Modern Exudate Management
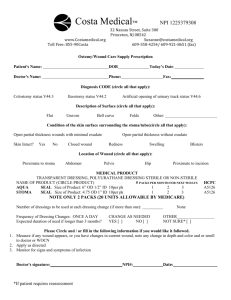
advertisement

Title Modern exudate management: a review of wound treatments Author(s) Richard White PhD Senior Research Fellow, Tissue Viability, Grampian NHS Trust, Aberdeen, Scotland, UK. Email: Richard@medicalwriter.co.uk Keith F. Cutting RN, MN, MSc, PGCE Principal lecturer, Buckinghamshire Chilterns University College, Chalfont St Giles, Buckinghamshire, UK. Keywords: wound exudate; exudate management. Key Points 1. The appropriate management of wound exudate requires an understanding of the underlying processes that lead to its production. 2. Exudate can present in a variety of forms, indicating the need to assess it by volume, viscosity and colour. 3. The selection of management options should be based on the characteristics of the wound and the needs of the patient. 4. Dressings may not always be the most appropriate option for exudate management. Consideration should also be given to physical methods of exudate control. Heading 1 Abstract Exudate must be effectively managed if the optimal moist environment necessary for wound healing is to be created, and the surrounding skin protected from the risks of maceration. To achieve these goals a detailed knowledge of dressing materials and their performance is required. An understanding of the impact of other treatments and co-morbidities on the production of exudate is also necessary. Exudate management is relevant to patient quality-of-life issues as it is often associated with leakage and malodour. It impacts on health economics because failure to control exudate production will lead to increased management costs and patient morbidity. This review considers exudate from the perspectives of its nature, composition, assessment and the range of management strategies available. Heading 1 Introduction The management of wound exudate requires the clinician to have an understanding of what it is, why it is present and how to accurately monitor and assess it. The production of wound exudate occurs as a result of vasodilation during the early inflammatory stage of healing under the influence of inflammatory mediators such as histamine and bradykinin. It presents as serous fluid in the wound bed and is part of normal wound healing in acute wounds. However, when the wound becomes ‘chronic’ and non-healing with persistent, abnormal inflammation or when infection becomes established, exudate takes on a different guise and generates clinical challenges. In the chronic wound, exudate contains proteolytic enzymes and other components not seen in acute wounds (1). This type of exudate has justifiably been termed ‘a wounding agent in its own right’ because it has the capacity to degrade growth factors and periwound skin and predispose to inflammation (2). In order to develop an effective management approach, the clinician must be able to accurately assess and understand the implications of the composition and quantity of exudate present in the wound. Heading 1 Exudate composition Wound exudate was described by the Swiss physician Paracelsus (c1491-1541) as nature’s balsam (3). It is derived from serum through the inflammatory/extravasation process. Acute wound exudate contains molecules and cells that are vital to support the healing process. It has a high protein content (although lower than that found in serum), with a specific gravity greater than 1.020. Its composition includes electrolytes, glucose, cytokines, leukocytes, metalloproteinases, macrophages and micro-organisms (4). In the first 48 to 72 hours after wounding, platelets and fibrin may be present, but this reduces as bleeding diminishes. See Table 1. Table 1: Some constituents of exudate and their functions. Component Function Fibrin Clotting. Platelets Clotting. Polymorphonuclearcytes (PMNs) Immune defence, production of growth factors. Lymphocytes Immune defence. Macrophages Immune defence, production of growth factors. Micro-organisms Exogenous factor. Plasma proteins, albumin, globulin, Maintain osmotic pressure, immunity, fibrinogen