for histology or examination post-fixation i) In any case where a cardiac abnormality is considered, the entire heart is retained for perfusion fixation ii) In any case where neurologic disease is considered, the entire brain is fixed for later sectioning. Brains in ME cases only are otherwise cut in the fresh state. In all ME cases, the dura should be removed from the bones of the cranial vault to look for subtle skull fractures. In all cases, the pituitary should be identified iii) If organs cannot be presented to the staff pathologist in a timely manner (ie. Infectious cases), entire organs may be maintained and discarded later as medical waste or transferred (on request) to the funeral home for burial. The decision and responsibility of choosing to retain organs will be that of the staff pathologist 8. Submission of Blocks — The number of blocks taken in ME cases should be limited to those organ systems immediately relevant to the cause of the patient's death. In rare exceptions, other organs may be sampled, after discussion with the attending ME. Other tissues may be retained in your stock pot. All blocks should be labeled with the CME autopsy number, with the section key given to the attending ME. Each slide reviewed must be signed in permanent ink by the reviewing ME. After completion of the microscopic review, all slides and paraffin blocks, along with the tissue stock bottles, are transferred to the ME Central Office on Albany Street for permanent storage. 9. Dictation — The clinical, gross, and microscopic summaries are dictated utilizing a standard format available from the ME staff pathologist. Tapes are mailed or hand-carried to the ME Office, where all transcriptions are done. The final report is signed at the Albany Street Office and stored there. No copies of the report may be released to us. Residents should make a note for their own records of the age and sex of the patient, and the major diagnoses to serve as information for applying for Board Examination, as they will not have a copy of the final report E. Death Certificate-In all ME cases, it is the Medical Examiner who composes and signs the Death Certificate. In ME cases done at BIDMC, the medical examiner or Drs. Hecht or Connolly fill out and sign the Death Certificate. The certificate must be signed in black ink. The address for Drs. Hecht or Connolly, when acting in the capacity as Deputy Medical Examiner, must be the 720 Albany Street office. Thus, we do not merely check and agree with the clinical causes of death. We must determine the manner of death: Natural, Accidental, Homicide, Suicide or Undetermined. If the patient has died of pneumonia after a fractured hip from a fall downstairs, the cause of death is NOT natural; it is Accidental, as none of the complications would have ensued if not for the accident. The certificate might read "acute pneumonia complicating a femoral fracture," the manner of death being Accidental. A man who dies of a myocardial infarct after being startled by a burglar in his home is a homicide victim. Writing up the Death Certificate is an art and science perfected by experience, but the guidelines are: (i) keep it simple and (ii) think carefully about the events leading up to the death. 17 (End of Medical examiner section) Ancillary Studies A. EXCEPT AS NOTED, ALL ANCILLARY TESTS MUST INCLUDE A REQUISITION STATING THE TEST NEEDED AND, "AUTOPSY - NO CHARGE." SUCH STUDIES ARE NOT TO BE BILLED TO THE PATIENT'S FAMILY B. Heart Blood Protocol: a) Heart blood should be taken in selected cases where serum might not be available in the clinical laboratory (ie. Non-inpatients), and can be used for biochemical testing/drug screen. In certain instances serological studies may be valuable in helping to establish an infectious diagnosis. These cases should be tailored according to discussion with the microbiology lab director on-call. b) Collect two (2) red-top (empty) tubes of blood from a vessel or heart (scooping spilled blood from a body cavity is unacceptable) spin it for 15 minutes in the clinical lab (call the CP resident on-call if you get lost), pour the supernatant into a second tube, then place the tube in the cutting room freezer. After the spindown/pour off, the tube must properly labeled with the date and the autopsy number. c) The tubes will be kept until the Autopsy Conference. After the conference, the resident is responsible for throwing out the tubes from the freezer for their cases. If there is a West Campus autopsy, the resident is responsible for bringing over the tube of heart blood and spinning it down, labeling it, and placing it in the cutting room freezer. C. Postmortem Microbiological Studies: Postmortem microbiological examination (including gram stain) may be useful in selected situations, but it should not be utilized in all autopsy cases. Blood cultures in general are highly sensitive and specific in living patients, but have limited utility as a routine procedure in postmortem evaluations. If a blood culture has been obtained prior to death there is usually no need to re-culture the patient, unless you are looking for unusual organisms (e.g., Brucella). In this case, contact the CP resident on-call for instructions. Tissues (lung/spleen) for culture are the more typical specimen. One should consider performing postmortem cultures in the following clinical situations. It is also a good idea to consult the staff pathologist, a microbiology staff member, or the CP resident-on-call. Remember to fill out a requisition in Microbiology (specify that this is an autopsy specimen under under MRN#01238374, Do Not bill; fetal cases should be entered into the mother's record). 1. Continuing clinical evidence of pneumonia and/or cavitary lesions. If an open lung biopsy has been done and appropriate cultures have been obtained prior to death, call the laboratory director, because lung culture and/or blood culture with special techniques for unusual organisms maybe indicated. The appropriate approach requires the consultation of a microbiology specialist. 2. Immunocompromised patients, unless there has been a recent respiratory culture. One would consider reculture of lung in patients in whom a new pneumonia or a new clinical infection has developed without an intervening opportunity for appropriate pre-mortem culture (such as bronchioalveolar lavage or open lung biopsy and culture). Blood cultures should be considered if no recent pre-mortem blood culture has been done. 3. Patients in whom there is a clinical concern of sepsis, in whom there have been no pre-mortem blood cultures, or in the instance of an unusual organism which would not usually be detected by blood culture. Blood culture and lung culture should be considered. 4. Neonatal deaths or stillbirths (ALL CASES), especially in those where there is a history of: a) Possible chorioamnionitis (culture the placenta: peel up the chorionic surface membranes and take a sterile chunk of tissue) b) Premature delivery (culture the placenta as well as the fetus) 18 c) Known infection of the mother, without opportunity for appropriate pre-mortem cultures. (1) In these instances it is necessary to review the microbiologic data available on the computer and to discuss the case with the laboratory director, as special tests for Chlamydia trachomatis, and/or Mycoplasma hominis may be indicated in infants who have evidence of pneumonia. (2) Take lung and spleen for culture. Specify Ureaplasma, mycoplasma and group B strep. Remember: In the neonatal intensive care unit many ill and tiny babies are housed in close proximity to each other. Therefore, documentation of infections in deceased neonates has important epidemiologic implications for managing other babies. 5. Cases where the initial gross examination discloses an unsuspected and uncultured abscess cavity, endocarditis, tuberculosis, or fungal lesion. The lesion should be cultured directly. 6. Dialysis patients who present with septicemia - specifically, examine and culture the A/V fistula if it had not been done ante-mortem 7. Patients in whom autopsy discloses any unexplained or unusual findings in any tissues or organs, for which the differential diagnosis includes infection and in whom appropriate pre-mortem cultures were not available. In the event of such a finding (ie. Cardiac valve vegetation), the dissection should be halted, the appropriate autopsy staff member should be contacted, and the issue should be discussed with the autopsy staff person and/or the director on-call of the microbiology laboratory. 8. Specimen collection for microbiologya) For procedural questions please refer to the clinical laboratory test menu. For questions call microbiology 7-2306. specimens should arrive in the laboratory within 2 hours after collection in appropriate closed containers b) Order of sampling and collection: Samples of the lung and/or blood should be obtained prior to manipulating the bowel, to minimize the risk of contamination by enteric organisms. Generally speaking, bacterial invasion and overgrowth become considerations only if a culture is taken about eighteen hours or more after death. For this reason the interval between the time of death and autopsy should be recorded c) Labeling: Successful microbiological isolation depends on appropriate labeling of the specimen. Please include the suspected diagnosis, the patient's name, and specific suspected diagnosis. The patient's name is particularly useful as the technologist may already be familiar with ante-mortem isolates from the same case. The autopsy number alone will not provide this essential information to the laboratory. Please fill out appropriate requisitions for all samples submitted. Correct labeling is the responsibility of the pathologist. Specimens must be submitted as soon as possible to avoid deterioration and/or overgrowth, and it is worth interrupting the remainder of the dissection in order to get specimens to the laboratory promptly d) Blood cultures: Blood specimens for culture can be obtained from the heart (right atrium, pulmonary artery trunk, or inferior vena cava) and/or the splenic pulp (much less satisfactory). There are two ways of taking blood from the heart. One requires a V-shaped opening of the pericardium without touching the heart itself and then aspiration of blood from the atrium or pulmonary trunk. If this cannot be done (adhesions or excessive effusion) or if contamination of epicardium occurs, the selected area of epicardium should be seared to dryness with a hot spatula, and then the needle inserted through the seared area. As blood cultures will be obtained only in unusual instances after discussion with the laboratory director, the appropriate medium and/or broth for culturing should be tailored to the individual autopsy. The lab slip should indicate the clinical suspicions, including appropriate information of possible such as: (1) Suspected fungemia (2) History of antibiotics and specific antibiotics utilized (3) History of possible salmonella e) Lung and other viscera: The heat sterilization method must be used for obtaining specimens from all other organs. When fluid, for example, lung exudate, is needed, a sterile scalpel blade can be used to 19 make an incision through the seared surface of the lung, and swab collections made for aerobic and anaerobic culture. Fragments of tissue for viral, fungal, and mycobacterial cultures can be obtained at the same time. Specimens for anaerobic culture must be collected as quickly as possible and promptly transferred to an oxygen-free transport tube (see below for transport collection systems) f) It is essential to label the specimen as to the source of tissue and the suspected organisms, so that the appropriate inoculation procedure can be selected in the microbiology laboratory. Tissue sampled should be at least 3 mm cubes, preferably at least two tissue pieces, as multiple small pieces are more likely to yield positive growth than a single large fragment. g) Imprints and smears of selected organs: During any autopsy, it is always possible to make fresh imprints or smears of suspected infectious cases for routine gram, PAS, and Methenamine silver stains. In addition, scrape smears or touch preps should be obtained from cavitary lesions which have a differential diagnosis of tumor versus infection, and if a necrotizing tumor is discovered on the cytologic evaluation, the expensive and detailed microbiological workup of tissue samples can be halted. Always take imprints and smears after cultures have been taken to minimize the possibility of contamination. Also do not overlook the value of Papanicolaou stains of imprints and smears in a diagnosis of viral diseases 9. Specimen Collection and Transport Systems a) Anaerobic Transport Swabs or Syringes (capped w/needle removed) - They are available throughout the hospital and should be used for transport of aspirated fluids such as pleural, peritoneal, and joint fluids. as well as abscesses. Tissues should be placed in a sterile cup and transported to the lab as soon as possible after collection b) Stool transport systems- Stool for enteric culture and O & P may be transported in CLEAN, TIGHTLY CAPPED CONTAINERS which aren't sterile c) Swabs- The use of swabs to collect material for Microbiological testing is adequate for skin, mucous membranes, genital sites and anal crypts only (1) Most testing for Chlamydia, mycoplasma, and viruses require DNA and can be sampled by standard sterile aerobic swabs (available on the floors and in the autopsy suites). (2) To ensure adequate amounts of material for inoculation, ONE swab should be submitted FOR EACH TYPE of culture requested. d) Urine transport - For clean catch urines a CVS kit with a gray-top tube and collection cup should be used. If a UA and other tests are needed at the same time, send a solid red-top tube wthout a serum separator filled with urine ANCILLARY STUDIES, OTHER TRANSPORT DEVICES Hematopathological Studies: In cases of lymphoma/leukemia or other hematopathological processes, it is important to sample the following organs: liver, spleen, lymph nodes, thymus (if it can be identified), and bone marrow from multiple sites (at a minimum, sample ribs and vertebrae) 1. In cases of marrow failure or pancytopenia, a wedge of femoral marrow should be obtained. 