Implementing the new medical oncology model

Medical Oncology
National
Implementation
Plan
2012/13
Citation: Ministry of Health. 2012. Medical Oncology National Implementation Plan
2012/13. Wellington: Ministry of Health.
Published in August 2012 by the
Ministry of Health
PO Box 5013, Wellington 6145, New Zealand
ISBN 978-0-478-39356-9 (online)
HP 5522
This document is available at www.health.govt.nz
Contents
Executive Summary
1 Overview
1.1
Purpose of the implementation plan
1.2
Implementation plan governance
1.3
Reducing inequalities
2 The need for medical oncology service improvement
3 Implementation plan framework
3.1
The implementation programmes
4 The 12-month implementation plan
4.1
Service configuration programme: develop a national four-level service centre model
4.2
Workforce programme: develop sustainable workforce models and education pathways
4.3
Service quality programme: tumour standards, guidance and protocols
5 National roll-out
6 DHB implementation priorities for 2012/13
7 Communications and stakeholder consultation
Reference
Appendices
Appendix One: Groups and governance in the national cancer programme
Appendix Two: Description of proposed four-level service centre framework
Appendix Three: Summary of local models of care
Appendix Four: Key pathway points and components v
2
4
4
8
9
11
14
15
17
18
19
20
23
23
24
1
1
1
1
Medical Oncology National Implementation Plan 2012/13 iii
List of Tables
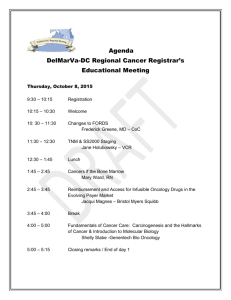
Table 1: Activities to address recommendations in the MOMOC report, over the
12 months of 2012/13
Table 3.1: Overview of the three recommended implementation programmes
Table 5.1: Roll-out activities by fiscal quarter year, 2012/13–2013/14
Table A1: Roles and linkages of groups involved in the National Cancer Programme
List of Figures
Figure 2.1: Provision of chemotherapy by fiscal year, 2008/09–2010/11
Figure 2.2: Projected number of patients starting chemotherapy, by regional cancer centre, 2010–2026
Figure A1: Governance structure of the National Cancer Programme vii
4
15
20
2
3
20 iv Medical Oncology National Implementation Plan 2012/13
Executive Summary
Important guiding principles
This implementation plan signifies the start of a process for increasing capacity and improving the delivery of medical oncology services in New Zealand. The plan outlines activities that can be undertaken in the 2012/13 fiscal year within current resource and fiscal constraints. While the majority of the activities in this plan are nationally led, district health boards (DHBs) are expected to work with the Ministry of Health to implement these activities at regional and local levels.
The plan will be updated annually. The Cancer Programme Steering Group will monitor its implementation.
The principles guiding this implementation plan are to:
maintain high quality of care and improve the quality of life for people with cancer
effectively, equitably and sustainably meet the future demand for medical oncology services, given the significant workforce and resource constraints that exist ensure fiscal responsibility.
Fiscal implications
The estimated costs for implementing the activities in the implementation plan will be met from Ministry of Health baseline funding.
New funding identified through Budget 2012 will support national and regional infrastructure, frameworks and processes to assist in implementing the new model of care on an ongoing basis.
A medical oncology system under pressure
Cancer is a leading cause of morbidity and mortality in New Zealand. The treatment of cancer is often complex, requiring multidisciplinary specialist clinical input, and often places significant pressure on patients and their family and whānau.
Medical oncology is a core service underpinning successful cancer treatment. As a modality of cancer care, it is facing significant challenges that threaten the sustainability of cancer care services in New Zealand.
Medical Oncology National Implementation Plan 2012/13 v
Over the past decade, new treatment options have expanded care opportunities and increased rates of survival, while also making the system more complex and increasing workloads. For example, between 2007/08 and 2010/11 the number of people receiving chemotherapy increased by 39 percent. Yet, during this same time, cancer registrations increased by only 8 percent.
The system now faces significant operational and capacity pressures due to the increasing complexity of treatment, expanded treatment options, higher rates of survival, growth of multiple treatment cycles, rising patient expectations, and significant workforce and funding constraints. Additional issues are a wide variety of treatment practices along with duplicated systems and processes at treatment centres across New Zealand, and increasing pressure for subspecialisation.
Without system-wide change, the existing challenges will be compounded over the next
15 years, when the demand for medical oncology services in New Zealand is projected to nearly double. This growth in demand, coupled with the existing constraints on the workforce, facilities and funding, severely compromises the sustainability of services in the future.
