April 2014

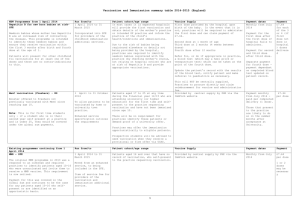
NEW Programmes from 1 April 2014
Hepatitis B for new born babies at risk- SFE
Newborn babies whose mother has Hepatitis B are at increased risk of contracting the disease. This programme is intended to identify these newborn babies and ensure they receive vaccination within the first 3 months after birth and fourth dose at the age of 1.
Patients will present for other childhood flu vaccinations for at least one of the doses and there are no contraindications to this.
Run from/to
1 April 2014 to 31 March 2015
Incorporated into SFE for providers of the childhood immunisation additional services.
Vaccination and Immunisation summary table 2014-2015 (England)
Patient cohort/age range
In most cases it is expected hospitals will provide the first vaccination and obtain details of the mother’s practice or intended GP practice and inform the practice of the child’s health/conditions and immunisations.
Due to the risk of babies being registered elsewhere or details not being provided by the hospital, practices are required to identify newborn babies registered with the practice (by checking mother’s status, not relying on hospital notice) who are at risk of Hepatitis B and provide appropriate vaccinations.
Vaccine Supply
First dose provided by the hospital upon birth of the baby. In the event that it is not, practices will be required to administer the first dose and can claim payment of £7.64.
Second dose at 1 month of age
Third dose at 2 months (4 weeks between doses)
Fourth dose after 12 months
Refer for, or do if appropriate in practice, a blood test (which may a heel prick or venepuncture test) which can be taken at the point of the fourth dose.
Update the patient’s record with the results of the blood test, notify patient and make referral to paediatrics as necessary.
This will NOT be centrally supplied. Practices to procure directly and claim reimbursement for vaccine and administration fee.
Provided by central supply by PHE via the ImmForm website
Payment dates
Monthly from July 2014
Payment for the first dose after the first dose if hospital fails to administer.
Payment for second and third dose after third dose.
Separate payment for fourth dose - payment dependant on completed blood test updated on patient record.
Payment
£7.64 for each of the
3 or 4 (if first dose not done in hospital) doses delivered
Payment monthly from
July 2014 - paid per completed delivery (1 dose).
Those that present to the practice are likely to do so in the summer months after acceptance at University.
£7.64 per dose
MenC vaccination (Freshers) - ES
Booster offered to freshers not previously vaccinated with MenC since reaching age 10.
Note: This is for first time students only - if a student who is in their second year self present at a practice and is under 25, they would be covered under the global sum payments.
1 April to 31 October 2014
To allow patients to be vaccinated by home or university town practice.
Enhanced service specification outlines the requirements
Patients aged 17 to 25 at any time during the financial year 14/15 who are attending university (or higher education) for the first time and self-present to the practice requesting vaccination and have not been immunised since age 10.
There will be no requirement for practices identify these patients or demand proof of a university offer.
Practices may offer the immunisation opportunistically to eligible patients.
Prospective students will be advised to seek vaccination when they receive a provisional or firm offer via UCAS.
Patient cohort/age range
Patients aged 16 and over that have no record of vaccination, who self-present to the practice requesting vaccination.
Existing programmes continuing from 1 April 2014
MMR – SFE
The original MMR programme in 2013 was a response to an outbreak and required practices to identify patients aged 10-16 who were unvaccinated and invite them to receive a MMR vaccine. This requirement is now retired.
Payment for this was covered in the Global Sum and continues to be the case for any patients aged 10-16 who self-present or are identified on an opportunistic basis.
Additionally patients over 16 who had no record of vaccination, who self-present to the practice requesting vaccination, were to be vaccinated. This is to continue.
Pertussis in pregnant women - temporary ES
Since 1 October 2012, a temporary programme of pertussis (whooping cough) vaccinations for pregnant women has been in place, while the JCVI evaluate the cost and clinical effectiveness of the programme.
Run from/to
1 April 2014 to 31 March 2015
Moved from an enhanced service, to being included in the SFE.
Item of service fee for providers of the vaccination and immunisation additional service.
1 April 2014 to 31 March 2015
Enhanced service specification outlines the requirements.
Vaccination of pregnant women and for new mothers who missed the opportunity to be vaccinated while pregnant.
Vaccine Supply Payment dates Payment
Provided by central supply by PHE via the ImmForm website Monthly from July 2014 £7.64 per dose
1 or 2 doses may be necessary
Provided by central supply by PHE via the ImmForm website Monthly from July 2014 £7.67 per dose – for each pregnancy
1
Rotavirus - SFE
From 1 July 2013, the rotavirus vaccine was introduced to the childhood immunisation schedule (at 2 and 3 months).
