General AnesthesiaChp - for merge
advertisement
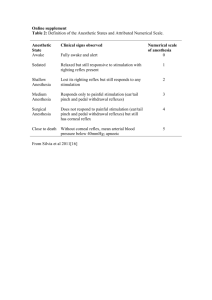
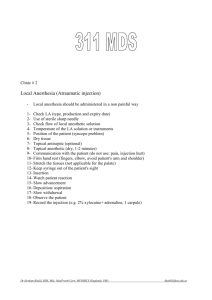
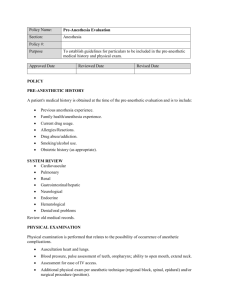
General Anesthesia Chp. 2, VAAA Chp. 5&8 in SASN Definition of General Anesthesia: ! Adrug induced unconsciousness@ ! a state of controlled & reversible unconsciousness ! achieved via injectable or inhaled drugs 1)Injectables Ex.) Thiopental, methohexital, pentobarbital, cyclo-hexamines (ketamine & telazol), propofol, Neuroleptanalgesics (tranquilizer & opioid) Neuroleptanalgesics: -a tranquilizer and an opioid combination for procedures that require significant CNS depression and analgesia, however can induce anesthesia in very sick patients (given IV slowly) Ex) acepromazine, medetomidine (Domitor), diazepam with morphine, meperidine, oxymorphone, butorphanol 2) Inhalants Ex.) Halothane, isoflurane, sevoflurane, desflurane, nitrous oxide ! Characterized by the absence of: 1) pain 2) memory 3) motor response 4) reflexes ! Achieved via techniques and agents chosen by the vet aka Aanesthetic protocol@ Four Components of General Anesthesia: 1)Pre-anesthesia $ $ $ $ Time immediately preceding anesthesia Minimum data base (PE, Dx tests, Patient History) Patient status (hydrated, fasted, etc.) Anesthetic protocol ( drugs to be used) 2) Induction $ $ $ Animal leaves state of consciousness, becomes unconcious After premeds given -10 mins after IM route -20 min after SQ route Phases: 1) Incoordination or excitment 2) Progressive relaxation 3) Unconciousness $ Ideally the excitement and struggling should be avoided during induction -unpleasant for patient -predisposes animal to cardiac arrhythmia, perivascular inj $ Loss of protective reflexes, ability to swallow/cough 3) Maintenance $ $ $ $ $ $ $ $ $ sufficient anesthetic is supplied to keep the patient at an appropriate depth of anesthesia surgical procedures done at this time onset of analgesia skeletal muscle relaxation cessation of movement further loss of protective reflexes -palpebral reflex(eye blink) occurrence of mild respiratory and cardiovascular depression CLOSE MONITORING ESSENTIAL THROUGHOUT THIS PERIOD 4) Recovery $ begins when the concentration of anesthetic agent in the CNS begins to decrease -reversal of induction $ Elimination: 1) Most injectable medications >liver metabolism and renal excretion >exceptions, some go directly to kidneys Ex.) Ketamine in cats 2) Inhalant Agents >mostly eliminated through respiratory system (lungs) >some liver metabolism 3) Short-acting thiobarbituates >drug is rapidly redistributed to other tissues -especially muscle and fat >results in lower levels of the drug in the brain **recovery from inhalant/inj can be speed up by analeptic agents -ex) doxapram and other specific reversing agents Safety of General Anesthesia **NEVER W/OUT RISK!!!!!** $ Every anesthesia patient is at risk for complications such as: >Hypotension (decreased blood pressure) >Hypoventilation (decreased resp rate/tidal volume) >Hypoxia (decreased availability of oxygen to the tissues >Hypothermia (low body temperature) Monitoring by a trained individual is the single most important factor in preventing serious anesthetic problems >Monitoring heart rate, pulse quality, ventilation, mucous membrane color, and perfusion (CRT) Precautionary Steps: 1) Minimum patient data base -patient history -PE -anesthetic protocol -Dx tests 2) Patient Status -corrected problems before anesthesia ex) dehydration, hypotension, anemia 3) Pre- anesthetics given to prevent cardiac abnormalities (bradycardia, arrthymias) -atropine -ace 4) Pre-anesthetic sedatives help reduce the dose of general anesthetic required to induce and maintain anesthesia, minimizes adverse effects of general anesthetic agent ex) ace, alpha-2-agonists, and opioids 5)double check doses 6) administer only the minimum dose of drug needed to achieve the desired level of anesthesia >AGive to effect@ >dose needed affected by age, breed, physical condition, liver & kidney fnx 7) Endotracheal intubation >efficiently administers oxygen >protects airway from aspiration/obstruction 8)CLOSE PATIENT MONITORING! Classical Stages and Planes of Anesthesia $ Animals pass through series of anesthetic stages and planes $ Animals show a progressive loss of: -pain perception -motor coordination -consciousness -reflex responses -muscle tone -cardiopulmonary function *Stages and planes are not well defined in every animal. *The technician monitoring anesthesia of the patient must evaluate as many variables and indicators as