transport of macromolecules. Lactic acid Product of cellular metabolism and indicates biochemical hypoxia (5). Glucose Cellular energy source. Inorganic salts Buffering, pH hydrogen ion concentration in a solution. Growth factors Proteins controlling factor-specific healing activities. Wound debris/dead cells No function. Proteolytic enzymes Enzymes that degrade protein, including serine, cysteine, aspartic proteases and matrix metalloproteinases (MMPs). Tissue inhibitors of Controlled inhibition of metalloproteinases (TIMPS) metalloproteinases. As fluid passes through the inflamed vessel walls (extravasation) it may be seen that wound exudate is in essence modified serum and will therefore contain similar solutes. As it arrives at the wound surface, this fluid may be contaminated with tissue debris and micro-organisms (4). Healing acute wounds produce exudate containing active growth factors. These are not present in chronic wounds (6). Heading 1 Appearance of exudate Modest amounts of thin, pale yellow or straw-coloured exudate in an acute healing wound is considered normal. In chronic wounds, the colour, consistency and amount of exudate may change as a result of various physiological processes (4). Table 2: Types of exudate, their appearance and significance (4). Type Colour Consistency Significance Serous Clear, Thin, watery Normal. Possibly a sign of infection. Some straw- bacteria produce fibrinolysins, which degrade coloured fibrin clots or coagulated plasma. Some strains of Staphylococcus aureus, β-haemolytic group A streptococci and Bacteroides fragilis, produce fibrinolysins. Pseudomonas aeruginosa produces a non-specific enzyme that degrades fibrin. Fibrinous Cloudy Thin Contains fibrin protein strands. Serosanguinous Clear, Thin, watery Normal. pink Sanguinous Red Thin, watery Trauma to blood vessels. Seropurulent Murky, Thicker, Infection. yellow, creamy creamcoffee Purulent Yellow, Thick grey, Infection. Contains pyogenic organisms and other inflammatory cells. green Haemopurulent Dark, Viscous, Contains neutrophils, dead/dying bacteria and blood- sticky inflammatory cells. This means an established stained infection is present. Consequent damage to dermal capillaries leads to blood leakage. Haemorrhagic Red Thick Infection. Trauma. Capillaries are so friable they readily break down and spontaneous bleeding occurs. Not to be confused with bloody exudate produced by over-enthusiastic debridement. Footnote style Adapted with permission from Cutting KF. Exudate: composition and functions. In: White RJ, editor. Trends in Wound Care Volume III. London: Quay Books, 2004 (4). Heading 1 Exudate volume In chronic wounds the inflammatory response is altered owing to an uncontrolled expression of inflammatory mediators with a concurrent increase in vascular permeability and the amount of extravascular fluid. If the wound becomes infected, an abrupt increase in exudate volume may be seen initially, followed by further quantitative and qualitative changes. This has been attributed in part to specific bacterial virulence mechanisms that result in vasodilation and extravasation (7). Gautam et al (2001) (8) have described a process whereby neutrophils attracted to the site of injury trigger the release of heparin-binding protein (HBP). It has also been shown that chronic leg ulcer exudate contains increased levels of HBP when compared to acute wound fluid (9). It is likely that HBPs are implicated in the production of increased exudate. Certain bacteria such as Pseudomonas aeruginosa stimulate the release of HBP from neutrophils, thus aggravating chronic inflammation by augmenting endothelial hyper-permeability (9). Recent research has indicated that some bacteria actually express histamine and thus, if present, produce an additional physiological source of histamine to the wound environment. Morganella species, for example M. morganii Gramnegative rods have been found to express histamine (10). Bacteria isolated from chronic wounds have been found to produce physiologically significant levels of histamine (11) (12). It has yet to be determined if the production of this proinflammatory agent may be effectively managed through the application of antihistamines. The volume of exudate may be described using the terms shown in Table 3 (13). Table 3: Exudate volumes and their effects (13). Exudate Effect volume None Wound tissues dry. Scant Wound tissues moist. Small Wound tissues wet; moisture evenly distributed in wound; drainage involves 25% of dressing. Moderate Wound tissues saturated; drainage may or may not be evenly distributed in wound; drainage involves 25-75% of dressing. Copious Wound tissues bathed in fluid; drainage freely expressed. Footnote style Adapted with permission from Bates-Jensen BM. The Pressure Sore Status Tool a few thousand assessments later. Adv Wound Care 1997; 10(5): 65-73 (13). AWAITING PERMISSION Heading 1 Exudate assessment Accurate assessment of the volume and viscosity of exudate will indicate whether or not the healing is progressing normally (14). Inspection of a dressing on removal may yield valuable information on the level of exudate produced during dressing wear time. To assess the exudate volume the healthcare practitioner should count the number of dressings used over a time period, note the wear time for individual dressings, examine the dressing for the presence of strikethrough (wet or dry), examine the peri-wound skin condition and note any leakage (15). Some of the subjectivity attached to exudate assessment can be reduced by using a tool such as the exudate continuum (Figure 1) (16). This is integral to the applied wound management approach described by Grey et al (16). This tool has the potential to assist in the accurate assessment of exudate and lend support in the decision-making process. It offers a method of generating a score relevant to volume and viscosity. For example, if a score of 4 is obtained using the exudate continuum (medium volume 3, and low viscosity 1) and this increases to 8 (high volume 5, and medium viscosity 3) over three days then the wound is likely to be deteriorating and may be infected. If the intervention chosen is appropriate, for example an absorbent antimicrobial dressing, then it is likely this will be reflected in a lower score after a few days. Figure 1: The wound exudate continuum (16). Chuck- this is being redrawn Footnote style Reproduced with permission from Gray D, et al. Understanding applied wound management. Wounds UK 2005 1(1): 62-8 (16). AWAITING PERMISSION Heading 1. Exudate management Several wound management tools have been developed that include a focus on exudate. One example is the wound bed preparation model (17) with the development of the acronym TIME, in which ‘M’ represents the need to maintain moisture balance (18). An exudate management strategy has been devised by Vowden and Vowden (2004) (19). This presents a strategy for assessing and evaluating the management of exudate. See Table 4. Table 4: An exudate management strategy (19). Cause Control Components Containment Correction Complications ●Systemic ●Whether ●Bacterial ●Dressing ●Modification ●Skin (local effective load seal of bacterial protection wound systemic ●Necrotic Where? load ●Protein loss related). or local tissue - at wound ●Debridement ●Pain control is ● ‘Chemical’ surface ●Exudate possible. composition - within modification. and pH dressing ●Viscosity - away from and volume. wound. ●Odour. Footnote style Reproduced with permission from Vowden K, Vowden P. The role of exudate in the healing process: understanding exudate management. In: White RJ, editor. Trends in Wound Care Volume III. London: Quay Books, 2004 (19). The selection of management options should be based on the characteristics of the wound and the needs of the patient. Successful management requires careful attention and continuous evaluation throughout the lifetime of a wound (14). For example, in the case of a leg ulcer, pressure ulcer or diabetic foot ulcer, exudate levels in the non-infected wound are generally higher in the early stages of healing and reduce as healing