2. Most tissues may be formalin fixed (do this early in the autopsy dissection). In cases of a lymphoma either first discovered at autopsy or not phenotyped prior to death, tumor tissue might be frozen in “oct” gel for later marker and molecular studies (in consultation with Hematopathology Staff and/or fellows) 3. Touch imprints of suspicious lymph nodes or vsiceral tumor nodules are also useful. For Giemsa stains, these can be air-dried. For Diff-Quik® stains, they should be air dried B. Quantitative Studies of Aluminum, Copper, Iron, Asbestos, etc.: Occasionally it may be necessary to do quantitative chemical studies of tissue specimens to investigate a specific disease process. For example, a quantitative iron determination on liver may be helpful in differentiating primary iron overload from other iron storage diseases. The Director or the GI team should be consulted before a quantitative chemical study is ordered. Such postmortem analyses are not generally reimbursable, and therefore will not be sent except in the case of unusual circumstances or if the family agrees to pay for such studies. Asbestos fiber determination can be of great value, especially in workman's compensation cases likely to come to trial. Save extra lung tissue (in 20 stock bottle) in cases of possible occupational lung disease. Lawyers will generally request such tissue and arrange for studies on their own. Bone for metabolic work-up can be fixed in buffered formalin or 70% ethyl alcohol C. Cytogenetics: Prior to beginning a fetal or neonatal autopsy, it is important to decide whether or not Cytogenetics studies should be performed. In deciding whether or not to submit Cytogenetics tissues, one should also consult the autopsy staff pathologist or the clinical attending to determine if such studies are indicated. A long post mortem interval (greater than 10-15 hours) may diminish the value of these studies, and the post mortem interval, if known, should be written on the requisition accompanying tissue to the Cytogenetics laboratory. In addition, if previous antemortem amniocentesis and chromosome studies have already been performed, it is not necessary to submit additional tissue at the time of autopsy unless requested by the clinician (as in the need for more detailed banding or enzyme studies). 1. The following are the clinical indications for which to consider the study: a) Unexplained fetal death associated with congenital anomalies b) A history of three or more spontaneous abortions or fetal losses c) Severe intrauterine growth retardation unexplained by other circumstances d) Ambiguous genitalia after thirteen weeks of gestation e) Any major malformations, for example cleft lip with fetal death, club foot with fetal death. (The two conditions which would not fall into this category would be neural tube defect or renal agenesis/dysgenesis f) Familial history of genetic diseases or syndromes g) History of previous chromosomal abnormality or genetic abnormalities associated with previous births 2. Tissues should be submitted as rapidly as possible after completion of the autopsy to the Cytogenetics laboratory at Beth Israel Deaconess Medical Center. Transport medium or saline is available in the Surgical Pathology cutting room refrigerator, from the Cytogenetics section during normal working hours or from Laboratory Control in shifts other than weekday "day" shifts. If you take the last container of transport medium, please obtain additional medium at the laboratory at the time of submission of specimens. Appropriate specimens to submit include a piece of skin, a piece of deep fascia (as above the groin), fetal placenta and membranes, and pieces of fetal viscera, such as lung and spleen. The more tissues submitted, the greater the opportunity to obtain reasonable cell growth. Fetal placenta and/or membranes may grow better than others given a long post mortem interval. Please put the different specimens in different containers, as this also increases the likelihood of obtaining a sterile sample. Specimens should be obtained by sterile technique, swabbing the skin with iodine and cutting with a sterile blade. D. Electron Microscopy: Due to autolysis, autopsy material generally is not adequate for electron microscopic examination. On occasion (e.g., tumor of unknown primary), autopsy tissue taken shortly after death may be studied. The decision about whether to process such tissues will be made, on a case-by-case basis, in consultation with Dr I Stillman and the EM Department. In potential cases, small (1 mm) tissue fragments (avoid obviously necrotic areas) should be fixed in K2 for 2 hours, at room temperature, and then transferred to cacodylate buffer for storage at 4°C. The tissue will be held in the EM lab, and the decision as to whether the case will be processed will be taken after evaluation of the light microscopy. Isaac Stillman should be paged prior to beginning cases of intrinsic medical renal disease and renal allograft. In such cases, a portion of renal tissue / allograft should be frozen (in cryostat) for potential IF studies. F. Toxicological and Ocular Fluid Studies: Occasionally it may be necessary to obtain tissue and body fluids for toxicological or electrolyte analysis (e.g., ME cases). In a suspected case of drug overdose or toxicity, obtain (at a minimum) liver (300 grams), bile (10 ml), blood (50 ml in sodium fluoride) and urine (50 ml); keep all of these specimens at 4°C. Gastric or small bowel contents may be useful in evaluating potential oral drug overdose. Ocular fluid analysis may be useful in evaluating electrolyte and certain drug levels prior to death. (In some instances, levels of electrolytes and drugs in the ocular fluid are more stable in the postmortem period 21 than are blood levels.) Instruction on the proper procedure for obtaining ocular fluid will be provided. Any questions regarding these tests and which test is most appropriate should be directed to Dr. Bruce Beckwith or Dr. Gary Horowitz Organ Donation A. Eyes- Residents will be notified by the Admitting Office that eyes will be removed by the Organ Bank on certain cases scheduled for autopsy. Eye Bank technicians will remove the eyes either in the evening or morning before the autopsy is performed. In the event of an afternoon autopsy, the Eye Bank should be called (5733325) to arrange a mutually convenient time for removal of eyes. Eyes can be removed in the cooler; the procedure does not require the presence or assistance of either Pathology Assistants or residents. B. Skin and Bone- These will be taken at 8:30 a.m. on weekdays before the autopsy begins. Removal is done by Organ Bank technicians. Pathology residents may be called in the evening to be informed that skin and bone will be harvested on a case to be autopsied in the morning. In the case of skin and bone harvesting on a weekend (on a body not being autopsied), only the Pathology Assistant will need to be present. During a weekday, the harvesting of skin and bone from non-autopsied patients will be done at a mutually convenient time for both the Organ Bank and Pathology Associates and Assistants. The Complete Adult Autopsy (see also Appendix 4) A. Confirm patient identity by checking the "toe tag" or body label. In cases where such identification is missing, the staff physician, funeral director or nurse must identify the patient before the case can be started. B. General: The complete autopsy includes (but need not be restricted to) a careful external examination, examination and removal of all internal organs (neck, thoracic, abdominal, pelvic organs, and brain), and examination and sampling of ribs, vertebral column, skin and muscle. The spinal cord should be removed in all cases. Testes should be removed in all unrestricted adult male autopsies and should be removed if there is any clinical suspicion of a testicular problem, or in cases of cancer of unknown primary. In addition to the routine dissection in unrestricted autopsies, one can examine and sample most anatomical regions, providing that the dissection of that region will not deform or disfigure the body. A resident should never undertake a difficult dissection in the region of the head and face or distal extremities without first discussing the issue with the staff pathologist Examples of additional dissections which can be done in unrestricted autopsies include the following: examination and sampling of musculoskeletal system in all areas except hands and face; dissection of deep veins of leg in cases of pulmonary emboli (dissection of deep veins of the arm may also be performed, but should first be discussed with the staff pathologist); arterial dissection of legs; temporal artery biopsy; removal of tongue. As already mentioned, examination of a-v fistula may be required in certain dialysis patients presenting with septicemia. It is important that the funeral home be notified, in most instances before beginning the procedure, in cases which will require unusual or complex dissections. Such communication is both a simple courtesy and also promotes a good working relationship with the local funeral homes. A. Dissection- NOTE: The following guidelines refer to the typical unrestricted adult autopsy. These steps may require modification in individual cases, particularly in those patients who have had extensive thoracic or abdominal surgery. If restrictions include “return organs to the body”, you will need to photograph all findings in the fresh state and take microscopic sections at the time of the autopsy and return all the organs to the body cavity in a plastic bag at the end of your dissection. The brain will be cut fresh by the neuropathologist. 1. Before beginning dissection, it is important to perform a thorough external examination (don't forget to examine the back) and to document findings. Photographs and drawings may be used when appropriate. A note as to how the body was identified should be included. The presence of scars, open wounds, tubes/drains, intravenous catheters, endotracheal tubes should be noted. Take care to note the presence of personal objects on the deceased (such as rings, watches, bracelets); the presence of these objects at the time of autopsy should be noted in the case book — e.g., "yellow metallic ring noted on left ring finger." 2. Occasionally it may be necessary to investigate the possibility of PNEUMOTHORACES, AIR OR FAT 22 EMBOLIZATION. These investigations should be done early in the autopsy, generally before cultures are obtained. The pneumothorax test is done before the chest plate is removed. The skin and subcutaneous tissue flaps of the chest wall are used as a sac to which water is added, such that the water level is higher than the mid-axillary line. A puncture is made below the water line and just superior to a rib, and the puncture is extended into the pleural cavity. Simultaneously, the water within the chest tissue sac is carefully examined, looking for the exit of air bubbles. A similar approach can be used to search for air in the heart, using the pericardium as a sac. If you are uncertain as to how this is done, please call your staff pathologist. 3. In order to detect FAT EMBOLIZATION, it is best to obtain a fresh sample of either blood clot, generally venous, or lung tissue. A frozen section can then be done on tissue or clot, followed by an oil red 0 stain, which detects neutral fat. Oil red 0 stain may also be done on formalin-fixed tissue which has not been processed in alcohol. 