possible to determine the patient=s depth of anesthesia *The technician must ensure that the patient does not feel surgical pain but must avoid excessive anesthetic depth Stage I -immediately after the administration of an inhalant or injectable agent -animal is conscious but disoriented, shows reduced sensitivity to pain -all reflexes are intact, animal is still awake, may struggle, urinate and/or defecate, anxiety -resp & heart rate normal/increased -IDEALLY SHORT, dangerous time (never trust the animal) Stage II -loss of consciousness BUT involuntary excitement -all reflexes intact (exaggerated) ex.) Yawning, pupils dilated -actions not under conscious control -unpleasant for animal/staff ex) struggling animal may injure itself/staff -Aexcitement phase@ involuntary ex.) Rapid movement of limbs, vocalization, and struggling -breathing may be irregular (may appear to be holding their breath -potentially hazardous for animal via release of epinephrine (cardiac arrhythmias/arrest) -ends when patient shows signs of muscle relaxation, decreased reflex activity, & slower respirations -IDEALLY SHORT! Stage III -subdivided into FOUR planes Plane 1 AIntubation phase@ -Alight@ -patient will not tolerate surgery -respiratory pattern becomes regular -involuntary movements cease -eyeballs start to rotate ventrally -pupils partially constricted -gagging/swallowing reflexes depressed but can pass an ET -sill have palpebral reflex -other reflexes present but depressed Plane 2: Asurgical phase:@ -Amedium@ -suitable for most surgery -unconscious/immobile -respirations regular but shallow (12-16) -normal protective reflexes are diminished/lost entirely -eyes : sluggish papillary light response, eyeballs central/rotated ventrally, pupils slightly dilated Plane 3: -Adeep@ -animal appears deeply anesthetized -significant depression of resp/cardiovascular fnx -resp rate less than 12 bpm -shallow respirations -heart rate reduced, pulse strength reduced -CRT increased (slower) -eyes: poor pupillary light reflex, eyeballs central, pupils dilated -weak/absent reflexes -marked skeletal muscle relaxation Plane 4: Atoo damn deep@ -respiratory effort is primarily abdominal muscular in nature -resp rate less than 8 bpm -eyes: fully dilated pupils, no papillary light response, dry eyes -no muscle tone -dramatic drops in heart rates and blood pressure -pale mucous membranes, prolonged CRT -nearing death Stage IV -don=t go there -complete cessation of respiration -circulatory collapse -DEATH INDUCTION TECHNIQUES AND AGENTS -Injectable Anesthetics Agents 1) IV -one of the most common induction techniques -ex) thiopental, ketamine, propofol -standard dose calculated & drawn into syringe -injected as needed directly into vein ATO EFFECT@ to Stage III, plane 1 -quick to bypass Stages I &II to place ET -endotracheal intubation -single bolus or constant infusion Ato effect@ 2) IM -ketamine/telazol -ferrets/ young pups/kits -useful for animals that can=t be handled easily -usually requires a larger dose (slower, takes longer to absorb in muscle) -cannot be given to effect -slower induction -lengthy recovery time 3)Oral -an extra label use -not used routinely -beware of producing aspiration -avoid contact with eyes -Inhalation Agents -need to used rapid acting inhalant agents (isoflurane, sevoflurane, halothane) 1) Mask -may be more suitable for critical patients -Cautions: -anesthetic gas pollution of room -risk of stressing patient -may be dangerous w/animals with poor respiratory fnx -Preventions: -use tight fitting mask -use preanesthetic sedation 2) Anesthetic Chamber -uses sturdy , see through container -Cautions: -small patients ONLY! -difficult to monitor patient -risk of vomiting/regurgitationk -waste gas contamination of room, exposure of personnel -option for factitious cats INTUBATION: (Stage III, plane 1) 1) Postition -sternal, extend neck, tongue out 2) Visualize -soft palette may be in the way -epiglottis -arytenoid cartilage 3) Place -timing -use a stylet for small dogs and cats to place tube -lidocane for cats 4) Confirm -cough, watch breathing bag, condensation on tube, Ahair test@, bag & observe 5) Secure -with gauze Advantages of ET: -more efficient delivery of anesthetic gas, - reduces exposure of personnel to waste anesthetic gas -more economical -reduces the amount of anatomic dead space w/in respiratory passages >Anatomic dead space describes those portions of the breathing passages that contain air but which no gas exchange can occur -larger proportion of gas delivered to patient reaches the exchange