The new medical oncology model of care
To address the growth in demand and current service challenges, the Ministry of
Health commissioned a report, New Models of Care for Medical Oncology (‘the
MOMOC report’) (Cranleigh Health, unpublished). The report described a new medical oncology model of care to ensure services are sustainable over the next 15 years.
Specifically it recommended:
1. creating a delineated service centre framework that defines service provision in terms of a national four-level, hub-and-spoke model
2. implementing a role delineation framework that identifies the tasks and functions on the patient care pathway that staff other than senior medical officers
(SMOs) can provide. This component would include taking on specialist nurses and introduces options for alternative 1 medical staff in hospitals and communities to focus the capacity of medical oncologists at key care delivery points
3. integrating care delivery using a tumour stream framework, which identifies how care will be delivered nationally and regionally, depending on the type of cancer, complexity of the treatment, and patient presentation.
Implementing the new medical oncology model of care
It is expected that the new model of care will be implemented over three to five years.
The Ministry of Health has prioritised a number of areas to initiate implementation at
1 Medical staff who are not employed as a medical oncologist. vi Medical Oncology National Implementation Plan 2012/13
a national level. The 12-month national implementation plan will commence in July
2012.
Table 1 summarises the activities recommended for beginning to implement the model in the 12 months of the 2012/13 fiscal year. It shows how each activity addresses a particular recommendation in the MOMOC report.
Table 1: Activities to address recommendations in the MOMOC report, over the
12 months of 2012/13
MOMOC recommendations
Implement a delineated service centre specification
Recommended activities for implementation
Implement a role delineation framework
Begin the workforce programme.
Appoint a national clinical lead to develop, with the sector, alternative clinical and non-clinical roles in medical oncology.
Appoint an oncology nurse clinical lead to develop, with the sector, the oncology nurse education pathway.
Support DHBs to develop short-term regional plans for the medical oncology workforce to increase the capacity of SMOs and oncology nurses, in line with the need indicated by local analysis.
Integrate services using a tumour type framework
Begin the service configuration programme.
Develop a self-assessment tool, based on a four-level service centre model, that DHBs can use to identify:
– the type and model of current provision of medical oncology services at regional or sub-regional and satellite centres
– ancillary services that support medical oncology services at regional or sub-regional and satellite centres
– regional strengths, interests and innovations, including projects and initiatives already under way, that align with implementation activities.
Refine the four-level service centre model, based on the DHB selfassessments, for sector consultation.
Begin the service quality programme.
Support development of national standards for tumour specific treatment through the Faster Cancer Treatment project.
Support quality improvement initiatives, such as multidisciplinary meetings, that are being undertaken through the Faster Cancer
Treatment project.
Medical Oncology National Implementation Plan 2012/13 vii
1 Overview
1.1 Purpose of the implementation plan
This plan outlines the priority areas of action to implement the recommendations of a report commissioned by the Ministry of Health, New Models of Care for Medical
Oncology (‘the MOMOC report’) (Cranleigh Health 2011). The report described a new medical oncology model of care for providing affordable, high-quality services sustainably in the future.
The plan focuses on the national activities to be undertaken in the first 12 months, which will inform regional and local implementation for the 2012/13 fiscal year and beyond. It also recognises the need to coordinate and integrate existing national, regional and local initiatives.
1.2 Implementation plan governance
To support the successful implementation of the new model of care, the Ministry of
Health has established the Medical Oncology Model of Care Steering Group (MOMOC
Steering Group). The role of this group is to provide leadership and direction on the development and evolution of services. It reports directly to the Cancer Programme
Steering Group. (See Appendix One for details.)
1.3 Reducing inequalities
This plan does not make specific recommendations for different population groups.
However planners, funders and service providers are encouraged to use the health equity assessment tools available to ensure all services and interventions consider equity.
Medical Oncology National Implementation Plan 2012/13 1
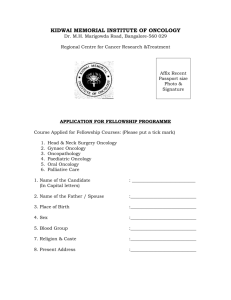
2 The need for medical oncology service improvement
Cancer is a leading cause of morbidity and mortality in New Zealand. The treatment of cancer is often complex, requiring multidisciplinary specialist clinical input, and often places significant pressure on patients and their family and whānau.
Medical oncology is a core service underpinning successful cancer treatment. As a modality of cancer care, it is facing significant challenges that threaten the sustainability of cancer care services in New Zealand. For example, between 2007/08 and 2010/11 the number of people receiving chemotherapy increased by 39 percent
(Figure 2.1). Yet, during this same time, cancer registrations increased by only
8 percent.