progresses. Dressing selection should therefore be tailored to the condition of the wound. This might necessitate the use of an absorbent moist dressing initially, changing to a moist dressing suitable for low exudate levels at a later stage. In wounds that become infected, exudate levels often increase and exudate can become viscous. The focus here should be on managing the underlying cause of infection. Cavity wounds and other wounds left to heal by secondary intention that are producing high levels of exudate may be suitable for treatment with topical negative pressure. One method is vacuum-assisted closure (VAC), which can be effective in removing viscous exudate (20) (21) (22). Heading 1 Methods used to manage exudate Heading 2 Dressings If dressings are indicated, then prudent selection and careful determination of wear time are imperative. This will help ensure an optimal moist environment is maintained, while protecting the surrounding skin from maceration (23) (24). Certain key performance characteristics are required for any such dressing: they must absorb and retain exudate, keep harmful chronic wound exudate away from the surrounding skin, perform efficiently when used under compression, be easy to remove and be demonstrated as cost-effective. Wound dressings exhibit various fluid-handling mechanisms: absorption, gelling, retention and moisture vapour transmission. Information on a dressing’s fluidhandling mechanism is available from the manufacturers. This information may not always be based on accepted, independent test methodologies, but rather on in-house laboratory data, which is invariably favourable to manufacturers’ own products. There are standard test methods, published as monographs in various pharmacopoeias and in peer-reviewed journals that provide independent, objective data on dressing fluid handling (25). The basic dressing mechanisms are as follows: Heading 3 Absorption Exudate is absorbed into the dressing matrix. In the case of some foam dressings, this is a reversible mechanism; the fluid can be expressed from the dressing under pressure. Not all foams behave in this fashion. Heading 3 Gelling Following absorption, the exudate interacts with the dressing material to form a gel (26). This is a typical attribute of alginates: these carbohydrate polymers gel according to the proportion of uronic acid units in their composition (27). However, with alginate gels, fluid may come into contact with the periwound skin (27). This can also occur with hydrocolloid gel, the degree being dependent on polymer composition (28). Heading 3 Fluid retention In dressings with this mechanism, fluid is absorbed by the dressing and is no longer available to wet the skin. Such materials retain the absorbed fluid directly above the wound, without sideways spread or ‘lateral wicking’. An example of this technology is the hydrofibre. Such dressings have been demonstrated to be clinically and cost-effective in exudate management, even when used under compression (29) (30). Heading 3 Moisture vapour transmission In recent years dressings have been designed to absorb fluid and, via an intermediate ‘wicking’ layer, move fluid away from the wound/skin interface towards a permeable backing layer. Here, some fluid is lost to the atmosphere by evaporation, a process known as moisture vapour transmission. This mechanism is intended to increase the fluid-handling capacity of the dressing (31) (32). The success of this process depends upon the proportion of absorbed fluid that is lost. Evaporation will be compromised by the presence of occluding materials, such as compression bandages, which may reduce evaporation rates. There are no clinical data to suggest that this works in practice. Indeed, some clinicians are sceptical that it has any performanceenhancing value (33). Heading 3 Antimicrobial properties Dressings with an antimicrobial component are intended for the control of the wound bioburden in critical colonisation and local infection (34). These dressings are useful, therefore, where raised exudate