4. In routine cases, the body is opened via a Y-shaped incision. After the Y-shaped incision is made, proceed as follows: i) ii) iii) 5. Measure abdominal panniculus. Remove chest plate and a sample of blood via needle puncture of the inferior vena cava (after appropriate heat sterilization). If clot in the IVC prevents blood collection, one may incise the ventricles and use the pericardium as a sac to collect a blood sample. If the heart is devoid of blood, as in a case of exsanguination, one can often collect blood by needle puncture of the pulmonary arteries. Cultures of lung (submit tissue, not a swab), effusions (pleural, pericardial, peritoneal), abscess cavities, or other sites of suspected infection can be obtained at this time as well. Palpate the accessible part of the pulmonary artery and its major branches, then make incisions into these structures to check for large emboli (these may become dislodged upon evisceration of the thoraco-abdominal block). The retroperitoneum and other body cavities should be inspected in situ. iv) The small and large intestines are next removed by tying-off the bowel at the ligament of Treitz and at the recto-sigmoid junction. In routine cases (i.e., bowel appears unremarkable), the intestines can be removed by cutting along the mesenteric surface. In cases of suspected bowel infarction or other instances when it may be useful to examine the intestine with its vasculature intact, one should leave the intestines attached to the abdominal block and dissect them later, maintaining the relationship of the intestine to its vascular supply. The intestines should also be retained, attached to the abdominal block in cases where these cannot be easily separated, such as in peritoneal carcinomatosis or when there are multiple, dense, fibrous adhesions v) The main arteries of the neck and upper extremities are isolated and tied-off (subclavian, common carotid), and the common iliac arteries are isolated and tied-off. This makes it easier for the funeral home to identify major arteries and to perfuse the extremities and head after autopsy. vi) The iliac veins should be inspected, palpated and then transected. The lower extremities should then be "milked" to assess the patency of the deep venous system. NOTE: Flow of blood from the transected iliac veins does not entirely exclude a thrombosis of deep leg veins, and additional dissection (e.g., of popliteal vessels) may be needed in individual cases. vii) The organs are then eviscerated en bloc from the level of the larynx, caudal to the prostatic urethra or upper vagina via the Rokitansky method. NOTE: Eviscerations, including brain removals, are generally performed by Pathology Associates or Assistants; however, residents will be required to learn how to perform such procedures and will be given enough practice in such to become proficient. Residents will be expected to perform at least two complete eviscerations by the end of their first year viii) If the intestines have been removed separately, they should be inspected externally (note the presence, position, and condition of appendix) and then opened along the antemesenteric surface. The mucosa should be examined throughout, with care taken not to rub the mucosal surface too vigorously. The bowel should then be placed in formalin, pending review by the staff pathologist. Staff pathologist residents may not need to show the staff pathologist the entire bowel if it is unremarkable, but need only save representative segments for the stock bottle. The individual blocks are next separated, as follows: 23 i) From a posterior approach, transect the thoracic aorta at the level of the diaphragm, and free-up the esophagus and reflect it inferiorly. After cutting the inferior vena cava at its entrance into the right atrium, one has divided the thoraco-abdominal block into two blocks, the first (#1) consisting of the cardiopulmonary system, mediastinal tissues and neck organs, and the other (#2) consisting of peritoneal, retroperitoneal and pelvic organs and structures. ii) Examine the main pulmonary arteries and its branches; if pulmonary thromboemboli are found, one must search for a venous source. This includes examining the IVC, hepatic vein and iliac veins, which are located in block #2, and the lower extremity veins. The deep veins of the lower extremity are dissected via a posterior approach. (Residents will receive instruction in performing this dissection.) It is rarely necessary to dissect the deep veins of the arms; if it does appear necessary, consult your staff pathologist 6. Remove adrenal glands; weigh, measure, and serial-section; then place in formaldehyde 7. The next block can be dissected by opening the larynx and trachea longitudinally via a posterior approach. If necessary, the parathyroid glands (usually four are present) can be identified at this time. Most will be found posterior to the thyroid gland along a line connecting the inferior and superior thyroid arteries. (Sample parathyroids in patients with calcium abnormalities and/or chronic renal failure.) The thyroid gland should be removed intact, weighed, and serially sectioned. 8. Block #2 can now be dissected. By a posterior approach, the descending aorta can be opened longitudinally down to its bifurcation. The iliac arteries should then be opened in a similar fashion. Identify the renal arteries and make cross-sections to assess their degree of luminal narrowing. Occasionally, in cases of bowel infarction, it is necessary to identify and remove the arterial supply of the bowel. This is done by keeping the aorta, its branches, the mesentery and bowel together as one piece. The celiac artery, SMA and IMA are identified. The vessels are then serially sectioned in the intact specimen to assess the extent of luminal narrowing and to evaluate the presence of clot and/or atherosclerosis. Occasionally it is necessary to fix and decalcify heavily calcified vessels. The portal venous system can be examined in a similar way by dissecting inferiorly from the portal vein to its various branches. 9. The aorta, its bifurcation, the kidneys, ureters and pelvic organs can then be dissected away from the anterior structures by transecting the anterior branches of the aorta and separating the tissue planes. The kidney capsules are removed, the cortical surfaces examined. As in a surgical specimen, the most proximal ureter is opened, probes are inserted in the kidney pelvis to each of the poles to guide a cut (using a long knife) through the collecting system to bivalve the kidneys. Kidney weights and cortical thickness measurements are made. The calyces are opened. The ureters are then opened longitudinally to their entrance into the bladder. The bladder is opened, and the urethra is opened longitudinally as well. In males, the prostate should be serially sectioned in 5-mm sections. Special attention should be paid to pelvic venous structures (prostatic plexus in males) to look for possible thrombi, especially in cases of pulmonary emboli. In females, the pelvic organs (if present) should be measured, and the endocervical and uterine cavity opened, then the myometrium and ovaries sectioned. At the infero-posterior portion of this block will be a segment of rectum which can be opened longitudinally. 10. The remaining block consists of esophagus, stomach, duodenum, extra-hepatic biliary tree, liver, pancreas, and spleen. The initial approach to this specimen is to open the esophagus, stomach and duodenum longitudinally and examine the mucosa. In suspected cases of varices, the stomach and esophagus can be turned inside-out to best visualize the varices. Contact the staff pathologist for instruction in this technique. The ampulla of Vater is identified, and the common bile duct is opened. The cystic duct is opened into the gallbladder, and then the hepatic ducts are opened. Any stones present within the gallbladder or common bile duct should be characterized, documented, and (if indicated) retained at 4°C for possible chemical analysis; contact Gary Horowitz for further instructions. (This is especially important in potential medicallegal post-surgical cases.) The liver is weighed and serially sectioned into 1.5-cm sections. The pancreatic duct and splenic artery are opened, and the pancreas is serially sectioned (if stones are present, these should be characterized and, in some cases, saved for chemical analysis). The spleen is weighed and serially sectioned as well Adult Cardiac Examination: 24 Dissection strategies are based on underlying disease states and optimal methods for visualization and demonstration of specific cardiac pathology. In general, residents should discuss planned strategies with the staff pathologist prior to evisceration The cardiac pathology service at Brigham & Women’s hospital is available for consultatoin. Contact Robert Padera, E-mail: rpadera@partners.org Beeper 732-5700 #37451 or the BIDMC staff member may call the BWH “on-service” carciac pathologist Non-Cardiac Deaths (Assumes cause of death is known) A. After the breast plate has been removed, the pericardium is incised its full length to expose the heart. Observation of the amount and quality of any pericardial contents (serous, serosanguinous, frank blood, etc.) should be documented. The main pulmonary artery should be opened in-situ and the presence of thrombus assessed. The heart is lifted at the apex and blood cultures (if warranted) taken from the inferior vena cava. The heart is then excised by cutting across the inferior vena cava, reflecting the heart superiorly. From the backside of the heart, the insertion of pulmonary veins into the left atrium is identified. Transection of the pulmonary veins, pulmonary trunk and aorta is performed circumferentially. B. The heart is weighed and the coronary arteries palpated. If significant coronary artery disease is found (calcification along major tracts of coronaries), it is best to perfusion-fix the heart and dissect the coronaries free after fixation (see Fig. 1). Fresh heart dissection can be performed if appreciable coronary artery calcification is not found. The coronaries should be incised in-situ every 2-3 mm to document absence of disease. Cuts should be superficial so as not to enter the myocardium. An understanding of coronary anatomy is necessary to complete this task. Once the coronaries have been evaluated, the heart is serially sectioned from apex to base at 0.5-cm intervals. Myocardial cuts should stop 1.0 cm below the tricuspid and mitral valves. Attention is then directed to the base of the heart. C. The right atrium is opened with the incision extending to the right atrial appendage. A cut is made in the lateral right ventricular wall, opening atrium and ventricle. The right ventricular outflow tract is identified and a knife inserted to open the pulmonary outflow tract. Attention is then directed to the left side of the heart. The left atrium is opened through the pulmonary veins and carried out to open the left atrial appendage. A knife is passed through the mitral valve, and the lateral free wall of the left ventricle is incised. The final cut places the knife through the aortic valve with the incision passing through the anterior left ventricular wall. These cuts are referred to as cutting the heart “along blood flow lines” and are standard cuts D. The benefit of this method is that it is quick, allows immediate examination of the coronaries, myocardium, valves and any congenital abnormalities such as ventricular septal or atrial septal deficits. The downside is that unsuspected coronary artery disease can be missed, unsuspected infarction can be missed, and, finally, presentation points will be lost in a poorly performed fresh dissection Cardiac Deaths A. Cardiac deaths requiring special imaging and/or dissection techniques are as follows 1. All sudden cardiac deaths (death for unknown cause) in people aged 18 years or older 2. All deaths within 30 days of a coronary intervention such as: a) angioplasty/stent/arteriography b) bypass surgery 3. 4. All deaths following valve replacement All in-hospital deaths with known myocardial infarction B. General Comments 1. In general, when removing the heart, it is best to transect the aorta at the level of the brachiocephalic artery. This allows enough room for a perfusion cannula. It is my opinion that a well-fixed heart is easier to dissect, preserves cardiac chamber morphology, and provides more information than many of the highly specialized techniques outlined in further sections (2-7). To that end, I prefer a large-bore cannula inserted retrograde into the aorta and the heart perfused through the coronary system (either native coronaries or those with grafts) at ~80-100 mm/Hg (Fig. 1). Perfusion fixation by this method will take anywhere from 10 to 30 minutes, depending on the patency of the coronary tree. Perfusion fixation should continue as long as needed to achieve the standard 10 to 1 volume ratio for tissue fixation. The heart is suspended with string to complete overnight fixation. This fixation is the method of choice when the cause of death is 25 uncertain and preservation of coronary anatomy and myocardium is essential. It should be evident that, in cases of uncertainty, pressure perfusion fixation is the best method. 