surface in the alveoli -allows direct delivery of oxygen to patient when assisted respiration is needed >aka open airway >IPPV (Intermittent positive pressure ventilation) -inflated cuff reduces risk of aspiration of vomitus, blood, saliva, other material Ex. During dentals Disadvantages: -may stimulate vagus nerve & cause increase in parasympathetic tone (dogs) >resulting in bradycardia, hypotention, cardiac arrhythmias -can reverse with atropine -Brachycephalic dogs have a large amt of tissue w/in oral cavity, tissue falls over back of pharynx when mouth is open, making it difficult to intubate -Overzealous effort to intubate may damage larynx, pharynx, or soft palate **particular care while intubating cats! -laryngospasm -prevent via placement of lidocane to help desensitize the laryngeal tissue -If too long of a tube used >increases amt of mechanical dead space (space in breathing system occupied by gases that are breathed in/out w/out any change in composition > may be inserted too far into breathing passages so that it enters a bronchus Maintenance of Anesthesia (Stage III, plane 2-3) Two important tasks: 1) Monitor patient closely to ensure the vital signs remain w/in normal ranges 2) Maintain patient at an appropriate level of anesthesia so no pain is felt THE KEY TO EFFECTIVE AND SAFE ANESTHESIA IS PATIENT MONITORING!!! A) Monitoring Vital Signs vital signs = those variables that indicate responses of an animal=s homeostatic mechanisms to anesthesia ***Rely on you own senses first and foremost, then confirm with electronic devices*** 1) Heart rate & rhythm -normal minimal heart rates : 1) dog = 60 bpm 2) cat = 100 bpm Lower heart rates may indicate excessive anesthetic depth -result of a depresant effect of anesthetic on heart rate & myocardial fnx -Cardiac rhythm can also be affected by anesthetic agents >especially halothane & xylazine -Cardiac monitoring via: 1)Direct palpation -chest, lingual artery, pedal artery, femoral artery 2) Auscultation -stethoscope, esophageal stethoscope 3)Cardiac monitor -When heart rate drops, check gas, drugs may be wearing off (atropine), depth of anesthesia effects heart rate **NOTE: the presence of a beating heart doesn=t necessarily imply adequate circulation ex) low blood pressure = pounding heart, not good circulation 2) Capillary Refill Time (< l sec or < 2sec) -reflects perfusion of tissue with blood but not infallible -prolonged CRT indicates that tissues have reduced blood supply >Due to: 1) vasoconstriction 2) low blood pressure (acepromazine) 3) shock 4) excessive anesthesia (stage III, plane 4) 3) Mucous Membrane Color -at gingival, conjunctiva, tongue, vulva, or prepuce -should be pink -pale mm color = blood loss anemia or poor perfusion -brick red color = acidosis (buildup of CO2, due to used up Co2 absorber) -bluish discoloration = Acyanosis@ (stagnant blood flow or lack of oxygen) -yellow = jaundice (hyperbilirubinemia) 4) Pulse Strength -subjective, palpate a major artery -reflects adequacy of blood circulation throughout body -causes of hypotension (low Bp, weak, thready pulse) 5)Blood Loss -estimated by counting 3 x3 gauze sponges *5 ml per gauze pad** -if excessive, predisposes animal to shock 5) Respiration rate & depth - monitor by observing animal=s chest or reservoir bag -monitor: 1) resp rate 2) depth of respiration (tidal volume) -tidal volume decreases by 25% due to anesthesia/preanesthetic drugs decrease the expansion of the intercostal muscles on inspiration 3) Character -at moderate depth of anesthesia normal rate is 8-12 or 8-20 bpm - < 6 should be using IPPV (intermittent positive pressure ventilation) -If alveoli in lungs don=t receive amounts of air adequate for normal gas exchange, they may partially collapse = atelectasis (partial collapse of alveoli) >reversed via Abagging@ or Asigh) animal every 5 minutes -hyperventilation (increase in depth) and tachypnea (increased resp rate) 1)due to build up of CO2 in blood or metabolic acidosis ( CO2 not being adequately removed by CO2 absorber) 2) disease 3) pain 4) Upper respiratory infection (increase resp rate, shorter more shallower breaths) -anesthetized animal=s breathing should be smooth and regular -thoracic and diaphragmatic 7)Thermoregulation -hypothermia = most common anesthetic complication -most temp loss occurs w/in first 15 min of anesthesia -contributing causes: 1) Surgery prep (shaved, skin washed w/ antiseptic, & alcohol solutions that cool by evaporation. 