1 April 2014 to 31 March 2015.
Remains in SFE.
Children aged between 6 and 24 weeks. Provided by central supply by PHE via the ImmForm website. Monthly from July 2014 £7.64 for completed course - two doses
Existing programmes continuing from 1 August
2014
Seasonal Influenza for at-risk patients - DES/ES
The seasonal influenza programme is historically wider than the DES - as identified in the Green Book including pregnant women but excluding 2-4 year olds.
NHS England has now agreed to commission the flu immunisation for the wider risk groups identified in the
Green Book as from 1 April 2014.
Practices are required to call/recall the patient for vaccination.
Service delivered from/to
1 August 2014 to 31 March
2015
The DES Directions will not be updated to include at-risk group and pregnant women.
Instead, an enhanced service specification will reflect both the DES and the other risk groups as identified in the
Green Book.
Patient cohort/age range
The programme will mirror the at-risk groups in the
Green Book to include pregnant women, but excluding 2-4 year olds, as they are covered under the childhood flu programme.
Patients aged 6 -24 months in clinical risk groups need inactivated vaccine, which will be purchased and centrally supplied by PHE.
2-17 year olds need Fluenz or inactivated vaccine
(where Fluenz is contraindicated) which will be purchased and centrally supplied by PHE.
18-64 years in clinical risk groups and over 65s need inactivated vaccine and practices must procure from manufacturers themselves.
Vaccine Supply
There is a change to how the vaccines for at-risk children are supplied. All children aged 2-17 should receive Fluenz, as it is identified as the most clinically effective vaccine.
For children aged 6 months to 17 years, the vaccine will be provided from central supply by PHE via the ImmForm website. The PA fee will not be applicable for this age group.
Excluding at-risk children, practices are required to procure their own vaccine and should ensure they have enough other vaccines for contraindicated patients. Practices will be reimbursed for the cost of the vaccine and for an administration fee. Practices will claim these fees in the normal way.
Payment dates
Monthly from October
2014
Payment
£7.64 per dose
Childhood Seasonal Influenza ES
The children’s flu programme was introduced in
September 2013; the intended cohort is patients aged 2-
17 which will be rolled out over the next few years.
As from 1 April 2014, the enhanced service has been extended to include children aged 4, so that the new cohort is children aged 2-4.
Practices are required to call/recall the patient for vaccination.
Pneumococcal - DES
There is an addition to this programme to resolve a historic anomaly between the enhanced service and the recommended cohort as indicated within the Green
Book.
The requirement from 1 April 2014 will be to offer vaccination to patients who have achieved the age of 65
(during the financial year 14/15) AND to patients are identified as at clinical risk as indicated in the Green
Book,
Practices are required to call/recall the patient for vaccination.
Shingles routine aged 70 - SFE
Continuation of the existing programme to identify patients eligible for Shingles vaccination.
Vaccination of patients is on an opportunistic basis and can be done alongside the flu vaccination programme.
Shingles catch-up - ES
Continuation of the existing catch-up programme which
1 September 2014 to 31 March
2015
Enhanced service specification outlines the requirements.
1 August 2014 to 31 March
2015
The DES Directions incorporating this programme will come into effect 1 April
2014.
1 September 2014 to 31
August 2015
1 September 2014 to 31
August 2015
There is extension to the current enhanced service to include children aged 4, so that the new cohort is children aged 2-4.
Patients who have achieved the age of 65 or who meet the at-risk criteria identified in the Green Book.
Patients who have achieved the age of 70 but not 71 on 1 September 2014
From 1 April 2014 cohort extended to include patients aged 78.
There is a change to how the vaccines for at-risk children are supplied. All children aged 2 to 17 should receive Fluenz, as it is identified as the most clinically effective vaccine.
For children aged 6 months to 17 years, the vaccine will be provided from central supply by PHE via the ImmForm website.
The PA fee will not be applicable for this age group.
Practices will be required to purchase adequate number of vaccines to deliver the programme.
Practices will be reimbursed for the cost of the vaccine and for an administration fee. Practices will claim these fees in the normal way.
Provided from central supply by PHE via the ImmForm website
Monthly from October
2014
Monthly from October
2014
Provided by central supply by PHE via the ImmForm website Monthly from October
2014
£7.64
Single dose to last lifetime
Monthly from October
2014
£7.64 per dose
£7.64 per dose
£7.64
Single dose
2
aims for patients aged 71-79 to be vaccinated – the programme is phased in view of vaccine supply and available funding. From 1 April 2014, the age cohort has been extended to include patients aged 78.
Vaccination of patients is on an opportunistic basis and can be done alongside the flu vaccination programme.
Enhanced service specification outlines the requirements.
Identify patients who have attained the age of 78 and
79 but not 80 on 1 September 2014 and offer a shingles vaccination. to last lifetime
3