2. Sudden cardiac deaths; possibly cardiac or suspected infarcts less than 6-12 hours-old a) Myocardial infarcts less than 6-12-hours-old have limited findings on H&E staining. If a new (acute)myocardial infarct is suspected as a cause of death, vital staining may be required to prove such an event. The heart is removed as previously described and the coronary vessels dissected fresh from the heart following known anatomic landmarks. The heart is cut in standard 0.5-cm coronal cuts, apex to base, and the central myocardial slice is placed into 37° succinate/tetrazolium solution. b) Viable myocardium has functional dehydrogenases which will reduce the clear tetrazolium solution to a purple-stained myocardium. In the case of an acute myocardial infarct, the myocytes do not have intact dehydrogenases, and, therefore, the myocardium cannot reduce the tetrazolium and remains pale-brown in the infarct area. The remaining myocardium should turn purple (internal control). Notify Dr. Hecht if there is a question of acute myocardial infarction less than 12-hours-old. 3. Cardiac deaths following angioplasty and/or coronary stents a) Successes and failures following coronary angioplasty have definite morphologic correlates which can only be diagnosed with appropriate post-mortem investigational techniques. The clinical scenario of death will dictate the method of evaluation. If possible, residents should review and discuss the angiographic findings of the case with the cardiologist prior to addressing the heart. These discussions are critical and often dictate the appropriate mode of investigation b) The default evaluation for acute death (<30 days) following coronary stenting consists of retrograde aortic perfusion, coronary dissection after 24 hours’ fixation, and x-ray of the coronaries to evaluate the stent position and status of the stent. The coronary artery involved with the stent, including proximal and distal, should be submitted for histologic evaluation. DO NOT attempt to cut across the stent. It is metal and will only crush and deform with your attempts. Early stents (< 30 days) can be gently removed from the distal coronary cuts. Later stents (> 30 days) require epoxy embedment and are not routine. Some cases will require clearing to see through the vessel wall. Segments are dehydrated through graded ethanols and are placed in methyl salicylate for 2 to 6 hours. The vessel will become translucent. This will not affect subsequent histology 4. Cardiac deaths following coronary artery bypass grafting (CABG) — Specialized Technique a) In-hospital deaths following CABG or death within 30 days of CABG should be evaluated with coronary artery and graft injection with radiopaque material. Caution is required while removing the breast plate, as internal mammary artery grafts will be adherent. Grafts and native coronaries are cannulated followed by infusion with 5% neutral buffered formalin. Ideally, diastolic pressure (80-90 mmHg) should be used. Hand injection with 50-cc syringes will be adequate to perfuse the heart prior to barium injection. Injection is followed with a barium/gelatin mixture using 20-cc syringes. Approximately 10 to 15 cc is all that is required. DO NOT FORCE THE INJECTION. If the formalin or injectate does not flow freely, it’s best to stop. If more than 10-15 cc is injected, you are over-injecting the heart, forcing injectate to the venous side, making the study useless. Extravasation of contrast material onto the epicardial surface will obscure arterial anatomy. Therefore, rinse off any extravasated material with warm water prior to x-ray. b) Following the barium/gelatin injection, the heart is immersed in 10% neutral buffered formalin for overnight fixation c) After fixation, the heart is radiographed prior to coronary dissection. The coronaries and grafts are dissected free from the myocardium, and the heart is cut in cross-sections from apex to base in 0.5-cm intervals. The base is opened along blood flow lines (see Section I, above). d) The dissected coronaries and grafts are x-rayed as are the myocardial cross-sections. Occlusion in grafts as well as in collaterals within the myocardium will be readily visualized. Coronaries and anastomoses should be decalcified before serial cross-sectioning. Anastomotic sites should be submitted entirely as serial cross-sections (Fig. 2). 5. Cardiac deaths following valve replacement and/or native valvular disease 26 Hearts should be retrograde-perfused via the aorta and immersion-fixed prior to dissection. Coronaries are dissected free, decalcified and serially sectioned in 2- to 3-mm intervals. The heart proper should be cut in a 4-chamber cut to demonstrate valvular pathology 6. Cardiac deaths in dilated or hypertrophic cardiomyopathy Since, by definition, cardiomyopathy is muscle disease in the absence of identified coronary artery disease or other primary cardiac muscle process, most cardiomyopathies have normal or insignificant coronary artery disease. I recommend retrograde perfusion via the aorta with overnight fixation. After fixation, the coronaries can be cut on the heart surface. A 4-chamber cut should be performed to demonstrate ventricular volumes. 7. Cardiac deaths to demonstrate infiltrative processes (amyloidosis, sarcoid, myocarditis, glycogen storage diseases, tumor, and hemochromatosis) Since coronary artery disease is usually NOT an issue, retrograde aortic perfusion is recommended with overnight fixation. Coronaries can be either cut on the heart surface or dissected free and cut after decalcification, if necessary. The heart proper should be cut in a 4-chamber cut configuration. 8. Cardiac - Final Anatomic Diagnoses (sample FAD) a) In general, for coronary artery disease cases, the FAD should reflect native coronary disease, any interventional procedures and pertinent negatives. For example: A. Atherosclerotic cardiovascular disease 1. Native coronary arteries (right dominant) a. Left main; 30% stenosis b. Left anterior descending; total occlusion with recent plaque rupture and overlying thrombus • status-post angioplasty (date) c. Circumflex; 70% stenosis d. Right coronary artery; 80% stenosis with sequential stenoses 2. Status-post coronary artery bypass (date) emergent a. Left internal mammary artery to left anterior descending; patent b. Saphenous vein graft to obtuse marginal one; patent c. Saphenous vein graft to posterior descending artery; patent d. Cannulation sites; intact e. Post-pericardiotomy pericarditis B. Myocardium, cardiomegaly 830 grams 1. Acute myocardial infarct. Anterior and septal left ventricular wall. Age ~3-5 days with reperfusion injury 2. Old myocardial infarct; posterior left ventricular wall with extension to right 3. Myocyte hypertrophy with dropout and interstitial fibrosis a. History of hypertension, clinical C. No significant valvular pathology 27 FIGURE 1 Formalin Perfusion 28 FIGURE 2 Coronary Artery and Bypass Graft Dissection and Block Submission (A-D) 29 Stock Bottle (retaining of organs for prolonged period) & Sections. A. Routine sections required on all cases are one cassette of lung, one cassette of heart, one cassette of liver and kidney, one cassette of bone marrow. Additional sections documenting findings should be guided by the attending. In addition, sections may also be requested at Gross conference. B. The following specimens should be placed in a “stock bottle” (one 2 pint white container) in all unrestricted autopsies; even those with “return all organs to the body”. Whole organs should not generally be kept beyond the autopsy conference in any case. 1. 2. 3. 4. 5. 6. 7. Section/slice of heart (LV and RV), and any tissue with pathologic findings (not the whole heart with valves and aorta) Sections (2-3 cm cubes) of lungs (from each lobe), thyroid, prostate, uterus with endometrium, ovaries, adrenal glands, breast, skin (e.g., from chest wall at Y incision), skeletal muscle (e.g., from psoas), bone (vertebral column), testis Sections (2-3 cm cubes) of liver and spleen, pancreas Sections (2-3 cm cubes) of each kidney (cortex & medulla). Do not save entire kidneys. Bone marrow –thin slice of spine or segment of rib. Short segments of small intestine (10 cm each of duodenum, distal ileum with cecum/appendix), large intestine (sigmoid), stomach and esophagus (5cm on either side of the GE junction). Small piece of any other organ not already mentioned or submitted for histology. B. Also save: Cardiac valves in cases with valvular disease (e.g., a stenotic aortic valve), lymph nodes in lymphoma cases C. In unrestricted cases, the entire brain is fixed for later sectioning. Brains can be cut in the fresh state in cases with no suspected neurologic findings, case that requires fresh tissue (ie. Metabolic disease), when the family requests that all organs be returned for burial WITH THE BODY, or in ME cases. In all ME cases, the dura should be removed from the bones of the cranial vault to look for subtle skull fractures. In all cases, the pituitary should be identified D. Autopsy conference 1. More tissue is saved for conference than will be stored in the stock bottle. The tissues not reserved for stock bottle and histology will be discarded as medical waste following conference or after 1 week of issuing a PAD. 2. Although families reasonably expect that organs will be returned for burial, they understand and sign a consent allowing us to retain tissues necessary for diagnosis. These fixed tissues are available for return until the time of discard (3 months following signout - CAP guidelines) 3. If organs cannot be presented to the staff pathologist in a timely manner (i.e. Infectious cases), entire organs may be maintained and discarded later as medical waste or transferred (on request) to the funeral home for burial. The decision and responsibility of choosing to retain whole organs will be that of the staff pathologist Autopsy Neuropathology The final part of the complete autopsy involves removal of the brain, pituitary gland, and spinal cord. This is usually done after the other organs have been removed. All of these tissues should be removed for neuropathological examination in all unrestricted autopsy cases. In patients with any neurodegenerative disease, or other major neurologic disease, the entire spinal cord should be removed, including the difficult-to-reach sections of the cervical spinal cord. In patients with a history of a neuromuscular disease, several muscles, including the quadriceps, should be snap-frozen and also sampled in formalin, and several nerves, including one sural nerve, should be preserved 30 separately. The pituitary should be placed into a labeled cassette and held. The following are minimum requirements and steps for fixing and evaluating brains (see Infectious Autopsy section for CJD brains): A. Brain at the time of autopsy (see I. below if organs are to be returned to the body) 1. Record fresh weight of brain in work book 2. Record in work book any gross abnormalities appreciated prior to sectioning, i.e., hemorrhage, cystic infarction, severe atherosclerosis, meningitis, severe autolysis, or indicate "grossly normal" 3. Properly label outside of brain crock and place label on basilar artery with the autopsy number, patient's name, and prosector's name 4. In cases in which the entire spinal cord is removed, the dura should be opened and pinned, so that the cord can be maintained in a straight configuration during fixation B. Fixation: 1. The brain crock is filled with formalin as follows: 1 to 1.5 Mason jars of concentrated formalin, followed by water until the crock is 2/3 full 2. The brain is then hung in the crock by suspending it via a string passed underneath the basilar artery. Suspend it in the formalin first, otherwise the basilar will break. Place the brain in a vented cabinet, and allowed to fix for one week; brains should be washed under continuous running water for at least 24-48 hours C. Brains may be donated to Harvard Medical School for medical student teaching, providing that the family has not specifically requested that tissues not be used for research or teaching outside of the Department of Pathology. In general, brains from individuals without neurological abnormalities, systemic disease, potentially infectious disease processes (HIV, HBV, TB) or metastatic tumor may be donated. The attending neuropathologist (e.g. Drs. Jeffrey Joseph or Matt Anderson) will decide which cases are most appropriate for donation. Needless to say, only uncut and properly fixed and washed brains should be donated. The fact that a brain was donated to HMS should be noted in the Autopsy Case Book. Donated brains still need to be examined! Any suggestion of pathology in the exterior requires a full dissection. D. Brain cutting (specific instructions on the proper way to cut a brain will be provided by the attending neuropathologist, e.g. Drs. J. Joseph or M. Anderson). 1. It is the resident's responsibility to check the brain cutting list and be prepared to cut the brains on the day they are scheduled. Occasionally a resident may need to be scheduled at a time when they are signing out surgical specimens or are covering the operating room. It is nevertheless his/her responsibility to have the brain cut ahead of time, or find appropriate coverage if necessary. 