Figure 2.1: Provision of chemotherapy by fiscal year, 2008/09–2010/11
90,000
Number
Individuals receiving chemotherapy
Number of attendances/admissions
80,000
70,000
60,000
50,000
40,000
30,000
20,000
10,000
0
2007/08 2008/09 2009/10 2010/11
Financial year
As a result of this growth in demand as well as changes in treatment practices and expanded treatment options over the past 10 years, current service provision is substantially stretched. Indeed, some cancer centres are having challenges maintaining service levels.
2 Medical Oncology National Implementation Plan 2012/13
These current constraints are predicted to worsen. Over the next 15 years demand for medical oncology services in New Zealand is projected to nearly double. This growth in demand, coupled with the existing constraints on the workforce, facilities and funding, severely compromises the sustainability of services in the future.
The key challenges that underpin the need for service improvement are:
overburdened and limited resources, particularly for medical oncologists, including a high administrative burden
national and international workforce shortages
space and funding constraints at almost all regional cancer centres and district health boards (DHBs)
a wide variety of practices and care delivery models, along with duplicated systems, processes and priorities across the sector
increasing complexity of diagnosis and treatment, which is driving a need for subspecialisation a significant projected increase in demand over the next 15 years, driven by the ageing population, higher rates of survival, prolonged treatment times and expanding treatment options (see Figure 2.2)
rising patient expectations.
Figure 2.2: Projected number of patients starting chemotherapy, by regional cancer centre, 2010–2026
Year
The new medical oncology model of care, as outlined in the MOMOC report, was developed to address these challenges.
Medical Oncology National Implementation Plan 2012/13 3
3 Implementation plan framework
The MOMOC report (Cranleigh Health 2011) outlines the new medical oncology model of care in detail. In summary, the principles guiding the implementation of a new model of care are to:
maintain high quality of care and improve the quality of life for people with cancer
effectively, equitably and sustainably meet the future demand for medical oncology services, given significant workforce and resource constraints
ensure fiscal responsibility.
It is expected that the new model of care will be implemented over three to five years.
The Ministry of Health has prioritised several areas of activity to initiate implementation at a national level. The national implementation plan for the first
12 months of the new model of care will begin in July 2012 (see section 5).
Implementation priorities for DHBs in 2012/13, at both local and regional levels, are outlined in section 6 of this document.
Implementation activities have been grouped into three implementation programmes, based on recommendations outlined in the MOMOC report. Table 4.1 summarises each of these programmes. The rest of this section then details the rationale behind each programme; section 5 describes the implementation activities associated with each one.
Table 3.1: Overview of the three recommended implementation programmes
MOMOC recommendations
Recommended programme
Objective
Implement a delineated service centre framework
Service configuration programme
To help improve and reconfigure services and to increase treatment capacity in the appropriate facilities
Implement a role delineation framework
Workforce programme
Integrate services using a tumour type framework
Service quality programme
To develop and support workforce models that increase clinical capacity
To improve clinical quality and service efficiency so that patient care is equitable nationwide
4 Medical Oncology National Implementation Plan 2012/13
3.1 The implementation programmes
3.1.1 Service configuration programme
The objective of the service configuration programme is to help to improve and reconfigure services, and to increase treatment capacity in the appropriate facilities.
The programme will include defining the scope of service delivered at each centre level and the minimum resourcing, regional and national supports required.
The programme involves the development of a national four-level service centre framework and accreditation guidance (see Appendix Two). The framework is expected to provide clarity to stakeholders on service levels, improve the sustainability of service delivery and support the provision of standardised, high-quality care across the country.
The activities of the service configuration programme are to:
develop a national service centre model with a multi-level, hub-and-spoke structure
identify and support local and regional service configuration innovations and initiatives that align with the new model of care (see Appendix Three)
provide national guidance on future accreditation criteria and processes
guide the national phased implementation of the service configuration model
support the development of a national accreditation programme for delivering medical oncology services.
The following are the priority actions for 2012/13.
Develop a self-assessment tool, based on a four-level service centre model, that
DHBs can use to identify:
the type and model of current provision of medical oncology services at regional or sub-regional and satellite centres
ancillary services that support medical oncology services at regional or subregional and satellite centres regional strengths, interests and innovations, including projects and initiatives already under way that align with implementation activities.
Refine the four-level service centre model, based on the DHB self-assessments, for sector consultation.
See section 4.1.
Medical Oncology National Implementation Plan 2012/13 5
3.1.2 Workforce programme
The objective of the workforce programme is to develop and support workforce models that increase clinical capacity and capability.
Over the long term, the workforce programme is expected to support an increase in caseload capacity of senior medical officers (SMOs) from 180 First Specialist
Assessments (FSAs) per SMO (2011 national average) to 250 FSAs per SMO in 2026.
