CHAPTER 33 - Nursing Pharmacology FrontPage
advertisement

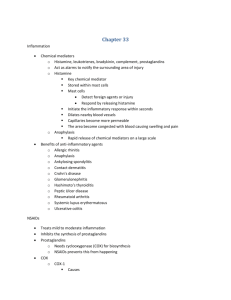
CHAPTER 33 DRUGS FOR INFLAMMATION AND FEVER LEARNING OUTCOME 1 Explain the pathophysiology of inflammation and fever. Concepts 1. Inflammation is a natural, nonspecific body defense that limits the spread of invading microorganisms or injury. Occurs in response to an injury or antigen. The central purpose of inflammation is to contain the injury or destroy the microorganism. Inflammation is not a disease, but a symptom of an underlying disorder. By neutralizing the foreign agent and removing cellular debris and dead cells, repair of the injured area can proceed at a faster pace. Inflammation limits the spread of injury or antigens by containing the injury or destroying the microorganism. Acute inflammation occurs over several days, whereas chronic inflammation may continue for months or years. 2. Signs and symptoms of inflammation include swelling, pain, warmth, and redness. LEARNING OUTCOME 2 Outline the basic steps in the acute inflammatory response. Concepts 1. Damaged tissue releases chemical mediators that alert the surrounding area of injury. The chemical mediators are histamine, leukotrienes, bradykinin, complement, and prostaglandins. (See Table 33.1 to see the sources and actions of these mediators.) 2. There are five basic steps in acute inflammation. They occur after cellular injury causes release of chemical mediators. The steps are vasodilation, vascular permeability (edema), cellular infiltration (pus), thrombosis (clots), and stimulation of nerve endings (pain). (See Figure 33.1 for an illustration of the steps of inflammation.) LEARNING OUTCOME 3 Explain the role of chemical mediators in the inflammatory response. Concepts 1. Histamine is a key chemical mediator in inflammation. It is stored in mast cells and initiates the inflammatory response. It directly stimulates pain receptors. Release of histamine produces vasodilation, allowing capillaries to become leaky, causing tissue swelling. Histamine is responsible for the symptoms of anaphylaxis. 2. There are two different receptors with which histamine interacts to elicit a response. H1 receptors are present in the smooth muscle of the vascular system, the bronchial tree, and the digestive tract. Stimulation of these receptors results in itching, pain, edema, vasodilation, bronchoconstriction, and the characteristic symptoms of inflammation and allergy. In contrast, H2 receptors are primarily present in the stomach, and their stimulation results in the secretion of large amounts of hydrochloric acid. Adams Ch 33-1 LEARNING OUTCOME 4 Outline the general strategies for treating inflammation. Concepts 1. Identify and treat the underlying cause. Inflammation is usually self-limiting and nonpharmacologic treatments such as ice packs and rest should be used for mild symptoms. Anti-inflammatory creams, ointments, patches, suppositories, and intranasal sprays are used for inflammation of the skin and mucous membranes of the mouth, nose, rectum and vagina. Many of these are available over the counter (OTC). 2. The goal is to prevent or decrease the intensity of the inflammatory response and reduce fever. Common diseases that benefit from anti-inflammatory agents include allergic rhinitis, anaphylaxis, ankylosing spondylitis, contact dermatitis, Crohn’s disease, glomerulonephritis, Hashimoto’s thyroiditis, peptic ulcer disease, rheumatoid arthritis, systemic lupus erythematosus, and ulcerative colitis. LEARNING OUTCOME 5 Compare and contrast the actions and adverse effects of the different nonsteroidal anti-inflammatory drugs (NSAIDs). Concepts 1. Nonsteroidal anti-inflammatory drugs (NSAIDs) are the primary drugs for the treatment of simple inflammation. This drug class includes aspirin, ibuprofen, and COX-2 inhibitors (see Table 33.2). All have about the same efficacy, but the side effects vary. All are also analgesics and antipyretics. Acetaminophen has no anti-inflammatory action and is not an NSAID. 2. There are two forms of the enzyme cyclooxygenase (COX) (see Table 33.3). Cyclooxygenase -1 (COX-1) is present in all tissues. It reduces gastric-acid secretion, promotes renal blood flow, and promotes platelet aggregation. Inhibition of COX-1 results in bleeding, gastric upset, and reduced renal function. Cyclooxygenase-2 (COX-2) is present at sites of injury. It promotes inflammation, sensitizes pain receptors, and mediates fever in the brain. Inhibition of COX-2 results in suppression of inflammation. 3. Aspirin treats inflammation by inhibiting both COX-1 and COX-2. It is readily available, inexpensive, and effective. Large doses are needed to relieve severe inflammation. Adverse effects include irritation to the digestive system, bleeding, and salicylism (tinnitus, dizziness, headache, excessive perspiration). 4. Ibuprofen is an alternative to aspirin. It inhibits COX-1 and COX-2. A common side effect is nausea and vomiting. Ibuprofen causes less gastric irritation and bleeding than aspirin. 