2. Record the weight of the formalin-fixed brain in the work book. 3. The prosector is responsible for bringing a copy of the patient's clinical summary and autopsy findings to the brain cutting. E. Gross photographs should be taken of any pathology that has potential teaching value, that will be used in conference, or that may come up at time of sign-out. The neuropathology attending should be consulted if one is unsure as to whether photos are necessary F. Notes must be taken and recorded in the autopsy case work book, even if findings are essentially normal. Important negative findings include: clear leptomeninges, vessels without atherosclerosis, absence of masses, hemorrhages, infarcts, or significant atrophy. G. Pink Cassettes must be properly labeled with the autopsy number and letter designation as follows: A02-098 A. Keep a key to match slide with anatomical site, list the stains you will need, and give a copy to histology with the cassettes. H. Brain sign-out: 1. Neuropathology final report should be issued within 12 weeks of the autopsy. This deadline may be extended in cases with many tissue blocks since they require special processing, but extensions must be 31 noted in writing in the patient’s folder in the autopsy office. I. 2. It is the resident's responsibility to arrange brain sign-out with the neuropathologist. 3. At the time of sign-out, residents should bring information regarding the clinical history, gross CNS findings and general autopsy findings. Cases of “return organs to the body”: 1. Call the neuropathologist to check if they want to participate and document their response in your notes (name, time, yes/no). If the brain is known to have significant pathology, all attempts should be made to change the permission and fix the entire brain. 2. Weigh the brain. 3. TAKE EXTERNAL PHOTOS OF THE INTACT BRAIN (TOP AND BOTTOM) with brain stem still attached. 4. Examine brain (cortex and white matter) and cord for focal lesions; infarcts, necrosis, tumor. Be sure to check for herniation (subfalcine, uncal, tonsilar). Cut off the brainstem then dissect the cerebrum coronally and the brainstem transversely. Examine ventricles for widening or granularity. Inspect caudate and basal ganglia for atrophy or asymmetry. Search for hemorrhages, lacunes, larger infarcts, masses, or vascular. Check the midbrain and pons for Duret hemorrhages. Look at the pigmented areas, including the locus ceruleus (upper pons) and substantia nigra (midbrain). Examine mammillary bodies for old/new hemorrhage and pons for central myelinolysis. The cerebellum may show abnormalities of the folia if the patient had been on a respirator, or vermal atrophy in alcoholics. Examine cerebellar white matter for atrophy. Record findings carefully, including clear notations on pertinent negative observations (as) relevant to the case. 5. Save the required slices in a small flat square containers. These will be fixed for 2-3 days and then transferred to the stock jar. However, no sections should be taken unless a lesion is found. 6. what to write: _____________________________________________________ A. Brain (XXXX g): 1. Hemispheres: convexities symmetric with a well-developed gyral pattern with clear leptomeninges. No localized external softening, hemorrhages, infarcts, masses, herniation (subfalcine or cingulate, uncal, or tonsilar), or contusions. 2. Coronal sections show intact cortical ribbon of appropriate thickness. Internal architecture has the usual pattern, without focal lesions or hemorrhages. The ventricular system is unremarkable, symmetric and of appropriate configuration and size. 3. Brain stem and cerebellum: Typical external configuration. Transverse sections of the brain stem show a well pigmented substantia nigra and locus ceruleus. The pons and olivary nuclei are unremarkable. Cerebellar hemispheres have usual foliar pattern and dentate nucleus B. Dura: unremarkable and sinuses are patent C. Circle of Willis/basal vasculature: normally formed and patent. No/minimal/non-occlusive atherosclerosis present in carotid arteries, main branches from circle of Willis, and basilar artery. D. Spinal cord: Dura intact and unremarkable. Leptomeninges are translucent. The anterior and posterior roots are comparable in size and bilaterally symmetric. Transverse sections of cord show no abnormalities. ______________________________________________________ 32 Slices to be saved: 33 IC SN H Love S, Histopathology 44;2004:309-317 Recording the Cause of Death A "cause of death" must be entered on the report of death and taken to the Admitting Office as soon as possible so that the body of the deceased may be released to the funeral home. Generally, the anatomical "cause of death" can be determined within 2-3 hours of the start of an autopsy. We should strive to keep to this time period. The staff pathologist should be consulted if possible on determining the cause of death, unless the cause is obvious - such as a ruptured aneurysm, large myocardial infarction, etc. Remember that one must list an anatomical cause of death (only one). Congestive heart failure, respiratory failure, or sepsis are clinical diagnoses and are not to be listed on the "cause of death" sheet (see Appendix 1) Reviewing the Case with the Staff pathologist; Sectioning, and Photography A. Following completion of the autopsy, the resident should contact the staff pathologist to review the fresh organs on the same day as the autopsy. Staff should discard most of the organs. These can be returned with the body to the funeral home in a doubled, closed biohazard bag. This is required by law if the family has indicated this as their preference on the Permit. When staff pathologists do not view cases on the same day, residents must fix the tissues in formalin-filled containers, sometimes up to three, drain the formalin, and wash the tissues the next morning for presentation (see section on “handling of tissues and formalin”), and after review, the tissues to be presented at conference must once again be placed in formalin for thorough fixation prior to presentation at Gross Conference. This is clearly a waste of formalin and time; additionally, it exposes personnel to greater 34 amounts of formalin than needed for a given case B. Residents should receive guidance with regard to examination of the small intestine and colon. Staff pathologists must make clear to residents how they prefer to handle bowel which appears normal to the resident. For example, some staff pathologists may want to be shown only bowel which appears abnormal, while other staff pathologists prefer to review the entire bowel. It is the Autopsy Directors' opinion that when fresh organs are examined by the staff pathologist that the bowel should be given the same review as any other organ. We will, however, leave the handling of this matter up to the individual staff pathologist's discretion and only ask that they make their wishes clear to residents C. Staff pathologists should provide guidance in deciding which organs should be saved for Gross Conference and which should be sampled for microscopy. (During the first two months of the academic year, it is appropriate to show all organs, both normal and abnormal, so that residents just beginning the program will develop a solid frame of reference. After this period, the Gross Conference should focus on abnormal findings.) This issue is of importance, since we have very limited space to store tissues D. Cases done late in the day or on weekends ordinarily are reviewed the next day or on the following Monday, respectively. In the latter instances, the organs should be fixed in formalin and placed in the vented cabinets (use plastic containers). To ensure uniform fixation, it is important to make slices in organs, use paper towels between tissue slices to allow good formalin permeation between slices, and line the bottom of the pan with paper towels to lessen "pan change." In particular, the cardiac chambers should be filled with paper towels or rubber gloves so that the fixed heart approximates its pre-fixation shape. Fresh tissues exposed to room temperature for 3 or more hours will show autolytic changes. It is therefore good practice to take small samples of the major organs for fixation early during the course of the autopsy E. A digital camera and camera-stand are available in the autopsy room for gross photography. A label with case number and ruler should be included adjacent to all organs photographed. Consult with your staff pathologist before discarding organs with important findings, as photographs may be indicated. Photographs should be taken after conference for all cases to be presented at the monthly Gross/Micro Conference. NOTE: Under no circumstances are fresh organs or any other potentially infectious materials to leave the autopsy room without the knowledge of the Director of the Autopsy Service F. Following completion of the autopsy case, the resident should do a basic cleaning of the work area (the major cleaning will be done by the Pathology Assistant). (Tissue to be discarded should be left in a pan with a sign stating "discard," and the Pathology Assistant should be notified of this in person. Do not leave fresh tissue on the counter without informing someone of its status, as such tissue may wind up staying out overnight or over the weekend.) The resident puts tissue in a plastic bag and freezes it. The tissue is discarded from the freezer on Wednesdays G. Autopsy cases should be sectioned after review with the staff pathologist, but no later than 2 working days after the autopsy. Additional sections might be requested following Gross Conference if additional findings are discovered. Tissue sections should be placed in green cassettes labeled with the autopsy case and cassette number. The resident should keep a key to match cassettes with a specific organ or pathological site. Two copies of the slide key are to be made. One is given to the Histology Lab with any tissue blocks submitted. The second is given to the autopsy secretary to be kept with the case folder. 1. Routine sections required are one section of: lung, heart, liver, kidney, bone marrow 2. Most cases can be adequately blocked in under 10 cassettes. Those requiring 15 or more are required to have the staff pathologist's signature on the log sheet. Preparation of Autopsy Documents (PAD/FAD) Note: The Autopsy Case folder must remain in the Department file at all times. Take copies of gross diagnoses or clinical summaries that are in the folder, but not the last copy. A. Gross Diagnosis- Provisional Anatomic Diagnosis (PAD) The resident should work closely with the staff pathologist in preparation of the Gross Diagnosis forms and other documents. A JCAHO regulation states that the preliminary or gross diagnosis must be in Medical Records within three working days of the day of the 35 autopsy. We should meet this requirement in every case. Each PAD/FAD MUST include a statement of the organs that were retained for prolonged fixation (not returned to the body cavity). “Organs retained for further study: Liver, spleen, heart, lungs, kidneys, adrenals, pancreas, brain…”. This statement is included in the templates. Note that while we strive for accuracy in the Gross Diagnosis, these documents are not expected to include the results of microscopic examination. Organ weights are included with expected values (Appendix 2). Thus, we should not delay submitting the Gross Diagnosis form in order to examine "rush" autopsy slides. Similarly, do not delay submitting the Gross Diagnosis simply because the case is potentially infectious and cannot be thoroughly dissected until after a 6-week period of fixative. State in the "Gross Diagnosis": "Body As-AWhole: Active hepatitis B infection (based on clinical data): organs will be fixed for 2 weeks before further gross and microscopic examination." This informs the clinicians about the status of the case, and tells them that the final sign-out will be delayed. It also satisfies the JCAHO request that the Gross Diagnosis form be submitted to Medical Records within 3 working days of the autopsy. If a brain is taken, the Gross Diagnosis form should state (if there are no grossly discernible lesions): "CNS: Brain, X-grams; complete examination will be performed and submitted in a supplemental report. B. Clinical Summary- The clinical summary should be prepared and reviewed with the pathology attending prior to issuing a PAD, however, the Summary is not part of the PAD and will not be sent out. The secretary will not keep a copy of the Clinical summary; Residents should save a copy of this summary and incorporate it into the final autopsy note in the FAD, or may attach a copy to the patient’s autopsy file. The clinical summary should be concise and summarize the hospital course. Completely restating physical examination findings, especially normal ones, or all laboratory data is not necessary. Be selective. One should strive to fit the summary onto one typed page. This summary should be objective and should avoid interpretation or extrapolation from data in the medical record. C. Final Diagnosis and Final Note- This part of the autopsy report must be completed within 4 weeks in the usual autopsy case. In infectious cases and those in which there are major CNS findings, the case should be completed within 12 weeks. (Place interesting or challenging microscopic slides from your cases on the Surgical Slide Conference tray for everyone's review.) D. Autopsy reports, including both the Gross and Final Diagnosis, should be distributed to all concerned clinicians. At a minimum, the list for distribution of reports should include the resident most involved with the patient's case and the staff physician responsible for the case (this is usually the physician whose name is on the patient's card, bracelet, etc.). Also list significant consultants (surgeons, angiographers, etc.). We are still working on establishing an "Autopsy Mailbox" in the Hospital computer system. This system, if established, would be another means of communicating autopsy findings. Any requests by family members for copies of an autopsy report should be referred to the Correspondence Office (667-3715). The Pathology Department does not handle the processing of such requests. E. Addendum: In cases in which the clinical data, and the gross examination of the brain, indicate that CNS findings are unlikely to have contributed to the patient's death, the results of the CNS examination can be reported in an addendum. This ordinarily permits a more rapid distribution of the Final Diagnosis form. In such cases, the Final Diagnosis should read, "CNS: Brain, X-grams, the results of a detailed gross and microscopic examination will be reported in an addendum." Such addenda should be distributed even if the examination discloses no findings, thus "closing" the case. If important or potentially important findings are disclosed, it is appropriate to send a short, additional "Final Note" with the addendum. Addenda may also be used to report results of other potentially time-consuming studies (chemical analyses performed outside the Hospital, external review of slides from the case by outside "experts," etc.). It is clearly preferable, however, to have these studies done rapidly enough to include the results in the original Final Diagnosis and Final Notes. In infectious cases (in which all organs are fixed before dissection), or in cases in which the CNS findings clearly are critical, the Final Diagnosis and Final Notes should be prepared only after both the general autopsy and neuropathological examinations are completed. 