2) anesthetized animals can=t generate heat by shivering/ muscle activity 3) metabolic rate is decreased so less heat generation 4) during surgery a body cavity may be opened and viscera exposed to room air temp 5) several preanesthetics and general anesthetics cause vasodilation 6) pediatric/geriatric animals less able to maintain thermoregulation prevention: 1) check temp every 5 min 2) warm IV fluids 3) circulating hot water blanket/hot water bottles 4) Bair hugger B. USE OF INSTRUMENTS TO MONITOR VITAL SIGNS 1) blood pressure -#1 side affect of anesthesia -different types 1) Systolic pressure -produced by contraction of the ventricles and propels blood through the aorta and major arteries -highest pressure that is exerted throughtout the cardiac cycle 2) Diastolic pressure -the pressure that remains when the heart is in its resting phase, between contractions. -lowest pressure that is exerted throughout the cardiac cycle -Mean arterial pressure - average pressure through the cardiac cycle -most important pressure -best indicator of blood perfusion of the internal organs Pulse pressure -pressure detected by manual palpation, difference between systolic pressure and diastolic pressurek -a mean blood pressure of 60 or more is ideal -normal systolic pressure in a dog/cat = 120 mm Hg (90-160) -normal diastolic pressure is 80 mm Hg (50-90) -normal MAP is 90-100 mm Hg -blood pressure not the same as blood flow -high systolic pressure indicates constricted blood vessels 2) Doppler Blood Pressure monitors -manual cuff, inflate/deflate -uses sound -emits a series of high freq sound waves 3) Oscillometer blood pressure monitors -measures blood pressure -cuff/detector unit connected to a pc -work automatically, don=t require an attendant to inflate/deflate the cuff -allows determination of diastolic pressure and MAP. 4) CVP (Central Venous Pressure) -helps to assess how well blood is returning to the heart & ability of the heart to receive and pump blood -preventing over hydration with IV fluids CVP increases a blood volume increases) - measured via inserting a long catheter in the jugular to anterior vena cava 5) Blood Gases a) Oxygen -free molecule in plasma (PaO2) -measured with a Blood Gas Analyzer -bound on hemoglobin (SaO2) -measured with a Pulse Oximeter -both indicate the degree of oxygenation of a patient (how well the lungs deliver oxygen to the blood) -Normal PaO2 is 90-115 mm Hg -Anesthetized animals show a greatly elevated PaO2 because they are breathing almost 100% oxygen -SaO2 readings are usually high due to breathing pure O2 -Low PaO2 and SaO2 values indicate hypoxia and need for O2 supplementation/ventilation b) Carbon Dioxide -PaCO2 (Blood Gas Analyzer) -is often elevated during anesthesia due to resp depression caused by anesthetic that causes the body to retain CO2 *Pulse oximeters and blood gas analyzers allow early recognition of situations in which the patient is poorly oxygenated 6) Capnography -monitoring the amount of CO2 in the air that is breathed in and out by the patient -noninvasive, continuous, and practical -during inspiration, CO2 = zero unless some rebreathing taking place/CO2 absorber not working properly -during expiration, CO2 content increases (end tidal) -CO2 levels then fall as expiration ends and inspiration begins 7) Electrocardiography -monitors heart rate and rhythm on a continuous or intermittent basis -Tachycardia -heart rates greater than 200 bpm in cat , 180 bpm in small dog, and 160 bpm in large dog -may be result of ketamine, atropine, epinephrine - Bradycardia -heart rates less than 60 bpm, in large dog, 70 bpm in small dog, and 100 bpm in cat -may be result of xylazine, domitor, or opioids -Normal rhythm (P, QRS, T) A) P-wave = atrial depolarization and atrial contraction B) QRS complex = depolarization of ventricles, ventricular contraction (systolic) C) T- wave = ventricles repolarization (diastolic) -Normal P, QRS, T wave - Tachycardia -increased ventricular rate A) > 200 in cat B) >170 in dog Bradycardia A) <100 in cats B) <60 in dog -Normal ECG ECG abnormalities: 1) Heartblock -electrical impulse that causes the heart to beat is not being transmitted efficiently throughout the heart -first, second, and third degree heart blocks -commonly seen after administration of alpha-2 agonists Ex) medetomidine (Domitor) -other causes: -high vagal tone -hyperkalemia -cardiac disease >first degree heart block - P-wave for every QRS complex & QRS for every P-wave 2) Premature ventricular contractions (PVC=s) -an impulse that arises from a focus in the ventricular muscle and represents an ineffective and uncoordinated contraction -appear as