In the short term, it will probably be necessary to initially invest in or divert specialist capacity so that SMOs and nurses can engage in project implementation activities and so that services are continued. The SMO caseload and nurse scope of practice must not be expanded as recommended unless model enablers are implemented with successful and measurable outcomes.
The activities of the workforce programme are to:
develop guidance on alternative clinical and non-clinical roles and support activities by referencing appropriate domestic and international models and programmes
identify and support local and regional workforce innovations and initiatives that align with the new model of care (see Appendix Three)
guide the national roll-out of appropriate programmes for the medical oncology workforce.
The following are the priority actions for 2012/13.
Appoint a national clinical lead to develop, with the sector, guidance on alternative clinical and non-clinical roles in medical oncology.
Appoint a national oncology nurse clinical lead to develop, with the sector, the oncology nurse education pathway.
Support DHBs to develop short-term regional plans for the medical oncology workforce to increase the capacity of SMOs and oncology nurses, in line with the need indicated by local analysis.
See section 4.2.
6 Medical Oncology National Implementation Plan 2012/13
3.1.3 Service quality programme
The objective of the service quality programme is to improve clinical quality and service efficiency so that patient care is equitable and effective nationwide.
The programme involves the centralised development of tumour specific treatment guidance, protocols and service standards, data and information technology (IT) tools, and other process systems and supports. These resources will reduce duplication and improve service consistency.
Service providers will be able to deliver efficient, standardised and high-quality care by using best-practice tools and information. These include IT systems, operational and clinical resources (for example, common processes for multidisciplinary meetings
(MDM) and tumour standards) that are being developed nationally as part of the
Faster Cancer Treatment project.
The activities of the service quality programme are to:
develop standardised protocols and guidance tools to improve service consistency and the application of clinical best practice
identify and support local and regional quality innovations and initiatives that align with the new model of care (see Appendix Three) provide a resource repository to enable access to resources and tools that support service innovation, projects, programme evaluation and national implementation 2
provide access to data on diagnosis and medical oncology treatment 3
support the use of best-practice IT and other technology-based solutions for efficient care delivery
guide the national roll-out of appropriate service quality models including the development of training programmes.
The following are the priority actions for 2012/13.
Support the development of national standards for tumour specific treatment through the Faster Cancer Treatment project.
Support quality improvement initiatives, such as multidisciplinary meetings, that are being undertaken through the Faster Cancer Treatment project.
See section 4.3.
2 The Health Improvement and Innovation Resource Centre is a candidate for this repository.
Its services will need to be evaluated against user need.
3 The National View of Cancer is a candidate for these data.
Medical Oncology National Implementation Plan 2012/13 7
4 The 12-month implementation plan
The Ministry of Health has prioritised the following areas for action for 2012/13.
These are described in further detail in this section.
1 Begin the service configuration programme.
Develop a self-assessment tool, based on a four-level service centre model, that
DHBs can use to identify:
the type and model of current provision of medical oncology services at regional or sub-regional and satellite centres ancillary services that support medical oncology services at regional or subregional and satellite centres regional strengths, interests and innovations, including projects and initiatives already under way that align with implementation activities.
Refine the four-level service centre model, based on the DHB self-assessments, for sector consultation.
See section 4.1.
2 Begin the workforce programme.
Appoint a national clinical lead to develop, with the sector, guidance on alternative clinical and non-clinical roles in medical oncology.
Appoint a national oncology nurse clinical lead to develop, with the sector, the oncology nurse education pathway.
Support DHBs to develop short-term regional plans for the medical oncology workforce to increase the capacity of SMOs and oncology nurses, in line with the need indicated by local analysis.
See section 4.2.
3 Begin the service quality programme.
Support the development of national standards for tumour specific treatment through the Faster Cancer Treatment project.
Support quality improvement initiatives, such as multidisciplinary meetings, that are being undertaken through the Faster Cancer Treatment project.
See section 4.3.
8 Medical Oncology National Implementation Plan 2012/13
4.1 Service configuration programme: develop a national four-level service centre model
The service centre model includes the scope of service delivery for each type of treatment centre, the treatment complexity levels that each centre could safely deliver and the resourcing and support systems it would require to do so. Developing this model will include defining:
clinical and non-clinical services required to deliver certain levels of care
inter-centre roles and responsibilities
regional clinical and operation governance structures and lines of accountability.
Regional medical oncology services are at different stages of development, with varying levels of resource capacity. Their different priorities, levels of experience and interests have influenced their development and service planning. Understanding the level of service each DHB currently provides is crucial in the development of the service centre model.
Output A national four-level service centre model (see Appendix Two)
Purpose
Activities
0–12 months
To support forecasted changes in demand for medical oncology services
Consult with the National Health Board on the national four-level service centre model.