36 Communication of Autopsy Findings One of the important aims of the autopsy is to provide accurate information regarding the autopsy findings in a timely fashion to the clinicians and family of the deceased. It is especially important to maintain a system whereby major unexpected findings, especially those that may have public health implications, are reported promptly. Prompt follow-up is also indicated in deaths of patients on experimental drug and radiotherapy protocols or bone marrow transplantation protocols, so that modifications in these procedures can be considered. The following protocol should be followed in disseminating the information derived from postmortem examination. F. Even in the most routine cases, please contact either the patient's attending physician or major house staff physician immediately after completion of an autopsy to provide them with the major gross findings. While this is not mandatory, it takes little time and clearly can strengthen the clinician-pathologist relationship. It can be done by telephone or e-mail. G. Major new findings disclosed at autopsy, such as death due to an undiagnosed ruptured AAA, should be communicated as soon as possible. H. If the prosector/attending pathologist identifies or seriously suspects a major infectious disease (such as TB, HBV, HIV) at any point during the evaluation of an autopsy case, the attending clinician should be notified promptly either by telephone or by letter. Appropriate documentation of this communication should be retained in the Autopsy Case folder. An example of such an interaction is as follows: 1. "Dear Dr. 'X': Gross examination of the lungs of your patient, John Doe, revealed a caseous nodule in the upper lobe, strongly suggestive of tuberculosis. Histological sections including special microorganism stains will be processed promptly. In addition, tissue will be submitted for culture. Results of these studies will be communicated when they become available." 2. The pathologist/pathology resident should not wait until the final diagnosis/final note is completed to communicate such information. I. The prosector should perform directed biopsies and culture in cases where a major infectious process is noted incidentally at autopsy or in cases where there is a strong suspicion of a major infectious disease (such as viral hepatitis, TB) not previously diagnosed. The tissue specimens should be processed immediately, and the attending clinician notified promptly regarding the results of this examination. J. In autopsy cases being treated with extra precautions because of known HIV disease, HBV, TB, C-J, directed biopsies should be performed carefully on tissues or organs of major clinical concern or those that appear clearly abnormal at the time of evisceration. These tissue biopsies should be fixed overnight in formalin (except for C-J disease, where the fixation protocol in the manual should be followed) and then processed immediately so that a provisional microscopic diagnosis can be rendered. Infectious Autopsy General Procedures ( “STANDARD OPERATION PROCEDURE – Infectious autopsy” approved by Dr. JL Hecht on 10/10/03, 4/19/05 and reviewed by Infection Control nursing and Dr. Sharon Wright-Brodie of infectious disease in 1/06): (‘STANDARD OPERATING PROCEDURE - Handling Cases of CJD, Creutzfeld-Jakob Disease, or Prion Diseases’ adopted 11/8/01 by William C. Quist, M.D., PhD; Jo-Ann Rosol-Donoghue (MASCP) SLS and approved by Jeff Joseph, M.D., Ph.D. 11/01; 6/02; 5/06) A. 1. Autopsy pathologists and infectious disease clinicians are not in precise agreement as to what the minimum standard for performing an infectious autopsy should be. There is much inter-institutional variation in how such cases are performed. As noted above, our procedures for routine autopsies have been reviewed by the Hospital's Infectious Disease Department and Infection Control Nursing, who feel that the routine procedures adequately protect residents and pathology staff from pathogens such as hepatitis B, HIV, and tuberculosis. 2. In cases of known or suspected hepatitis (either non-A, non-B, or B), HIV, we follow the following procedures (Creutzfeldt-Jakob disease and SARS are special cases and is described below) 37 a) Personnel in the autopsy room at the time the case is performed should be limited to the deiner who performs the evisceration, and the Pathology resident. The same autopsy room dress used in noninfectious cases applies for infectious cases as well. Cut resistant gloves or long gloves are available (not just for known infectious cases), please ask the autopsy supevisor (Gail Howe). b) The case will not be presented at autopsy conference. c) Tissue blocks for histology (that is tissue in a cassette) should be fixed for 24 hrs before submitting. d) Otherwise, these cases are dissected like every other case. They should be dissected fresh. DO NOT just put the organ block intact in a bucket 3. In cases of known or suspected active tuberculosis, the situation is different since the worry is related to airosolization and duration of exposure, and there is a literature about the validity of precautions. a) Limit personnel to a Deiner and 1 resident. Wear an approved TB mask in addition to the usual personal protective equipment. b) A limited fresh dissection is necessary. DO NOT just put the organ block intact in a bucket c) The organ block is separated into the usual 3 organ blocks: heart/lungs, kidneys/pelvis, GI tract including large and small bowel) and each part is serially sliced and fixed for 2 weeks in a large formalin bucket before dissection. d) Prior to large bucket fixation, small chunks of each organ (slice of heart, liver, kidney, bowel…) are put in a stock jar to ensure that something will be well fixed for histology. 4. Additional tips: a) Inflate the lungs through the trachea (DO NOT detach the lungs); this will limit splashing during inflation. Weigh the lungs by tipping them into the pan balance. b) Since the fixed gross organs from known infectious cases are not shown at conference, liberal use of gross photography should be made in these cases. B. Brain Removal and Fixation in Infectious Cases1. AIDS: Regardless of the clinical history, in addition to the brain, remove a small section of cervical spinal cord (removed through the foramen magnum) and segment of lumbar spinal cord, including cauda equina. Also remove a piece of skeletal muscle (pectoralis or psoas) and a piece of peripheral nerve (femoral nerve). If there is a clinical history of myopathy in an AIDS patient, also remove a piece of muscle such as quadriceps or gastrocnemius. All tissues should be fixed in 10% formalin for 1 week. 2. Creutzfeldt-Jakob disease (CJD), Subacute Spongiform Encephalopathy, or Prion Disease Cases: The purpose of this procedure is to address the current protocols to be followed when handling possible cases of CJD, Creutzfeld-Jakob disease, or prion diseases during autopsy. General rules: a) Use disposable, absorbent “chux” beneath all work being done b) Whenever possible, use disposable instruments (e.g. scalpel blades, forceps, wooden sticks, etc.) when handling the tissue, c) Note: Disposable instrument kits will be available in each morgue d) Discard all disposable instruments in the proper containers (sharps containers or red bag lined boxes for biohazardous waste) e) If you need to use regular instruments (scissors, hacksaw), soak the instruments in full strength bleach for 1.5 hours after finishing the procedure. Set a timer! f) Label all specimen containers and vials with “CJD” Precautions”. Performing autopsy: 38 a) Notify the attending neuropathologist (e.g. Dr. Jeff Joseph #35290 or Matt Anderson #31766). b) Unless there is an overwhelming clinical question, limit the autopsy to the brain. c) Use a hacksaw to open the skull. Do not use the electric saw (may aerosolize the tissue). d) Remove the brain in the usual manner. Save a sample of the cerebral cortex in a specimen container at –80C. Label appropriately. e) Fix the remainder of the brain in formalin until dissection. f) Dissect the brain in the standard manner. Block as in any dementia. Take three extra “scout” blocks, two of cortex and one of basal ganglia. g) Keep scout blocks in fixation at least overnight to complete the fixation. h) Using disposable forceps remove the tissue from the original formalin, wash briefly in water, and place the three scout blocks for one hour in concentrated (95%) formic acid. Use a timer! No more than one hour! i) Wash copiously in tap water and return to abundant, fresh buffered formalin overnight, to reestablish the correct pH. It is no longer “infectious”. Discard of the formalin in the original container as follows: a) On the “chux” place a Tissue-Tek Neutra-Pad (4295) b) Position the colored side of the pad facing up c) Formalin from the tissue will be absorbed and neutralized resulting in lower vapor emissions d) The used formalin from the container should be absorbed onto this pad or pads and absorbed e) Then wrap the chux around these pads and dispose of all in the biohazardous box Process the tissue: a) Process the formic-acid scout sections routinely, getting the more rapid H&E stains (i.e. not the usual LFB stains). You no longer need to indicate CJD precautions. b) Examine the H&E scout sections for spongiform encephalopathy. If the cortex or basal ganglia display significant vacuolization of the neuropil, especially in deeper cortical layers, then treat the remaining blocks similarly in formic acid. In the absence of spongiform changes, process the remaining blocks as any other brain autopsy specimens. Significant notes: a) Although the brain tissue is infectious, no data have demonstrated aerosolized transmission. The only documented routes of transmission are by direct implantation of infectious materials into the brain (e.g. with surgical instruments, dural grafts, corneal transplants), by administration of human-derived growth hormone, and probably by large oral inoculation of brain or spinal cord (Kuru, nvCJD or Mad Cow Disease). Nevertheless, you want to minimize aerosol exposure. b) The best tool to use to prevent infection is your brain! c) Follow all safety rules/precautions d) Wear all appropriate PPE (personal protective equipment) as outlined in the autopsy manual including “TB mask”. e) Dispose of all tissues properly. f) Label all potentially infectious containers. g) Wash hands thoroughly after any autopsy procedures. 