Physio Lecture 4 ABO Typing
advertisement

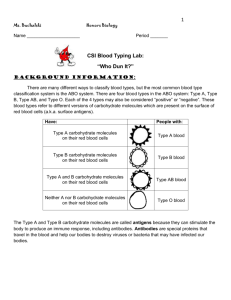
Physio Lecture 4: Blood Typing: ABO blood groups This will be easy or hard for you. It is easier if you have had Microbiology. Carl Landsteiner discovered the ABO blood type, system and won Nobel Prize. An antigen is anything, usually a protein or sugar, that the body does not recognize, and can elicit an immune response. A, B, and D (Rh) are antigens. They are proteins on red blood cell membranes, and the proteins have sugars that stick out on their tails. You are in LAX, trying to get your black suitcase off the luggage carousal. Everyone else’s suitcase is black, too, but they each have their own ID tag on it. Diana walks up, grabs a bag, does not check the ID tag, and it is not hers, it belongs to Julie. When Diane tries to leave the airport, an alarm goes off and provokes the police to come after her. If she checked it first to make sure it was hers, it would not provoke an attack. Every cell in your body is like your luggage; it has your ID tag on the surface of the cell membrane. If you take Diane’s cells and put them into Julie’s body, Julie’s police will go after invading cell. Why don’t Diane’s cell antigens provoke an immune response to her own cells? If they did, it would be abnormal, called an autoimmune disease. Your immune system scans for antigens. If one is found, the macrophages, neutrophils, and, if necessary, the T cells will be sent to destroy it. RBCs are the most numerous of all cells, making up 25% of your body’s cells. There is an ID marker on each one that tells us what blood type you are. These ID markers, or antigens, can be A, B, and/or D (Rh). The last sugar in the chain of the antigen determines you blood type. Type A’s terminal sugar is N-acetylglucosamine, type B’s sugar is galactose, and type D’s terminal sugar is proline. Type O does not have a terminal sugar. Type AB has two terminal sugars. Blood type A has its terminal sugar represented as a pyramid shape on the slide. If you are type A, do you want to make antibodies to fit the pyramid? No, those antibodies will attack, causing agglutination (not coagulation). Agglutination is an Immune response that involves antibodies that recognize an antigen, and a bunch of these antibodies pile onto the antigen, causing the whole complex to precipitate out of solution. Coagulation is blood clotting, and has nothing to do with antibodies or RBCs. The Incredibles are a family of super-heroes; the husband finds himself in the enemy lair. An intruder alert sounds, and as he tries to run away, a little sticky tar ball shoots out of the wall and sticks to him. He is very large, so he laughs it off and keeps running. But as more and more tar balls are shot at him, they stick all over his body until he is completely engulfed in them, can no longer move, and he is plastered onto the ground. The sticky tar balls are like WBC’s attaching to the antigens on the RBCs. Antibodies can also cause an RBC to pop (hemolysis), and the hemoglobin pours out. We don’t want patients to get foreign RBCs during a blood transfusion. If the blood typing machine is not cleaned correctly, it might type the blood wrong, so you have to it check manually sometimes. In the future, it may be obsolete to have blood typing: they are taking blood, using enzymes to chew off the antigens so there are no ID tags, and no immune response will occur. They are also trying to make synthetic blood. Although the most common proteins on RBCs are A, B, and D (the Rh factor), there are other RBC proteins that are rare, and can possibly provoke an immune response. These people cannot even have O negative blood, so you have to see if their family might have a compatible type, since they may have the same genes. There are ranges in antigenicity; some of the ABD proteins are better than others at provoking the immune response. Some are very antigenic, some are not as antigenetic. Those that are not very antigenic take frequent exposures before provoking a response. An antigen on a RBC is called an agglutinogen; it provokes an immune response. An antibody in the plasma that would recognize an antigen on a foreign RBC is an agglutinin. For example, blood type A has agglutinogens that will be attacked by a person with blood type B. The person with type B will produce agglutinins (antibodies) against type A agglutinogens. These agglutinins are called anti-A antibodies. A person with type A blood will produce