Develop a self-assessment tool, based on a four-level service centre model, that DHBs can use to identify:
the type and model of current provision of medical oncology services at regional or sub-regional and satellite cancer centres ancillary services that support medical oncology services at regional or sub-regional and satellite centres regional strengths, interests and innovations, including projects and initiatives already under way that align with implementation activities.
DHBs assess service configuration against the preliminary four-level service centre model that is proposed.
Refine the four-level service centre model, based on the DHB selfassessments, for sector consultation.
Organise a medical oncology innovation forum to share service improvement activities across DHBs.
Medical Oncology National Implementation Plan 2012/13 9
12 months and beyond
Lead
Linkages and dependencies
Circulate draft model and engage with sector to seek feedback.
Develop draft minimum service standards.
Develop accreditation standards and processes that support a four-level service centre model.
Guide and coordinate the national phased roll-out of the four-level service centre model.
Subject to funding, a national medical oncology service improvement fund may be established in 2013/14. DHBs and regional cancer networks could access this fund to support local and regional initiatives that are aligned to the new model of care.
Ministry of Health and DHBs
Service quality programme: The development of standards for tumour specific treatment will help to identify centres at which treatment and activity can safely be delivered.
National Health Board
Health Workforce New Zealand
Health Quality and Safety Commission
10 Medical Oncology National Implementation Plan 2012/13
4.2 Workforce programme: develop sustainable workforce models and education pathways
Devolving non-critical SMO activities to other clinical and non-clinical personnel will increase the capacity of SMOs to undertake essential activities. In the short term, the
MOMOC report recommends an increase in SMO positions to ensure service continuity, in line with the need indicated by local analysis.
In the longer term, using a patient pathway model as described in Appendix Four will ensure services are sustainable in the future in terms of having the workforce to support it. The model outlines what happens at points on that pathway, identifying who has the skills to do those tasks and then where best to learn the skills required.
Output A Guidance on alternative clinical and non-clinical roles in medical oncology
Purpose To maximise the workload capacity of SMOs to take on essential SMO activities
Activities
0–12 months
12 months and beyond
Lead
Linkages and dependencies
Additional considerations
Appoint a national clinical lead to develop, with the sector, alternative clinical and non-clinical roles in medical oncology.
The clinical lead will work with key groups to identify activities that can be devolved, and to define the scope of practice, training and qualification requirements and minimum support and supervision requirements to support these activities.
Implement alternative clinical and non-clinical roles in medical oncology.
Ministry of Health, SMO and nurse clinical lead, DHBs
Health Workforce New Zealand
Health Quality and Safety Commission
Relevant professional bodies
SMO Workforce Survey
With potential changes in roles, responsibilities and training programmes, it will be important to engage early with key training and union leaders at the:
Association of Salaried Medical Specialists
Royal Australasian College of Physicians
New Zealand Nurses Organisation
Health Workforce New Zealand.
Medical Oncology National Implementation Plan 2012/13 11
Output B
Purpose
Activities
0–12 months
An oncology nursing education pathway
To ensure oncology nursing staff are appropriately skilled for the tasks they are required to perform
Appoint an oncology nurse clinical lead to develop the oncology nurse education pathway with the sector.
The clinical lead will work with key nursing groups to:
identify specific nursing activities/tasks and competencies at each stage of the patient care pathway develop an education programme for oncology nursing, using existing education programmes and knowledge and skills frameworks engage with the sector to endorse this programme incorporate the agreed actions in the regional workforce plans.
Begin to implement the oncology nurse education pathway. 12 months and beyond
Lead
Linkages and dependencies
Additional considerations
Ministry of Health with the oncology nurse clinical lead
Existing nurse specialist training programmes
Existing academic nursing programmes
Previous and current nursing workforce initiatives
New Zealand Nurses Organisation
Health Workforce New Zealand
Health Quality and Safety Commission
With potential changes in roles, responsibilities and training programmes, it will be important to engage early with key training and union leaders.
12 Medical Oncology National Implementation Plan 2012/13
Output C
Purpose
Activities
0–12 months
Short-term regional plans for the medical oncology workforce
To ensure continuity of current medical oncology services
Support DHBs to develop short-term regional plans for the medical oncology workforce to increase the capacity of SMOs and oncology nurses, in line with the need indicated by local analysis.
Engage with the sector to gain its endorsement of the regional workforce plans.
Implement regional workforce plans. 12 months and beyond
Lead
Linkages and dependencies
Additional considerations
Ministry of Health, SMO and nurse clinical lead, DHBs
Health Workforce New Zealand
Health Quality and Safety Commission
Relevant professional bodies
SMO Workforce Survey
With potential changes in roles, responsibilities and training programmes, it will be important to engage early with key training and union leaders.