39 C. Safe Handling of Human Remains of Severe Acute Respiratory Syndrome (SARS) Patients (Interim CDC Guidelines – May 3, 2005). We conform to these guidelines. Severe acute respiratory syndrome (SARS) is a respiratory illness caused by a coronavirus, called SARS-associated coronavirus (SARS-CoV). All postmortem procedures require adherence to standard precautions with the use of personal protective equipment (PPE) and facilities with appropriate safety features. Mechanical devices used during autopsies can efficiently generate fine aerosols that may contain infectious organisms. Thus, PPE should include both protective garments and respiratory protection as outlined below Objective: Safely handle human remains during autopsy procedures to prevent transmission of SARS-CoV. Activities In general, safety procedures for human remains infected with SARS-CoV should be consistent with those used for any autopsy procedure. However, additional respiratory protection is needed during an autopsy procedure that generates aerosols (e.g., use of oscillating saws). Personal protective equipment (PPE) Wear standard autopsy PPE, including a scrub suit worn under an impervious gown or apron, eye protection (i.e., goggle, face shield), double surgical gloves with an interposed layer of cut-proof synthetic mesh gloves, surgical mask or respirator, and shoe covers. Add respiratory protection if aerosols might be generated. This includes N-95 or N100 disposable particulate respirators or PAPR. Autopsy personnel who cannot wear a disposable particulate respirator because of facial hair or other fit limitations should wear a loose-fitting (i.e., helmeted or hooded) PAPR. Remove PPE before leaving the autopsy suite and disposed in accordance with facility policies and procedures. Engineering controls Whenever possible, perform autopsies on human remains infected with SARS-CoV in autopsy settings that have adequate air-handling system. This includes a minimum of 6 (old construction) to 12 (new construction) ACH, negative pressure relative to adjacent areas as per recommendations for AIIRs, and direct exhaust of air to the outside or passed through a HEPA filter if air is recirculated. Exhaust systems around the autopsy table should direct air (and aerosols) away from healthcare workers performing the procedure (e.g., exhaust downward). Use containment devices whenever possible. Use biosafety cabinets for the handling and examination of smaller specimens. When available, use vacuum shrouds for oscillating saws to contain aerosols and reduce the volume released into the ambient air environment. Prevention of percutaneous injuries Follow standard safety procedures for preventing percutaneous injuries during autopsy. 40 Fetal/Neonatal Autopsy Policy: Fetal autopsies are performed on involuntarily terminated pregnancies in which the fetus is either greater than or equal to 20 weeks' gestation (determined by dates and/or ultrasound) and/or greater than 350 grams in weight. It is required by law (MGL c.111, section 202) that the death be registered with the department of public health. an autopsy permission form must be completed which should include signatures of both parents, assuming both are known and actively involved. All fetal deaths below these cutoffs should be handled as surgical specimens. Voluntarily terminated pregnancies (Fragmented fetus or POC), irrespective of gestation or weight, are handled as surgical specimens. (Exceptions are therapeutic procedures designed to deliver an intra-uterine fetal demise [IUFD] or impending IUFD. Such cases are considered fetal deaths if they fall within the established weight and/or gestation.). It is a responsibility of the after-care team to arrange for photography of the deceased fetus. Pathology is not responsible for this activity. The autopsy should not be delayed any longer than 1-2 hours because photographic services are not available. The general autopsy attending will be responsible for all cases except those that involve known anomalies or genetic aberrations. Cases with congenital abnormalities (by ultrasound or by external exam) will be referred to Dr. Jonathan Hecht. Fetal/neonatal cases are occasionally referred to the Children's Hospital Department of Pathology for autopsy. The decision for referral should be made by Dr. Hecht or (if he is not available) the autopsy staff pathologist. The indications for referral are as follows: 1. multiple congenital anomalies; 2. prior amniocentesis documenting a genetic abnormality; 3. parents and/or clinicians wish that a case be referred. A case referred to the Children's Hospital will still be given a BIDMC autopsy number. The Beth Israel Deaconess Medical Center Pathology resident who gets credit for the case is responsible for seeing to it that the fetus arrives at Children's and is returned to Beth Israel Deaconess Medical Center upon completion of the autopsy, and that the cause of death is submitted promptly. The resident is encouraged to view the autopsy at the Children's Hospital Department of Pathology. AUTOPSY PROCEDURE A. Verify that we have the placenta in pathology B. Read the mother (and baby) charts 1. Maternal/gestational ages 2. History of fetal loss (SAB), therapeutic abortions (TAB), siblings 3. Social history (drug use, toxin exposure) 4. Prenatal care, screening (infections, Diabetes, cytogenetics/AFP), and risk factors (smoking, prior fetal losses, incompetent cervix or anatomic defect) 5. Complications (Preecclampsia, hypertension, placenta previa, twins) 6. Prenatal ultrasound (fetal anomalies, small for dates, oligohydramnios) C. Look at the baby/fetus with a senior before cutting anything! D. Take photographs – face (front AND side view), full body (front/back), hands (palms)/feet (profile). The hand/feet photos are not necessary if the appropriate views (see example below) are represented in the body shots. Remember what you need to see: Genitals, neck, palms, side view of the feet, front and side view of the face, abdomen. 41 If the hands are folded on the abdomen or hands are palm side down, or the cord is covering the genitalia or the feet are flopped to the side rather than frog-legged, you are WRONG! E. Weight the fetus F. Take an AP X-ray if indicated (external limb anomalies, ultrasound abnormalities, or internal findings on dissection – TE fistula, renal anomalies) G. Take cytogenetics (Skin down to fascia, and liver) if there are 2 or more structural anomalies (1 anomaly in a fragmented fetus), or requested by the clinician H. Open chest/abdomen using the standard Y-shaped incision (REMEMBER THAT YOU WILL BE SEWING UP THE SKIN LATER as in an adult autopsy) noting any abnormalities of organ position (situs inversus, diaphragmatic hernia (trisomy 18), congenital renal tumors) I. Cultures of the lungs and spleen may be taken now if there is a question of infection/sepsis J. Remove/weigh the thymus. K. Remove the gonads – they will otherwise be lost L. Take out the block intact including the tongue M. Remove brain using the biparietal incision (REMEMBER THAT YOU WILL BE SEWING UP THE SKIN LATER) (and spinal cord), weigh and fix for later exam N. Open the esophagus in-situ to look for tracheoesophageal (TE) fistulas O. Continue examining through the stomach and duodenum to look for duodenal atresia 42 P. Detach all the organs, weigh them and note any abnormalities (important weights are thymus, liver, heart, combined lungs) 1. Lungs – combined weight, look for abnormal lobation, petechiae 2. Heart (ventricles should be about equal in size, aorta should be anterior) If there was any question of cardiac disease, leave the heart/lung block undissected in a small formalin container for consultation. Otherwise, open the atria (snip off the tip) i) Cut the lateral right free wall to the apex. Probe the pulmonary outflow tract to see if there is an overriding aorta, and the cut out the outflow on the anterior wall along the septum. Note the foramen ovale in the posterior atrial septum (there should be a flap covering it, but a probe can get through), and the tricuspid and pulmonic valves. ii) The ductus arteriosus is the extension of the pulmonary trunk beyond the branches to the lungs. There should be a sharp transition to gray endothelium. If you see it, then the DA is patent. iii) Open the left ventricle by cutting along the anterior and posterior septum to create a free wall flap. This exposes the ventricular septum. Note the mitral valve then cut along the outflow tract (through the septal leaflet of the mitral valve) to reveal the membranous septum and aortic outflow. This is the most common site of VSD. 3. Kidneys – combine weight, look for hydronephrosis, misplacement, horseshoe fusion Q. Submit sections (mixed cassettes , but bowel and gonads should have their own cassettes): 1. 2. 3. 4. 5. 6. Thymus Lung (part of each lobe – not specifically identified) GI (from all segments – do not open the bowel) Gonads (with uterus and tubes in a female) Kidneys, adrenals (both sides) Skeletal muscle (diaphragm or tongue) R. It is the resident's responsibility to pack the fetal body cavities, sew the skin back together, and wrap the fetus upon completion of the autopsy. Use the straight needle-silk sutures in the morgue. 43 Perinatal Checklist: External exam (DO NOT DICTATE ALL THESE ELEMENTS, JUST LOOK FOR THEM) 3) General body habitus: 1. Macrosomia (diabetes, Beckwith-Weidemann syndrome). Is it symmetric? (head and body are both big) 2. Edematous (hydropic) 3. Macerated with skin slippage B. Head: 1. Epicanthal folds (Down’s) 2. Excessive wrinkles under eyes / flat nose (potters) 3. Cleft lip or Palate (LOOK IN THE MOUTH) (trisomy 13) 4. Protuberant tongue 5. Nose pressed down (Potters) 6. Flattened nasal brigde (Down’s) 7. Low set ears (top should be at the level of the outer canthus of the eye) 8. Overfolded/misshapen ears (potters) 9. Scalp defects (trisomy 13) 10. Short neck (trisomies) C. Thorax: 1. Short sternum (should be half way from internipple line to umbilicus), tri18 2. Nuchal (back of the neck) thickening or hygroma (swelling of the neck) 3. Spinal fusion defects/spina bifida S. Abdomen: defects in wall T. External genitalia: 1. Male- fused scrotum, testes descended or abdominal, ?hypospadias 2. Female- patent vagina 3. Ambiguous (vs. not identified.) 4. Anus: Patent (VATER syndrome) F. Extremieties: 1. # fingers on each hand/foot 2. Syndactyly/polydactyly- specify if extra is near the thumb or pinky, or which fingers are fused (triploidy or tri 13) 3. Arthrogriposis/clenching/contractures (cns malformations) 4. Overfolded fingers (tri 18) 5. Short great toe (tri 18) 6. Joint webbing 7. Abnormal palm creases (simean crease or single flexure of 5 th finger) 8. Skeletal dysplasia on X-ray Measurements: A. Body weight: 1. Crown-rump length: 2. Crown-heel length: 3. Foot length: 4. Head circumference (at nipples): 5. Chest circumference (at nipples): B. Organ weights: 1. Thymus 2. Lungs (Combined) 3. Heart 4. Liver 5. Kidneys (combined) 6. Brain P/FAD format: – Liveborn/stillborn (macerated) female/male fetus (__wks by foot length, __wks by crown-rump length, __wks by clinical/US at __wks) 44 – – – Probabale CAUSE OF DEATH: (multiple congential anomalies, placental abruption, chorioamnionitis, prematurity, indeterminate) •Fetal pathology •Placental pathology •Ancillary studies (cultures, cytogenetics) Major findings not associated with the cause of death (review of systems) Placental pathology (S02-XXXX) AUTOPSY SUMMARY: • Summarize the clinical scenario (1-2 sentences) • External findings (Grossly normal, well developed female fetus; Markedly macerated male fetus; Fragmented fetus of indeterminate sex) (1-2 sentences) • Describe findings listed above (b) • Synthesize the data What went wrong (cause of death) Likelihood of recurrent loss USE YOUR RESOURCES (genetic counselors, gynecologists, children’s pathologists, etc. Call them without hesitation). This is your chance to learn 45 ADULT TEMPLATE: BETH ISRAEL DEACONESS MEDICAL CENTER 330 BROOKLINE AVENUE BOSTON, MASSACHUSETTS 02215 AUTOPSY REPORT #A04-010 Name: Smith, John Age: 65 Hospital #: 1234567 Sex: Race: Caucasian Restrictions: None Date of death: 9/6/04 Hour of death: 8:58 AM Date of autopsy: 9/6/04 Date of PAD: 9/8/04 Date of FAD: Prosector: J.Smith J. Jones Male Clinical Service: Medicine Report to Dr(s): Dr. J. Simpson Staff Pathologist: J. Partridge, M.D. _________________________________ Provisional/Final Anatomic Diagnosis For PAD only (remove from FAD): PLEASE NOTE: THIS IS A PRELIMINARY (GROSS) REPORT AND IS PENDING MICROSCOPIC EXAMINATION. FINAL ANATOMIC DIAGNOSIS TO FOLLOW. II. External Examination A. Body Habitus: Height = _’__”, weight: ___ lbs (from chart). B. Eyes: COLOR, pupils (A)SYMMETRIC. C. Mouth: (i.e. poor dentition, upper and lower dentures). D. Skin/Scars: 1. COLOR (i.e. Jaundice with scleral icterus). 2. LESIONS (i.e. Petechial rash, both legs). 3. SCARS (i.e. s/p appendectomy, RLQ, 6 cm healed scar). E. Lines/devices: (i.e A-line, right antercubital, tracheostomy). F. Chest: (i.e. unremarkable, barrel chested). G. Abdomen: (i.e. mildly distended. prominent veins around the umbilicus/caput medusa) H. Extremities: (i.e. tattoos, edema, nail clubbing, hematoma). III. Cardiovascular System: A. Pericardium: (i.e. adherent, fibrinous pericarditis, effusion, tamponade). B. Heart (___ g): 1. Left ventricular hypertrophy (_cm, mid lateral ventricle). 2. (No) acute or remote infarcts. 3. Valves: (i.e. Mitral leaflets with myxoid degeneration, calcification of the mitral annulus, aortic cusps with calcification and stenosis). C. Coronary arteries (Left/right dominant): 1. LAD: __% stenosis (cross sectional area). 2. RCA: 46 3. Circumflex: D. Aorta: (i.e. moderate atherosclerosis, focally severe in the abdomen with stenosis of the renal arteries). IV. Respiratory system: A. Pleura: (i.e. fibrous plaques, effusions, 50 cc, adherence of parietal and visceral) B. Right lung (____ g): 1. MEDICAL (i.e. collapse, consolidation, hemorrhage, mild emphysematous changes, upper>lower lobes). 2. ). 3. NEOPLASTIC (i.e. tumor obstructing right main stem bronchus. Microscopic: squamous cell carcinoma). 