anti-B antibodies. A person with type B blood will produce anti-A antibodies. Since type O does not have a terminal sugar, there is no such thing as anti-O antibodies. If you are type AB, you have no anti-A or anti-B antibodies. Type O has both anti-A and anti-B antibodies. You have antibodies against the blood type that you don’t have. “Rho” is Rh factor (called D factor). It is not as antigenic as A and B; it takes time to be exposed to it. If you have the D antigen, you Rh+ and if you don’t have it you are Rh negative. Rh + is a dominant gene so more people are Rh+. People who are Rh negative will still make anti-A or anti-B antibodies, so if you give an AB+ person AB negative blood, it will cause agglutination. Rules of blood typing 1. Figure out what blood type they have 2. Ask yourself which antibodies they make 3. What blood type can they receive? 4. What blood types can they donate blood to? 5. Don’t give a person a foreign blood type When we take blood from a person to donate to someone else, we first separate RBCs, remove their antibodies by washing them, and then given the infusion. We do not want the recipient’s body to attack the donor’s RBCs. What type is Julie? She does not want to have blood drawn. That’s okay; we can tell her blood type without her blood. Take a bottle of anti-A antibodies and inject some into Julie. If she lives, she has type B or O blood. If she dies, she has the A antigen, so we know she has either type A or AB blood. If she survived, we then take a bottle of anti-B antibodies and inject them into Julie. If she lives, she is type O. If she dies, she is B or AB. However, if she was type AB, she would have died in the first injection. If it took two injections to kill her, she was type B. Here is a more practical way to determine blood type: Put a drop of blood onto a card, add one drop of anti-A antibodies onto the blood drop, and swirl. Put a drop of blood onto a card, add one drop of anti-B antibodies onto the blood drop, and swirl. Put a drop of blood onto a card, add one drop of anti-D antibodies onto the blood drop, and swirl. Check for which of the three blood drops agglutinate (clump). Agglutination on A and D 1. Figure out what blood type they have: A+ 2. Ask yourself which antibodies they make: Anti B 3. What blood type can they receive? A+ or O+ 4. What blood types can they donate blood to? A+, O+ Agglutination on B and D 1. Figure out what blood type they have: B+ 2. Ask yourself which antibodies they make: Anti A 3. What blood type can they receive? B+ or O+ 4. What blood types can they donate blood to? B+, O+ Agglutination in all three 1. Figure out what blood type they have: AB+ 2. Ask yourself which antibodies they make: none 3. What blood type can they receive? any 4. What blood types can they donate blood to? AB+ and O+ Agglutination on A only 1. Figure out what blood type they have: A negative 2. Ask yourself which antibodies they make: Anti B and Anti D 3. What blood type can they receive? A negative or O negative 4. What blood types can they donate blood to? A+, A neg, O+, O neg Agglutination on B only 1. Figure out what blood type they have: B negative 2. Ask yourself which antibodies they make: Anti A and Anti D 3. What blood type can they receive? B negative or O negative 4. What blood types can they donate blood to? B+, B neg, O+, O neg Agglutination in A, B, but not D 1. Figure out what blood type they have: AB negative 2. Ask yourself which antibodies they make: Anti-A and Anti-B 3. What blood type can they receive? A neg, B neg, AB neg, O neg 4. What blood types can they donate blood to? O+ and O neg Type AB+ can get any blood. It is the universal recipient. No agglutination 1. Figure out what blood type they have: O negative 2. Ask yourself which antibodies they make: Anti-A, anti-B, anti-D 3. What blood type can they receive? O negative only 4. What blood types can they donate blood to? Anyone O negative can be given to anyone. It is the universal donor. Agglutination in O only 1. Figure out what blood type they have: O+ 2. Ask yourself which antibodies they make: anti-A, anti-B 3. What blood type can they receive? O+ and O neg 4. What blood types can they donate blood to? AB+ and O+ Type O+ is the most common type, but type O negative is the rarest. If you don’t understand the logic of it, memorize the chart instead of figuring it out. NOTE: California uses the most blood for transfusions. We also give the least blood. What if you were a field medic