Medical Oncology National Implementation Plan 2012/13 13
4.3 Service quality programme: tumour standards, guidance and protocols
An estimated 70 percent of oncology treatments are considered routine; and the five most common cancers together account for 90 percent of cancer treatment volumes. It is therefore appropriate to develop national standards for tumour specific treatment.
Currently treatment guidance is duplicated at the six cancer centres. It is also considered difficult to maintain and regularly review.
The national tumour standard work groups, initiated as part of the Faster Cancer
Treatment project, are focused on eight tumour types. Following the development of the treatment standards more detailed work will begin on developing guidance and protocols for medical oncology treatment.
Output National standards, guidance and protocols on tumour specific treatment
Purpose
Activities
0–12 months
12 months and beyond
Lead
Linkages and dependencies
Additional considerations
To develop efficient and sustainable best-practice management of specific tumour types and promote a nationally coordinated and consistent approach to service provision
Support the development of national standards for tumour specific treatment through the Faster Cancer Treatment project.
Support quality improvement initiatives, such as multidisciplinary meetings, that are being undertaken through the Faster Cancer
Treatment project.
Align guidance for medical oncology treatment with the activity and outputs of other medical oncology workstreams (for example, oncology nursing education programme requirements or competencies).
Develop protocols and processes for post-treatment follow-up and review, including frequency of these services and clinician skill levels.
Ministry of Health
Existing tumour specific groups and initiatives (for example, the Faster
Cancer Treatment tumour groups and National Lung Cancer Working
Group)
Workforce and Service Configuration Programme activities
The development of the guidance on tumour specific treatment should take into account national priorities and best-practice clinical research.
14 Medical Oncology National Implementation Plan 2012/13
5 National roll-out
The expected outputs outlined in this plan will drive regional and local planning for
2012/13 and beyond.
The Ministry of Health will guide and coordinate the national phased roll-out with the cancer centres, DHBs and regional cancer networks, as outlined in Table 6.1 below.
Table 5.1: Roll-out activities by fiscal quarter year, 2012/13–2013/14
Ministry
Service configuration
Q1
Consult with
National Health
Board and develop assessment tool
Workforce
Quality
Q2
2012/13
Q3
Analyse assessments and refine tool
Scope nursing education pathway
Develop nursing education pathway
Scope alternative clinical and nonclinical roles in medical oncology
Begin to develop
Faster Cancer
Treatment tumour standards
Begin Faster
Cancer Treatment service improvement activities, including MDM initiatives
→
Q4
Hold medical oncology forum
Develop nursing education pathway
Consult on nursing education pathway
Support development of regional workforce plans
→ →
2013/14
Q1
Finalise service centre model
Finalise nursing education pathway
→
Medical Oncology National Implementation Plan 2012/13 15
DHBs
Service configuration
Q1
2012/13
Q2
Use assessment tool
Q3
Workforce Support workforce programme development
Quality
→
Support standard development
Support service improvement activities, including
MDM initiatives
→
→
→
Q4
Participate in medical oncology forum
Develop regional workforce plans
2013/14
Q1
Implement regional workforce plans.
→ →
16 Medical Oncology National Implementation Plan 2012/13
6 DHB implementation priorities for 2012/13
The majority of the activities in this plan are nationally led. However, in 2012/13 DHBs are expected to:
support service improvement and communication processes
assess current service configuration against the four-level service centre model
support increasing SMO capacity in line with the need indicated by local DHB analysis
support service improvement activities, including specific MDM processes
develop regional workforce plans
support workforce programme development by including agreed actions into the regional workforce plans.
Medical Oncology National Implementation Plan 2012/13 17
7 Communications and stakeholder consultation
The development of this implementation plan follows the recommendations of the
MOMOC report. That report was strongly informed by substantial sector engagement at regional cancer centres, DHBs and the cancer networks, and with sector experts.
This implementation plan has been developed by the Ministry of Health, key clinicians and sector experts, and the MOMOC Steering Committee.
As part of the ongoing implementation of the new model of care, the Ministry of Health will further engage with key stakeholders through written communications and face-toface meetings.
Initially the Ministry will hold a number of key meetings with the sector. These meetings will:
facilitate sector communication and discussion on the MOMOC report and implementation plan recommendations
discuss regional and local innovations
identify regional and local service structures and priorities.
18 Medical Oncology National Implementation Plan 2012/13
Reference
Cranleigh Health. Unpublished. New Models of Care for Medical Oncology: Report to the
Ministry of Health.
Medical Oncology National Implementation Plan 2012/13 19
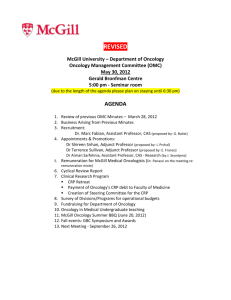
Appendix One: Groups and governance in the national cancer programme
Figure A1 below shows how the MOMOC Steering Group fits within the governance structure of the National Cancer Programme. Table A1 outlines the roles and linkages of each group in the programme.
