Risk Assessment Haz Vul Template Guideline
advertisement

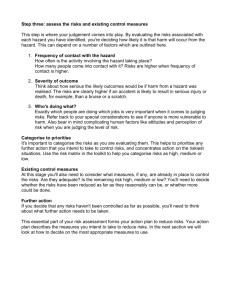
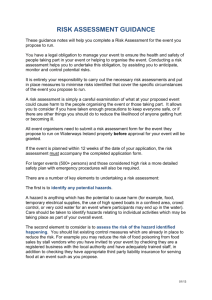
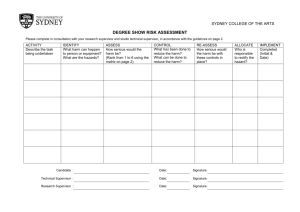
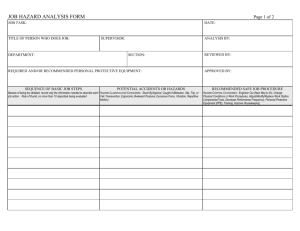
Infection Prevention and Control Risk and Hazard Vulnerability Assessment template guideline GUIDELINES FOR USE OF THE RISK ASSESSMENT PRIORITIZATION TOOL 1) PURPOSE The purpose of this tool is to enable committees and work groups to focus resources on the most compelling health care delivery issues, specifically, to understand the degree of threat posed by a hazard. With limited time and resources, groups may choose to use this tool to prioritize the most important work. The design of this tool is to stratify the risk potential of health care hazards for the organization. This tool enables users to develop an escalated response to health care delivery concerns in order to improve patient and/or organizational safety. The tool should be utilized with objective and subjective data as well as the judgment of a multidisciplinary team and leaders. The tool assesses and combines the impact of a particular scenario on two targets (the patient and the organization). As a guiding safety principle, risk to the patient should always prevail over risk to the organization. Risks identified via use of this tool do no preclude identification of other priorities or goals. 2) DEFINITIONS Risk: an expression of the degree of threat posed by a hazard. Clinical or healthcare risk is the chance of an adverse outcome resulting from clinical investigation, treatment or patient care. Risk is the combination of the probability (likelihood) and severity (consequence) of a hazard being realized. Hazard: an activity or condition posing threat of harm to a patient, healthcare worker, healthcare equipment or schedule (down-time, delay). Our primary target of concern in healthcare is the patient (e.g. TB Exposure). Event: something that takes place or happens; an occurrence; an adverse or damaging medical occurrence (e.g. Earthquake). Probability: the likelihood the hazard will occur. Likelihood of harm is defined as the probability of the failure occurring during an exposure interval. Severity: An estimation of the worst experienced harm that can reasonably result from the event, process failure or hazard, i.e. how serious the effects or harm would be, given a reasonable worst case. Exposure Interval: The exposure interval is the period of time an event/issue/hazard poses threat of harm. In health care, this is usually the time associated with a procedure, care episode, or admission. Judgment and experience will serve as the best guide for determining the length of exposure interval. One year is the recommended period of time to consider as an exposure interval. Risk Reduction Strategy: Countermeasure / action taken to reduce risk 3) EXPECTED USER GROUPS This tool is intended for use by facility committees, teams or workgroups. The results of the Risk Assessment, goals and action plans to address risks should be reported to facility leadership and the Medical Executive Committee. 2/16/2016 1 Infection Prevention and Control Risk and Hazard Vulnerability Assessment template guideline 4) WHEN TO USE THIS TOOL a) The tool should be used at the beginning of a work cycle (e.g. yearly) in order to develop the goals and workplan for the cycle. b) The tool should also be employed at any time during the cycle when circumstances change or significant changes occur, e.g. internally (new services, branch offices, programs or populations served) and as a response to external events. Revise the risk assessment when new risks are identified and there may be a need to reprioritize. c) Consider review of the risk assessment periodically. Determine whether things change quickly in the organization and identify the frequency of review. 