bizarre, wide QRS complexes -QRS without P-wave -commonly seen in anesthetized animals -especially those induced w/ barbituates -halothane -hypoxia common -cardiac dz, gastric torsion, trauma to the heart, acid-base or electrolyte disorders -epinephrine is a potent stimulus of PCV=s -administered -result of fear, pain, excitement 3) Fibrillation-contraction of small muscle bundles w/in the ventricles or atria -ventricular fibrillation (v-fib) -atrial fibrillation -ventricular fibrillation indicates that cardiac arrest is imminent -absence of recognizable QRS complexes -Atrial fibrillation -Ventricular fibrillation 4) Respiratory arrhythmia -heart rate affected by breathing -normal Reflexes and Other Indicators of Anesthetic Depth Reflex = an involuntary response to a stimulus 1) Reflex activity -diminishes w/ deeper anesthesia 2) Palpebral reflex -blink, lost with deeper anesthesia 3) Swallowing reflex -indicator to pull e-tube -lack of indicates 4) Pedal reflex -squeeze digit 5) Ear flick reflex -tickle inner ear 6) Corneal reflex -corneal contact (blink/retract) 7) Laryngeal reflex -closes epiglottis 8) Muscle tone -jaw tone 9)Eye position and pupil size -I central, II ventral (surgery), III central 10) Salivary and lacrimal secretions -why need ET tube 11) Heart and respiratory rates -CRT 12) Response to surgical stimulation -pain response -increase heart rate, increase resp rate D.) Judging Anesthetic Depth -monitor as many variables as possible -consider all the info -each animal is unique and has an individual response to increasing anesthetic depth E.)Recording Information during Anesthesia -medical records (drug log) -controlled substance log -patient=s record F. Patient Positioning and Comfort During Anesthesia -during induction should be supported as it losses consciousness (avoid allowing patient to smack their heads on table -disconnect ET when flipping over, moving patient -correct placement of ET -hoses of the anesthetic machine should be supported to that there is no drag on tube -when positioning on table make sure animal assumes as normal a posture as possible -when restraining animal with ropes/gauze, they should not be too tight as to cut off blood circulation or overextension -do not compromise the chest of small patients with heavy drapes/instruments -be cautious when tilting the surgery table -eye lubricant (anesthesia decreases tear secretion) Recovery from General Anesthesia Recovery period = period between maintenance levels of anesthesia and consciousness Factors affecting length of recovery period: 1) length of anesthesia -direct relationship 2) condition of the patient -disease 3) type of anesthetic given and route of administration -IV, SQ, IM, Inj, Inhalant 4) patient=s temp -inverse relationship 5) breed of patient -sight hounds and barbituates Stages of Recovery -progress back through the same anesthetic stages that occurred during induction Monitoring -recovery should take place in an area where animal can be monitored closely -emergency kit -oxygen -monitoring equipment -check vital signs every 5 minutes -MM color -CRT -Respiratory effort -check temp every 15 minutes until >98 F -before 98 can=t shiver Administration of Oxygen -for several minutes after discontinuation of anesthetic -keeps patient oxygenated -eliminated waste gases through scavenger system -allows periodic bagging -re-inflates collapsed alveoli -prolonged intake of high levels of oxygen can be toxic Extubation -remove when shallowing reflex returns -exception: -brachycephalic breeds (delay extubation until they can lift their head) -remove the ET tube at the end of inspiration -if blood or fluid had accumulated in oral cavity, leave cuff of tube partially inflated as tube is removed -prevents fluids from flowing down trachea Stimulation Of the Patient -may hasten recovery by gentle stimulation -reticular activating center -rubbing face, head, and neck -moving limbs -turn patient over every 10-15 minutes -avoids collapsing of lungs Reassuring the Patient -quiet, calm, gentle handling -minimize patient discomfort -blankets, padding, pain meds Postoperative Analgesia -Give BEFORE animal experiences post-op pain Nursing Care -application of supplemental heat if patient is hypothermic -warm towels, hot water bottles, circulating warm water pads -NEVER electric heating pads!!!!! Preventing Patient Self-Injury -some patients will go through a period of excitement A a stormy recovery@ -tranquilization and/or use of analgesic meds -never left alone on a table or in a cage with the door left open