Figure A1: Governance structure of the National Cancer Programme
Cancer Programme Steering
Group (CPSG)
MOMOC Steering Group
Cancer Treatment Advisory
Group (CTAG)
Medical Oncology Working
Group (MOWG)
Table A1: Roles and linkages of groups involved in the National Cancer Programme
Group Group role
CPSG Provides governance for the National Cancer
Programme
Oversees priority setting, planning and implementation of the programme
Formal linking members
National Clinical Director, Cancer
Group Manager, Personal Health
Service Improvement Group
CTAG Provides clinical advice on cancer treatment to
CPSG
National Clinical Director, Cancer
MOWG Provides clinical advice on issues relating to medical oncology. This group reports to CTAG
The Chair (or representative of
MOWG) is a member of CTAG
MOMOC
Steering
Group
Develops and drives the implementation of a
12-month national work plan for the medical oncology model of care
Provides national leadership and reports on implementation progress
Reports to CPSG
National Clinical Director, Cancer
Group Manager, Personal Health
Service Improvement Group
20 Medical Oncology National Implementation Plan 2012/13
Appendix Two: Description of proposed four-level service centre framework
Centre level
Service elements of each centre
Level 1 These centres can be located in urban or rural areas and provide non-complex, lowrisk, day-case chemotherapy treatment, patient education and appropriate follow-up services.
Care would be primarily nurse-led and provided by a specialist medical oncology nurse, supported or supervised by a dedicated general physician or medical officer of special scale. Some opportunities exist for general practitioners to also become involved in care delivery or follow-up management in centres with appropriate credentials (eg, integrated family health centres).
Specialist medical oncology nurses, medical officers of special scale and general practitioners would have received appropriate postgraduate training and potentially further training through regional centre rotations.
Clear standards, protocols, processes and delegated authorities are recommended to:
support nurse-led clinical decision-making
help escalate acute care needs to regional centres, emergency departments or other after-hours care.
Local referrers (eg, surgeons) would participate in and refer to regional MDM networks via video conferencing.
It is unlikely that these centres would provide direct specialised outpatient clinic services, unless they were given the appropriate support (eg, through telemedicine).
Level 2 Level 2 centres would provide a Level 1 service, plus:
low-complexity, outpatient clinic care by generalist SMOs, who would be advised by regional subspecialty leads or networks and national standards and protocols regular outpatient clinics by a visiting medical oncologist
pre- and post-clinic clinical support (minimum one nurse per clinician), ideally with a community or complex needs coordinator support from the complex needs coordinator for family physicians and other providers caring for cancer patients.
Medical Oncology National Implementation Plan 2012/13 21
Centre level
Service elements of each centre
Level 3 Level 3 centres would provide a Level 2 service, plus:
chemotherapy treatment for the majority of complex day cases and outpatients
inpatient care in general medical ward (non-treatment) a 9 am–5 pm medical oncologist (SMOs or resident medical officers – RMOs)
± a visiting oncologist; SMOs participate in regional subspecialty network
RMO training advanced nursing care practice a local MDM for high-volume activity clinical trial involvement
a clinical oncology pharmacy service that includes compounding capacity to meet acute care and clinical trial needs.
Level 4 A Level 4 centre would provide a Level 3 service, plus all components of a comprehensive cancer service including:
all forms of inpatient and day-case chemotherapy treatment haematology, radiation oncology and palliative care
inpatient beds for admission under specialist medical oncologists a 24/7 medical oncologist SMO plus RMO cover
SMO subspecialisation/interest for common cancers and specialist network for rarer cancers local and regional specialist MDM support for all common cancer types
advance nursing care through a clinical nurse educator, a site- or specialtyspecific clinical nurse specialist or nurse practitioner the ability to conduct and coordinate clinical trials oncology acute care services, ideally with appropriate systems and training for the emergency department and a 9 am–5 pm acute care service within the oncology unit capabilities to manage, oversee, support and accredit other oncology service sites, to ensure medical oncology services are delivered in a safe, coordinated manner across the region.