levels are attributed to bacterial causes. There is also justification for their use in cases of spreading infection where systemic antibiotics have been used and impaired perfusion is suspected (35) (36). Typical antimicrobial dressings are those containing silver, iodine or honey (12) (35) (37). Heading 2 Physical therapies Heading 3 Topical negative pressure therapy Suction drainage of wounds has been used for many years (38), and a variety of systems exist, including vacuum-assisted closure (VAC) therapy (39) (40) (41) (42). The VAC closed system is claimed to improve perfusion, reduce oedema and promote granulation tissue formation and is supported by evidence from many wound types, including trauma wounds, pressure ulcers, leg ulcers and surgical wounds (43) (44). The removal of exudate, particularly the more viscous forms, also removes bacteria and protease enzymes – both barriers to healing. This technique does, however, have disadvantages, and should not be used on wounds containing eschar or necrotic tissue. Heading 3 Compression In the healthy limb, the return of venous blood to the heart is achieved through the combined actions of the calf muscle pump and the foot pump, both of which require reasonable mobility and dorsiflexion of the ankle (45). Where venous ulceration occurs, the patient needs assistance in achieving venous blood return. Compression bandaging and intermittent pneumatic compression therapy have both been found to be effective (46) (47). Compression therapy has two main functions: to counteract venous hypertension and to control oedema (48). In achieving these functions, exudate is reduced in the non-infected venous leg ulcer (49) (50). In lymphoedema the application of appropriate compression bandages or garments will result in a reduction both of the limb oedema and of any exudate leakage (51) (52). Intermittent pneumatic compression therapy is administered through a bootshaped device which, by means of a pump, is inflated and deflated to achieve alternating, dynamic compression of the encased limb. IPC can be used as the main method of compression or as an adjunct to orthodox compression bandaging (53). Heading 3 Elevation/exercise In venous leg ulceration, the patient is advised to elevate the affected limb (with the ankle above the level of the heart) to achieve venous blood return. While this may not always be practical, some degree of elevation will aid venous return and, consequently, reduce exudate. In lymphoedema, manual drainage (54) and exercise (54) (55) are central to the control of oedema and leakage. Heading 1 Conclusion It is an unfortunate aspect of wound management that exudate is often regarded as an issue only when it becomes a clinical challenge - when leakage occurs or when peri-wound skin becomes macerated (56). However, such events are due to a combination of inaccurate assessment, inappropriate dressing selection, over-optimistic wear time or poor patient concordance. When dealing with purulent exudate, clinicians sometimes resort to using absorbent pads, taped in position and changed frequently. While dressings remain the mainstay of treatment, not all are suitable or effective for exudate management. Effective clinical management of exuding wounds depends on accurate assessment of the volume and viscosity of exudate, an understanding of relevant pathologies and the selection of an appropriate exudate management mechanism. This is all too often left to a dressing, without due consideration for other approaches. A focus on this aspect of wound care has the potential to reduce morbidity and costs, and is therefore justified. References Article 1. Vickery C. Exudate: what is it and what is its function? In: Cherry GW, Harding K, editors. Management of wound exudate: Abstracts from the first combined meeting of the European Tissue Repair Society and the European Wound Management Association at Green College, University of Oxford. ETRS Bulletin 1997. Article 2. Trengove NJ, Bielefeldt-Ohmann H, Stacey MC. Mitogenic activity and cytokine levels in non-healing