Frequently Asked CAP Questions
advertisement

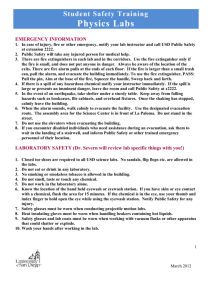
CAP- FEQUENTLY ASKED QUESTIONS MAY 2011 1. Attestation statementMust the Proficiency attestation page be signed both electronically and by hand by the techs performing the testing along with the director/ designee? While on a recent inspection we call in and were told the computer printed name was sufficient for the testing personnel. However, during the CAP audioconference today it was stated that both had to be signed. We would like to have this clarified as soon as possible of which is correct. Also, where can this information be found in the checklist? CMS – BOTH electronic AND written signatures are required on the attestation form You must be able to show who performed the testing for each challenge. It would be advisable to store all worksheets and test results together so that an inspector has access to all proficiency testing results with the attestation sheet. This is not in the current checklist; the instructions are included on the attestation sheet. It will be a part of ‘evidence of compliance’ in the July 2011 checklist. 2. Procedure Review: If a lab director signs a procedure indicating their approval, but the procedure is not effective until a later date, does the review date count from when the document becomes effective or the actual approval date? The review date will be based upon the date the director signed the procedure. 3. Annual Review Does the review date of a procedure have to take place before the actual signed date of the prior year, or is it alright as long as it is signed before the end of that review month. This was referenced during one of the audio-conferences, but I cannot find this in print. Effective with the release of the July 2011 checklist edition, the review period will be changed to every two years. We have not received clarification yet as to what variance will be allowed. 4. Emergency eyewash Emergency Eyewash facilities are required for areas where there are hazardous chemicals as defined by the laboratory’s chemical hygiene plan (e.g. chemicals that are irritating, corrosive, toxic by contact or absorption, etc.). For areas with hazardous chemicals, the 11 elements noted under Laboratory General Checklist item, GEN.72500 would be applicable and there are no exceptions for “grandfathered” eyewash facilities. It is recommended that the existing laboratories in the older buildings be evaluated to see whether it would be necessary to upgrade existing plumbing to meet the intent of this requirement. If no hazardous chemicals are in use, an upgrade to existing eyewashes may not be necessary. 5. If an Occult blood, which is waived, is performed in a moderate complexity lab, should they list the activity code as waived or moderate? Waived 6. Laboratory General Checklist item, GEN.41042, Refrigerator/freezer temperatures are checked and recorded daily. 1 LRRT/CAP’s FAQ 5-5-2011 CAP- FEQUENTLY ASKED QUESTIONS MAY 2011 The CAP requires that temperature monitoring be performed daily, including weekends and holidays. This does not mandate the need for a human to actually record the temperatures, however temperatures must be monitored. One acceptable approach would be to purchase “traceable” thermometers with time/date, min/max memory for temperature monitoring of the refrigerators/freezer when the laboratory is closed. If the temperatures exceed acceptable limits during the time when the laboratory is closed, the laboratory must have an action plan to check the contents for adverse affects. 7. Spill Kits GEN.72800, Explicit instructions posted, and appropriate supplies available, for the emergency treatment of chemical splashes and injuries and the control of chemical spills wherever major chemical hazards exist. NOTE: Spill kits must be handled in accordance with manufacturer instructions. If no expiration date is assigned, the spill kit must indicate the date it was put into service and the director must periodically assess its usability. You have asked for clarification of a major chemical hazard and whether there are limits or types of chemicals. You have also asked for a recommendation for handling spill kits without a manufacturer stated expiration date. An example of “major” hazards would be where chemicals are stored in bulk, such as gallon containers of formalin, xylene, alcohols, etc. The laboratory should have adequate spill-response equipment readily available, including appropriate PPE. To use the equipment properly, laboratory personnel who will respond to a spill or release of hazardous material must have appropriate training. In some cases, it may be appropriate that an in-house trained emergency response team deal with the situation rather than laboratory personnel. Appropriate emergency response procedures must be included in the laboratory’s Safety Plan. For laboratory spill kits without a manufacturer stated expiration date, the laboratory may consult with the manufacturer for its recommended time for expiration. If the manufacturer is not able to provide this information the laboratory may set an arbitrary expiration date based on the date it was put into service and the storage conditions of the kits. Some materials will have a considerable history and expiration dates can be projected with a certain degree of certainty. A yearly reassessment may be appropriate based on visible examination or other appropriate means (typically recommendations from manufacturer). Spill kit Expiration? Some spill kits have an expiration date. If there is no expiration, contact the manufacturer of the spill kit to obtain recommendations regarding the life/effectiveness of the spill kit so that an expiration date may be determined. Ultimately, it is the responsibility of the medical director to determine its usability. JH Health Safety and Environment’s response to spill kits usage: 1. The Mess up mitts can be used to clean up oil and organic/aqueous spills. 2. HSE approved the use of the spill kit for areas with limited hazardous chemicals- http://www.spillkit.com/drybox.htm 2 LRRT/CAP’s FAQ 5-5-2011