5. COX-2 inhibitors are the newest and most controversial class. They do not inhibit COX-1; thus, they do not affect blood coagulation and do not irritate the digestive system. They were the treatment of choice for moderate to severe inflammation until 2004 when rofecoxib (Vioxx) was found to double the risk of heart attack and stroke and was subsequently removed from the market. Valdecoxib (Bextra) was also removed in 2005. Celecoxib (Celebrex) is the only remaining COX-2 inhibitor. Ch 33-2 Adams LEARNING OUTCOME 6 Explain the role of glucocorticoids in the pharmacologic management of inflammation. Concepts Systemic glucocorticoids are effective in treating acute or severe inflammation. They are naturally released from the adrenal cortex, suppress histamine and prostaglandins, and can inhibit the immune system to reduce inflammation. (See Table 33.4 for a list of glucocorticoids.) Serious adverse effects may include suppression of adrenal-gland function, hyperglycemia, mood changes, cataracts, peptic ulcers, electrolyte imbalances, and osteoporosis. Glucocorticoids can also mask infections; this creates the potential for existing infections to grow rapidly and undetected. For this reason, glucocorticoids are contraindicated in active infections. Glucocorticoids are used for short-term treatment of acute inflammation. If they are absolutely necessary for long-term treatment, the dose is kept as low as possible, and use of alternate-day dosing is established. Cushing’s syndrome may result when glucocorticoids are used long term. They must be gradually discontinued. LEARNING OUTCOME 7 For each of the classes listed in Drugs at a Glance, know representative drugs, and explain their mechanisms of drug action, primary actions related to inflammation and fever, and important adverse effects. Concepts 1. Anti-inflammatory Drugs—NSAIDs. Prototype drug: ibuprofen (Advil, Motrin, others). Mechanism of action: to inhibit prostaglandin synthesis. Primary use: for musculoskeletal disorders such as rheumatoid arthritis and osteoarthritis, mild to moderate pain, reduction of fever, and primary dysmenorrheal pain. Adverse effects: nausea, heartburn, epigastric pain, and dizziness. 2. Anti-inflammatory Drugs—Systemic Glucocorticoids. Prototype drug: prednisone (Meticorten). Mechanism of action: being metabolized to an active form of glucocorticoids. Primary use: to treat inflammation. Adverse effects: Cushing’s syndrome if used for long-term therapy. 3. Antipyretics. Prototype drug: acetaminophen (Tylenol). Mechanism of action: to reduce fever by direct action at the level of the hypothalamus and dilation of peripheral blood vessels, which enables sweating and dissipation of heat. Primary use: to relieve pain and reduce fever. It has no anti-inflammatory properties. Adverse effects: possible liver damage. It has less gastric irritation than aspirin and does not affect blood coagulation. Prototype Drug ibuprofen (Advil, Motrin, others) prednisone (Meticorten) patients in clinical this week. Adams Ch 33-3 LEARNING OUTCOME 8 Use the nursing process to care for patients receiving drug therapy for inflammation and fever. Concepts 1. Assessment: Obtain a complete health history (hepatic, renal, respiratory, cardiovascular or neurologic disease, pregnancy or breast-feeding), including data on origin of fever, recent surgeries, or trauma. Obtain baseline vital signs and weight. Obtain patient’s complete medication history, including nicotine and alcohol consumption, herbal-supplement use, and use of alternative therapies, to determine possible drug allergies and/or interactions. Evaluate appropriate laboratory findings (e.g., CBC, coagulation panels, bleeding time, electrolytes, glucose, lipid profile, hepatic or renal function studies). Assess patient’s ability to receive and understand instruction. Assess for and promptly report adverse effects: symptoms of GI bleeding (dark or “tarry” stools, hematemesis or coffee -ground emesis, blood in the stool), abdominal pain, severe tinnitus, dizziness, drowsiness, lightheadedness, confusion, agitation, euphoria or depression, palpitations, tachycardia, hypertension, increased respiratory rate and depth, pulmonary congestion, edema. 2. Nursing Diagnoses: Pain; Hyperthermia; Risk for Injury (hepatic toxicity); Fluid Volume Deficit related to fever; Risk for Injury related to adverse drug effects; Risk for Infections related to adverse drug effects of glucocorticoids; Risk for Impaired Skin Integrity related to adverse drug effects of glucocorticoids. 3. Planning: The patient will experience diminished fever, decreased or absent pain, decreased signs and symptoms of inflammation; be free from or experience minimal adverse effects. Verbalize an understanding of the drug’s use, adverse effects, and required precautions. Demonstrate proper selfadministration of the medication (e.g., dose, timing, when to notify provider). 4. Implementation: Assess for intolerance to ASA for possible cross- hypersensitivity to other NSAIDs or acetaminophen. Monitor hepatic and renal function. Monitor for abdominal pain and change in color of stool (gastrointestinal bleeding), hearing and balance (ototoxicity), and vision. Monitor electrolytes, bloodglucose and lipid levels periodically (hyperglycemia from corticosteroids). Monitor for signs and symptoms of infection in patients on corticosteroids. Monitor for osteoporosis and unusual changes in mood or affect in patients on corticosteroids. Weigh the patient on corticosteroids. Weigh the patient daily and report weight gain of 1 kg or more in a 24-hour period or more than 2 kg per week or increasing peripheral edema. Avoid use of aspirin or salicylates in children under 18. Do not stop corticosteroids abruptly. Use with caution in patients with a history of excessive alcohol consumption. Use with caution in patients with diabetes. 5. Evaluation: The patient experiences diminished fever, decreased or absent pain, decreased signs and symptoms of inflammation; is free from or experiences minimal adverse effects. Verbalizes an understanding of the drug’s use, adverse effects, and required precautions. Demonstrates proper selfadministration of the medication (e.g., dose, timing, when to notify provider). Ch 33-4 Adams