and healing chronic leg ulcers. Wound Rep Regen 2000; 8(1): 13-25. Book 3. Haeger K. The Illustrated History of Surgery. London: Harold Starke, 1989. Book 4. Cutting KF. Exudate: composition and functions. In: White RJ, editor. Trends in Wound Care Volume III. London: Quay Books, 2004. Article 5. Trengove NJ, Langton SR, Stacey MC. Biochemical analysis of wound fluid from non-healing and healing chronic leg ulcers. Wound Rep Regen 1996; 4: 234-9. Pubmed 6. Baker EA, Leaper DJ. Proteinases, their inhibitors and cytokine profiles in acute wound fluid. Wound Repair Regen 2000; 8(5): 392-8. Article 7. Wilson JW, Schurr MJ, LeBlanc CL, Ramamurthy P, Buchanan KL, Nickerson CA. Mechanisms of bacterial pathogenicity. Postgrad Med J 2002; 78: 216-24. Pubmed 8. Gautam N, Olofsson AM, Herwald H, Iversen LF, Lundgren-Akerlund E, Hedqvist P, et al. Heparin-binding protein (HBP/CAP37): a missing link in neutrophil-evoked alteration of vascular permeability. Nat Med 2001; 7(10): 11237. Pubmed 9. Lundqvist K, Herwald H, Sonesson A, Schmidtchen A. Heparin binding protein is increased in chronic leg ulcer fluid and released from granulocytes by secreted products of Pseudomonas aeruginosa. Thromb Haemost 2004; 92(2): 281-7. Pubmed 10. Kim SH, An H, Field KG, Wei CL, Velazquez JB, Ben-Gigirey B, et al. Detection of Morganella morganii, a prolific histamine former, by the polymerase chain reaction assay with 16S rDNA targeted primers. J Food Prot 2003; 66(8): 1385-92. Pubmed 11. McDermott C, Mylotte JM. Morganella morganii: epidemiology of bacteraemic disease. Infect Control 1984; 5(3): 131-7. Article 12. Cooper RA, Morwood S, Burton N. Histamine production by bacteria isolated from wounds. J Infect 2004; 49: 39. Pubmed 13. Bates-Jensen BM. The Pressure Sore Status Tool a few thousand assessments later. Adv Wound Care 1997; 10(5): 65-73. Pubmed 14. Thomas S. Assessment and management of wound exudate. J Wound Care 1997; 6(7): 327-30. Pubmed 15 Mulder GD. Quantifying wound fluids for the clinician and researcher. Ostomy Wound Manage 1994; 40(8): 66-9. Article 16. Gray D, White R, Cooper P, Kingsley A. Understanding applied wound management. Wounds UK 2005; 1(1): 62-8. Pubmed 17. Sibbald RG, Williamson D, Orsted HL, Campbell K, Keast D, Krasner D, et al. Preparing the wound bed: debridement, bacterial balance, and moisture balance. Ostomy Wound Manage 2000; 46(11): 14-35. Book 18. Dowsett C, Ayello E. TIME: principles of chronic wound bed preparation and treatment. In: Cutting KF, editor. Trends in Wound Care Volume IV. London: Quay Books, 2005. Book 19. Vowden K, Vowden P. The role of exudate in the healing process: understanding exudate management. In: White RJ, editor. Trends in Wound Care Volume III. London: Quay Books, 2004. Pubmed 20. Armstrong DG, Lavery LA, Diabetic Foot Study Consortium. Negative pressure wound therapy after partial diabetic foot amputation: a multicentre, randomised controlled trial. Lancet 2005; 366(9498): 1704-10. Pubmed 21. Lambert KV, Hayes P, McCarthy M. Vacuum-assisted closure: a review of development and current applications. Eur J Vasc Endovasc Surg 2005; 29(3): 219-26. Pubmed 22. Venturi ML, Attinger CE, Mesbahi AN, Hess CL, Graw KS. Mechanisms and clinical applications of the vacuum-assisted closure (VAC) device: a review. Am J Clin Dermatol 2005; 6(3); 185-94. Pubmed 23. Bishop SM, Walker M, Rogers AA, Chen WY. Importance of moisture balance at the wound-dressing interface. J Wound Care 2003; 12(4): 125-8. Pubmed 24. Bolton LL, Monte K, Pirone LA. Moisture and healing: beyond the jargon. Ostomy Wound Manage 2000; 46(1A Suppl): 51S-62S. Erratum in Ostomy Wound Manage 2000; 46(3): 9. Pubmed 25. Thomas S, Fram P. The development of a novel technique for predicting the exudate handling properties of modern wound dressings. J Tissue Viability 2001; 11(4): 145-60. Pubmed 26. Thomas S, Hay NP. Fluid handling properties of hydrogel dressings. Ostomy Wound Manage 1995; 41(3): 54-9. Article 27. Thomas S. Observations on the fluid handling properties of alginate dressings. Pharm J 1992; 248: 