5) STEPS a) Identify the Hazards (What Can Go Wrong): At the beginning of a work cycle, define the list of specific hazards from any or all of your data sources: unusual occurrences, potentially compensable events, significant/sentinel events, root cause analysis, medical legal claims, member complaints, regulatory complaints, internal data, audits and surveys, regulatory complaints, regulatory or professional organization “alerts”, legislative imperatives, review of the literature and community standards of care/practice. If using a function specific template with hazards previously identified, determine if there is a need to add facility specific hazards that are unique to the organization and community. i) Define your hazard as a Source, Mechanism or Outcome of harm, wherever possible. (1) (2) Source is defined as the origin from which the harm is derived. Mechanism is the means by which the harm is produced by the hazard. (3) Outcome is the harm itself, the result or consequences [e.g. the misidentification (source) of blood products leading to administration errors (mechanism) resulting in a blood reaction (outcome). (4) Place the description of the source, mechanism or outcome of harm in the “Hazard” column. ii) Hazards may have sub-categories or risk factors within the category that require consideration and scoring of risk individually. iii) Determine the length of the exposure interval. One year is recommended. b) Assess Hazard Risks i) Risk Criteria Scoring (1) Probability of Harm: An estimation of the likelihood of a harm event occurring during the exposure interval. (2) Severity of Harm: Determine the worst experienced harm that can reasonably result from the event, process failure or hazard during the exposure interval. 2/16/2016 2 Infection Prevention and Control Risk and Hazard Vulnerability Assessment template guideline (3) Assign a risk score or rating that most correctly describes the listed risk criteria and place the score in the column below the criteria. (4) Multiply the individual scores and place in the column entitled “Score”. This will automatically be calculated when using the excel Risk Assessment Tool template. If you have added hazards to the tool by adding rows, be sure to add the formulas to the tool in order to calculate your ratings in the “Score” column. c) Determine the Risk Priorities: (1) Determine a cut off/threshold priority score or numeric range for high priority, moderate priority and low priority. Look for natural groupings of numbers. The highest risks will require implementation of risk reduction strategies. This is a subjective determination by the multidisciplinary team. Consider the organization’s existing preparedness related to the hazard when determining priorities. The team may review a risk that was scored “High” and determine that this is a lower risk due to the activities already undertaken to address this hazard. This decision should be documented in meeting minutes. (2) Rank the events with a priority number in the column titled “Priority”; the highest total scores are the #1 priority. If two events have the same total score, place the event with the highest patient risk subtotal score as the highest priority for that score. Rank #2 and #3 priorities, those that are determined to be moderate and low risk. (3) Use of a histogram or bar graph may be of assistance in determining the highest priorities for focusing risk reduction activities. Be realistic; identify the top 2-4 risks in a specific area as highest priorities in order to focus risk reduction activities. Include moderate risks in goals if it is determined that action is required to decrease risk. RISK SCORING DESCRIPTIONS RISK SCORE RISK TO PATIENTS Probability of Hazard (How likely is the harm/event) 5 4 3 Frequent; Probable: Quite Occasional: Occurrence likely to occur in May occur in almost certain in exposure exposure exposure interval interval interval 2 1 Rare: Not likely Improbable or to occur but Impossible: So possible in unlikely it can exposure not be interval assumed, Occurrence may not be experienced 2/16/2016 3 Infection Prevention and Control Risk and Hazard Vulnerability Assessment template guideline Severity of Hazard (If event does occur, what is the worst credible consequence of the harm/event) Catastrophic, Life Threatening, Death Major Impact to Health & Safety; Critical, severe or severely exacerbated injury or illness or significantly reduced life expectancy Moderate Minor Impact to No harm; no Impact to Health & impact Health & Safety; Trivially Safety or mildly exacerbated exacerbated injury or illness; injury or illness; may require temporary first aid harm 2/16/2016 4