and you could not do a blood typing before transfusion? Prick the thumb of the donor and mix a drop of blood with the recipient: Those donors who agglutinate cant donate. Erythroblastosis Fetalis (Hemolytic Disease of the Newborn, or HDN) The baby and mom have different blood types. The baby has antigens that mom’s immune system creates antibodies against. Mom’s antibodies cross the placenta, causes hemolysis in the fetus. ABO and Rh incompatibility The blood in the baby’s vessels travels in a counter current direction compared to the Mom’s blood vessels, with no shared vessel. How does mom become sensitized to the baby’s antigens? There are times where mixing can occur. She trips, gets a micro tear in placenta, antibodies can cross the placental barrier. Or perhaps Mom has an amniocentesis, can cause mixing there. Another way is if she has an abortion, or if she delivered a previous baby with an incompatible blood type: as the placenta detaches, there is always mixing. The most common HDN is from ABO incompatibility. Mom is O, baby is A. Mom’s anti-A antibodies cross the placenta and attack; this is very common, but clinically not a problem. Time is on the baby’s side. The baby’s RBC antigens are not expressed because the sugar is not put in place until very late in the pregnancy. That’s why it is hard to blood type a newborn. They always get type O negative if they need blood. Rh incompatibility. Mom is Rh neg and baby is Rh + This is less common and much more dangerous. Most of us are Rh +, but if dad is + and mom is negative, the baby tends to be Rh+. Her first pregnancy goes fine. During delivery, as the placenta tears away, she becomes sensitized. During each of the next pregnancies, her Anti-D antibodies attack the child. The first pregnancy has only about 3% chance of being a problem. The second pregnancy has a 15% chance of being a problem. Don’t want that high of a chance! Prevention of HDN Prevent HDN by giving Mom a shot after placenta is delivered. The medicine is RhoGam, which are anti-D antibodies. The very thing we don’t want her to make, she gets! This is passive immunity. The process is called neutralization. With the injected anti-D antibodies present in the mom, she will not make any herself. All of the baby’s red blood cells that escaped into the mother’s circulation after the placenta detached get their D antigens covered up by the injected anti-D antibodies, so the mom does not make her own anti-D antibodies. The injected antibodies technically could cross from the mother to the placenta of the next child, but they don’t because they degrade before the next pregnancy. The Mom has to have the shot at 28 weeks pregnant and again within a few hours after delivery. When a mom is Rh negative, you don’t bother checking dad’s blood type because you can’t be sure that he is the baby’s father. Give the shots every time the mom is Rh negative. Treatment of HDN Prenatal Treatment: intrauterine transfusion. Exchange transfusion during pregnancy. Take out baby’s blood while putting in O negative blood. New RBCs are made in the baby’s bone marrow, but they only live for 120 days, so it won’t change the baby’s genetic blood type. Transfusions are done over a 6 week period. Postnatal Treatment: Phototherapy, exchange transfusion if necessary The exchange transfusion is with O or D negative blood. When Hgb is destroyed, the heme (ring) around the iron has to be removed from the body. The ring turns into bilirubin, which is hydrophobic, and does not like to go into transcellular compartment. The liver needs to make it hydrophilic; it does this by conjugating it. But in a newborn baby, the liver is busy doing a lot of other things, too, and may not be able to handle everything. In that case, the liver enlarges, trying to accommodate the demand of these functions. The spleen may also enlarge. We need to help the baby convert the heme ring by using ultraviolet phototherapy. The baby is exposed to UV light at birth and one week later. Dangers of HDN If the baby with HDN survives massive hemolysis, there are other problems to deal with. Anemia can arise from deformed hemoglobin. There are four oxygens per hemoglobin molecule, and if there is only one oxygen missing, it causes problems with organs that need the most oxygen (heart, brain, and kidney). A build-up of bilirubin can also kill neurons; a condition called kernicterus. The spleen and liver can enlarge (hepatosplenomegaly) and put pressure on the organs.