4. INFECTIOUS (i.e. Targetoid lesions, necrotizing granulomas. Microscopic: aspergilloma. Cultures: positive for fungus). C. Left lung (____ g): 1. MEDICAL (i.e. collapse, consolidation, hemorrhage, mild emphysematous changes, upper>lower lobes). 2. NEOPLASTIC (i.e. tumor obstructing right main stem bronchus. Microscopic: squamous cell carcinoma). 3. INFECTIOUS (i.e. Targetoid lesions, necrotizing granulomas. Microscopic: aspergilloma. Cultures: positive for fungus). D. Trachea 1. (i.e. Erythematous mucosa adjacent to tracheostomy site, thick mucous secretions, trachea and bilateral bronchi, diffuse mucosal necrosis c/w prolonged intubation). IV: Gastrointestinal system: A. Esophagus: (i.e. unremarkable, intestinal metaplasia- 3 cm above the G-E junction, fibrosis c/w history of radiation, enlarged peritracheal lymph nodes). B. Stomach: (i.e. normal fold/no focal lesions, punctate superficial erosions/stess ulcers, diffuse thickening or mass. Microscopic: no evidence of viral inclusions. Gastric tube site remnant within stomach wall). C. Duodenum/small bowel: (i.e. unremarkable, mucosal flattening or ulceration. Microscopic: c/w peptic ulcer disease). D. Colon/rectum: (i.e. unremarkable. multiple adenomatous polyps, no carcinoma. 3 cm tumor mass in the cecum. Microscopic: andeocarcinoma, grade 3, stage 2 involving 10/10 region lymph nodes). E. Liver: (____ g): (i.e. mild vascular congestion, multiple white nodules, < 0.7 cm. Microscopic: metastatic small cell carcinoma.). F. Gallbladder: (i.e. distended with green bile. Single mixed-type gallstone.). G. Pancreas: (i.e. unremarkable. Fat necrosis c/w acute pancreatitis). H. Peritoneum: (i..e. serosanguinous effusion, 100 cc). V: Hematopoietic system: A. Spleen (___ g): (i.e. unremarkable). B. Lymphadenopathy: (tracheal, hilar, diaphragmatic, and peri-aortic). VI: Endocrine: A. Thyroid (__ g): (i.e. unremarkable, multinodular hyperplasia). B. Adrenals (right = _._ g, left = _._ g): unremarkable. 47 VII. Genitourinary system: A. Right kidney (___ g): (i.e. unremarkable, focal glomerulosclerosis). B. Left kidney (___ g): (i.e. unremarkable, focal glomerulosclerosis). C. Prostate: Nodular hyperplasia. D. Testes (L = __ g, R = __ g): unremarkable. E. Uterus, tubes and ovaries: unremarkable. VIII. Central Nervous System: A. Brain (___ g): See separate neuropathology report. B. Meninges: Unremarkable. In cases of “put back the organs” where neuropathology is uninvolved include: A. Brain (____ g): 1. Hemispheres-dorsal convexities: symmetric with a well-developed gyral pattern. No localized external softening of contusion. No displacement of the cingulated gyrus, medial temporal lobe or cerebellar tonsils 2. Coronal sections show intact cortical ribbon of appropriate thickness. Internal architecture has the usual pattern without focal lesions or hemorrhage. The ventricular system is unremarkable, symmetric and of appropriate configuration and size. 3. Brain stem and cerebellum: Typical external configuration. Transverse sections of the brain stem show a well pigmented substantia nigra and locus ceruleus. The pons and olivary nuclei are unremarkable. Cerebellar hemispheres have usual foliar pattern and dentate nucleus B. Dura: unremarkable and sinuses are patent C. Leptomeninges: transparent without subarachnoid hemorrhage or exudates D. Circle of Willis/basal vasculature: normally formed and patent. Minimal atherosclerosis is seen in carotid arteries without stenosis. E. Spinal cord: Dura intact and unremarkable. Leptomeninges are translucent. The anterior and posterior roots are comparable in size and bilaterally symmetric. Transverse sections of cord show no abnormalities. Organs retained for further study: Liver, spleen, heart, lungs, kidneys, adrenals, pancreas, brain. 48 Cassette Identification Key A= lung, left (upper lobe inked red, lower black) B= lung, right (upper lobe inked red, lower black, middle blue) C= heart (septum, left and right free wall) D= liver E= kidney F= bone marrow G= Sections corresponding to specific findings. Organ Heart Male Female RV Weight (g) Expected Organ Weights Change p/fixation Measurement (cm) -5.8% 300(270-360) 250 (200-280) 0.2-0.4 (measured 2cm proximal to pulmonic valve) 1.5 (measured 2cm distal to mitral valve) (circumference) 8.5 4.5-7.0 3.5-4.5 LV Aorta Ascending Thoracic Abdominal Lungs Right Left Liver Kidneys Male (combined) Female Cortex Medulla Adrenals (each) Male Female Parathyroids Thyroid Spleen Brain Male Female Cord 450 (350-570) 375 (325-480) 1650 (1500-1800) -4% +2% 313 (230-440) 288 (240-350) 0.6-0.7 1.3-1.7 9.7 8.3 0.12-0.18 (comb) 40 (30-70) <250 +15% +2% +9% 1400 1275 45 49 Final Note (Clinical summary) (Synthesis) (Cause of death) Note: Dr. _____ reviewed slide __ in consultation. Special tests performed: 50 Fetal Template: BETH ISRAEL DEACONESS MEDICAL CENTER 330 BROOKLINE AVENUE BOSTON, MASSACHUSETTS 02215 AUTOPSY REPORT #A04-087 Name: Harris, Twin B Age: 0 Hospital #: Baby (Mother) Sex: Female Race: Caucasian Restrictions: None Date of death: 8/18/04 Hour of death: 1:03AM Date of autopsy: 8/18/04 Date of PAD: 8/19/04 Date of FAD: Prosector: J.Smith J. Jones Clinical Service: OB/GYN Report to: Dr. J. Simpson Staff Pathologist: Jonathan Hecht, M.D., Ph.D. _____________________________________________ Provisional/Final Anatomic Diagnosis For PAD: PLEASE NOTE: THIS IS A PRELIMINARY (GROSS) REPORT AND IS PENDING MICROSCOPIC EXAMINATION. FINAL ANATOMIC DIAGNOSIS TO FOLLOW. I. External examination (expected values for gestational age): A. Phenotypically (i.e. male/female) fetus, __ weeks based on obstetrical ultrasounds. B. Skin: 1. Maceration with skin slippage over __% of surface. 2. (Skin defect in left leg, presumed cytogenetics sample). C. Measurements 1. Weight: _____ grams (____+___ g). 2. Crown-rump length: __ cm (___+_ cm). 3. Crown-heel length: ______ cm (____+___ cm). 4. Foot length: left ___ cm, right ___ cm (___ +___ cm). 5. Head circumference: ___ _cm. 6. Inner/Outer canthal distances: ___/___ . 7. (x-rays show___). D. Head and neck: 1. Hair: COLOR, DISTRIBUTION (single whorl, none). 2. Neck: (i.e. unremarkable, nuchal thickening or lateral neck webbing). 3. Ears: (i.e. normally formed, flattened, ear pits, patent canals). 4. Mouth/palate: (unremarkable, cleft hard palate/lip, hyperglossia, teeth). 5. Eyes: (i.e. symmetric, closed). E. Chest: (i.e. unremarkable, narrowed, widely spaced nipples). F. Abdomen/back 51 1. (i.e. Unremarkable, omphalocele, gastroschesis, distension, meningo-myelocele, sacral teratoma, lumbar midline defect). 2. Umbilical cord remnant: 7 cm long, 1 cm diameter, 3 vessels. G. Pelvis: 1. (i.e. male external genitalia, fusion in midline, descended tested; unremarkable ovaries, tubes and uterus). 2. Patent anus. H. Extremities: 1. Apparently proportional to torso without palpable fractures. 2. Feet: Five toes. No webbing, abnormal spaces between toes. 3. Hands: Five fingers. No webbing or abnormal palmar creases. II. Respiratory System: A. Patent trachea with no stenosis or atresia. No tracheoesophogeal fistula present. B. Lungs with normal lobation. Combined weight = _____ grams (__ g, expected). III. Cardiovascular System: A. Heart ___ grams (__ g, expected). B. Patent foramen ovale and ductus arteriousus. C. Cardiac chambers, AV valves and semi lunar valves grossly unremarkable. IV. Gastrointestinal System: A. No malrotation present. B. No atresia or stenosis present. C. Liver: ____ grams (__ g, expected), unremarkable with gallbladder. D. Pancreas: unremarkable. V. Genitourinary System: A. Left and right kidneys combined ___ grams (_ g, expected). No cysts. B. Ureters not dilated, bladder: unremarkable with urine. C. Two ovaries, one uterus: unremarkable. VI. Lymphohematopoietic System: A. Spleen: ___ grams: (i.e. unremarkable, accessory spleen). B. Thymus: ____ gram (__ g, expected): involution. VII. Endocrine System: A. Adrenals, combined weight ____ grams (___ g, expected): unremarkable VIII. Musculoskeletal System: Unremarkable IX. Cranium: A. Brain: __ grams (__ g, expected). See separate neuropathology report. B. Skull, small subgaleal hemorrhage and subcutaneous petechiae on surface of the cranium (non-specific) X. Placenta: (S0_-_______) A. PATHOLOGY REPORT. B. (summary of findings) 52 Organs retained for further study: Liver, spleen, heart, lungs, kidneys, adrenals, pancreas, brain. 53 Cassette Identification A= lungs,thymus, liver B= kidneys, adrenal, spleen C= gonads/uterus/tubes (wrapped on lens paper) D= GI tract, brain (if not taken for brain cutting) E= Heart FINAL NOTE (Clinical summary, ultrasound, genetics) (Synthesis) (Cause of death) Note: Dr. _____ reviewed slide __ in consultation. Special tests performed: 54 Autopsy Conferences The times and places of the Autopsy Conferences are as follows: The weekly Gross Pathology Conference will be held in the East Campus Autopsy Room every Thursday afternoon (11-12 p.m.) A monthly subspecialty autopsy Gross/Micro Conference is held on the last Wednesday of each month in the department conference room. Staff pathologist staff will request specific microscopic sections be shown to correlate with gross findings. This conference is coordinated with the chief resident. The conference is part of Quality Assurance/Quality Control, and a record of the findings is kept on file. The Pathology Department also participates in the weekly Surgical Morbidity and Mortality Rounds, and periodically in Medical Morbidity and Mortality Rounds. The surgical or medical coordinator will notify the Pathology Chief Resident(s) at least 5 working days in advance of autopsies to be presented at this conference. We should adhere strictly to this rule in order to allow sufficient time to prepare cases and to obtain Kodachromes, if needed. (Residents already should have photographed the significant gross findings.) The resident should organize their presentation and discuss the case with the Pathology staff member ahead of time. Generally, if microscopic sections are not available in time for this conference, microscopic follow-up can be given at a later date. On occasion, microscopic sections are crucial for the understanding and evaluation of a case. In such cases, one or two microscopic sections can be rushed so that information is available prior to the Surgical Conference. If this cannot be accomplished due to time limitations, the Chief Resident should request that the case be rescheduled. Observers A. Medical students and others (i.e. Pastoral care, researchers, residents from other departments) may observe autopsies, and may participate if directly supervised by the prosector or pathology staff. They must have permission from the director of autopsy or Dr. Connolly. B. All visitors must wear personal protective gear as described for residents. Their presence must be noted in the residents autopsy notes. C. They must understand that they are obliged to maintain patient privacy. Autopsy findings may be shared with the medicine teams who cared for the decedent, but only after the information is verified with pathology staff. Requests for Tissues for Research Purposes The Department of Pathology collaborates with several researchers from BIDMC and elsewhere in projects that utilize autopsy material. All collaborations must be approved in advance by the Director of the Autopsy Service, and requests for collaboration need to be made in writing and directed to Dr. Hecht. Quality assurance consists of microscopic correlation (GM conference), and reviews of 10% of adult PAD/FAD/NP on a quarterly basis by Dr. J. Hecht. 55 BETH ISRAEL DEACONESS MEDICAL CENTER Department of Pathology Autopsy Pathology Quality Assurance Monitoring Form Autopsy Effectiveness Report Pathologist Reviewer (ID Number)___________ Autopsy Number__________________ Autopsy Date_____________________ Date of Review________________ Patient Number_____________________________ Clinical Service_____________________________ Major Disease(s): Cause of Death: 1. Did this autopsy uncover a major disagreement in diagnosis? Yes______ No_________ If YES, check the following applicable categories: ______ Discrepant primary diagnosis with adverse impact on survival ______ Discrepant primary diagnosis with equivocal impact on survival ______ Discrepant secondary disease not directly related to cause of death, but was either symptomatic and should have been treated or could have eventually affected prognosis ______ Discrepant non-diagnosable (occult) secondary disease 2. Did this autopsy establish an unexpected or additional diagnosis? Yes______ No________ If YES, was this a ____ Neoplasm;____ Myocardial infarction;____ Infection;____ Other, specify: Would the clinical outcome been affected if this diagnosis had been known? 3. DID THIS AUTOPSY: (A) provide clarification of the clinical differential diagnosis? (B) confirm or verify the major clinical diagnosis? (C) provide information on any diagnostic procedures? Yes_____ No_____ Yes______ No_______ Yes______ No_______ Yes______ No_______ (radiologic?_____ endoscopic?______ other?____________________________) (D) provide information about any of the following areas? ____surgical pathology; _____cytopathology; _____hematopathology; ______ clinical laboratory; ____other_________ 4. Is there need to provide additional follow-up on this autopsy? If YES, please describe (USE BACK OF PAGE IF NEEDED) Yes______ No_______