22 Medical Oncology National Implementation Plan 2012/13
Appendix Three: Summary of local models of care
Model
Subspecialty model
Physician with special interest
Community nurse-led model
Nurse practitioner
Tumour specific
‘cheat sheets’
Description Sample sites
Subspecialty model is implemented in some regional cancer centres where SMOs have developed cancer-specific interest and subspecialisation
Auckland
Waikato
A physician with special interest in oncology provides medical support in a local satellite centre with linkages to a medical oncologist at a regional cancer centre
Local Invercargill specialists may refer to Invercargill-based physician for advice
Invercargill cases go through an MDM at a regional cancer centre (Otago)
Invercargill
Community nurses participate in assessments alongside medical oncologists
In the West Coast use of video conferencing systems are used to support care delivery
Wellington
West Coast
A clinical nurse specialist role has been established that could develop into a nurse practitioner model
In a regional cancer centre, tumour specific guidelines or
‘cheat sheets’ have been developed to assist generalist medical oncologists with care delivery
Palmerston
North
Christchurch
Source: Cranleigh Health (unpublished), Appendix Four.
Medical Oncology National Implementation Plan 2012/13 23
Appendix Four: Key pathway points and components
Pathway points Role and pathway model components
Diagnosis and referral Some of the workload of SMOs and other clinical staff could be reduced through improved diagnosis and referral standards.
It is understood that a number of inappropriate referrals are made currently and that, with the appropriate standards, care could be devolved and directed to more appropriate clinicians or services.
Furthermore, many referrals have insufficient information and can add to SMO or nursing workloads.
Therefore, it is recommended that the referring clinicians compile a complete referral with all supporting information in line with national standards.
This diagnosing lead clinician will send this referral in a timely manner to the appropriate MDM or medical oncology service.
Multidisciplinary meetings
Ideally the majority of cancer diagnosis and treatment referrals are discussed at a specialist MDM that is attended by an appropriate:
medical and radiation oncologist radiologist
pathologist specialist nurse surgeon and/or physician and/or referring clinician if not one of the above.
Rather than being coordinated by clinical staff, MDMs would be supported by dedicated coordinators and national standards, processes and tools.
Referral receipt and prioritisation
Pre-FSA
Rather than prioritising for SMOs, a specialist nurse could manage initial screening and work up for common or standard cases in line with national standards. There are also opportunities to build this procedure into the MDM and treatment planning processes. An SMO would assess complex cases based on escalation criteria.
A specialist nurse could complete a pre-FSA checklist (by cancer type)- links to MDM and referral protocols.
24 Medical Oncology National Implementation Plan 2012/13
Pathway points
First Specialist
Assessment
Post-FSA
Education and consent
Booking and scheduling
Treatment
On-treatment follow-ups
Complications and symptoms
Role and pathway model components
Assessment (or part of the assessment) of simple, non-complex, standard cases could potentially be devolved to non-SMO clinicians
(eg, a supervised specialist nurse, medical officer of special scale or a general practitioner with training in oncology).
Increasing the nursing and administrative supports at the outpatient clinic appointment (eg, one nurse per clinician) is expected to reduce the administration burden on SMOs, increase patient throughput, support a better team approach and improve patient continuity of care
(with specialist nursing becoming a familiar first point of contact).
Other appropriately trained staff, such as enrolled nurses or administrators, could provide post-FSA support, thus increasing the capacity of both SMOs and specialist nurses.
With the appropriate tools and standards, activities could include counselling, education, pre- and post-clinic follow-up activities, clinical administration support (eg, additional investigations and referrals), and complex needs management.
With the appropriate tools and standards, education and patient consent may be devolved to appropriately trained nurses, RMOs or well-supported providers in satellite services.
Enrolled or registered nurses or administrative staff could lead patient booking and scheduling.
Staff members would be guided by:
national treatment standards or protocols that define minimum centre support (Levels 1–4)
FSA scripts
nurse resourcing (minimum nurse and skill mix per patient ratio) treatment time requirements.
Specialist nurses could manage treatments in line with national treatment standards and local delivery protocols including escalation pathways.
Minimum requirements for postgraduate training and/or experience and resourcing would need to be defined so that all centres deliver care safely.
Minimum levels of clinician supervision support would be defined when a medical oncologist is not on site.
Specially trained and experienced enrolled or junior nurses could provide additional treatment delivery support so that the specialist nurse could focus on critical specialist tasks.
Follow-ups could be partially devolved to qualified registered nurses to manage using standards and escalate as required.
Qualified registered nurses could manage complications and symptoms, using protocols, standards, standing orders and escalation pathways.
Medical Oncology National Implementation Plan 2012/13 25
Pathway points
Follow-up and discharge
Role and pathway model components
Subsequent cycles and restaging
Non-SMO clinicians or nurses could manage and assess non-complex, low-risk, standard cycles and/or assist in the restaging process.
Follow-ups may be shared with other specialities or clinical staff (eg, general practitioners with training in oncology, specialist oncology nurses, and radiation oncologists for specific tumour types).
A clearly defined pathway would ensure access to SMOs for appropriate input when required.
Source: Cranleigh Health (unpublished).
26 Medical Oncology National Implementation Plan 2012/13