850-1. Article 28. Thomas S, Loveless P. A comparative study of the properties of six hydrocolloid dressings. Pharm J 1991; 247: 672-5. Pubmed 29. Armstrong SH, Ruckley CV. Use of a fibrous dressing in exuding leg ulcers. J Wound Care 1997; 6(7): 322-4. Pubmed 30. Guest JF, Ruiz FJ, Mihai A, Lehman A. Cost effectiveness of using carboxymethylcellulose dressing compared with gauze in the management of exuding leg ulcers in Germany and the USA. Curr Med Res Opin 2005; 21(1): 81-92. Pubmed 31. Erasmus ME, Jonkman MF. Water vapour permeance: a meaningful measure for water vapour permeability of wound coverings. Burns 1989; 15(6): 371-5. Pubmed 32. Palamand S, Reed AM, Weimann LJ. Testing intelligent wound dressings. J Biomater Appl 1992; 6(3): 198-215. Article 33. Vowden K. Wound management: The considerations involved in dressing selection. Nurs Prescr 2004; 2(4): 152-61. Pubmed 34. Kingsley A. The wound infection continuum and its application to clinical practice. Ostomy Wound Manage 2003; 49(7A Suppl): 1-7. Article 35. White RJ, Cooper RA, Kingsley A (2001). Wound infection and microbiology: the role of topical antimicrobials. Br J Nurs 10(9); 563-78. Pubmed 36. Frank C, Bayoumi I, Westendorp C. Approach to infected skin ulcers. Can Fam Physician 2005; 51: 1352-9. Article 37. White RJ, Cutting KF, Cooper RA, Kingsley AR. The use of topical antimicrobials to control wound bioburden. Ostomy Wound Manage 2006; in press. Pubmed 38. Maitland AI, Mathieson AJ. Suction drainage: a study in wound healing. Br J Surg 1970; 57(3): 193-7. Pubmed 39. Edlich RF, Haines PC, Pearce RS, Thacker JG, Rodeheaver G. Evaluation of a new, improved surgical drainage system. Am J Surg 1985; 149(2): 295-8. Pubmed 40. Smith SR, Gilmore OJ. Surgical drainage. Br J Hosp Med 1985; 33(6): 30815. Pubmed 41. Ritter MA, Fechtman RW. Closed wound drainage systems: the Stryker Constavac versus the Snyder Hemovac. Orthop Rev 1988; 17(5): 496-8. Pubmed 42. Zerbe M, McArdle A, Goldrick B. Exposure risks to the management of three wound drainage systems. Am J Infect Control 1996; 24(5): 346-52. Pubmed 43. Banwell PE, Teot L. Topical negative pressure (TNP): the evolution of a novel wound therapy. J Wound Care 2003; 12(1): 22-8. Article 44. Moore K. VAC therapy: interactions in the healing process. Wounds UK 2005; 1(1): 86-90. Article 45. Vowden K, Vowden P. Anatomy, physiology and venous ulceration. J Wound Care 1988; 7(7 Suppl): S1-S7. Pubmed 46. Douglas WS, Simpson N. Guidelines for the management of chronic venous leg ulceration. Report of a multidisciplinary workshop. British Association of Dermatologists and the Research Unit of the Royal College of Physicians. Br J Dermatol 1995; 132(3): 446-52. Article 47. NHS Centre for Review and Dissemination, University of York. Compression therapy for venous leg ulcers. Effective Healthcare 1997; 3(4): 1-12. Pubmed 48. Felty CL, Rooke TW. Compression therapy for chronic venous insufficiency. Semin Vasc Surg 2005; 18(1): 36-40. Pubmed 49. Burton CS. Venous ulcers. Am J Surg 1994; 167(1A): 37S-40S. Pubmed 50. Brem H, Kirsner RS, Falanga V. Protocol for the successful treatment of venous ulcers. Am J Surg 2004; 188(1A Suppl): S1-S8. Pubmed 51. O’Brien JG, Chennubhotla SA, Chennubhotla RV. Treatment of edema. Am Fam Physician 2005; 71(11): 2111-17. Pubmed 52. Cheville AL, McGarvey CL, Petrek JA, Russo SA, Taylor ME, Thiadens SR. Lymphedema management. Semin Radiat Oncol 2003; 13(3): 290-301. Pubmed 53. Vowden K. The use of intermittent pneumatic compression in venous ulceration. Br J Nurs 2001; 10(8); 491-509. Pubmed 54. Szuba A. Literature watch. The addition of manual drainage to compression therapy for breast cancer related lymphoedema: a randomized controlled trial. Lymphat Res Biol 2005; 3(1): 36-41. Pubmed 55. Badger C, Preston N, Seers K, Mortimer P. Physical therapies for reducing and controlling lymphoedema of the limbs. Cochrane Database Syst Rev 2004; 18(4): CD003141. Pubmed 56. Cutting KF, White RJ. Avoidance and management of peri-wound maceration of the skin. Professional Nurse 2002; 18(1): 33-6.