Examining Existing Barriers And Oral Health Outreach For Low
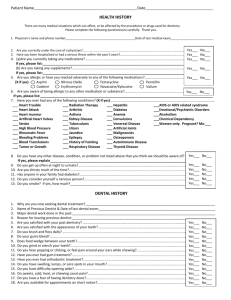
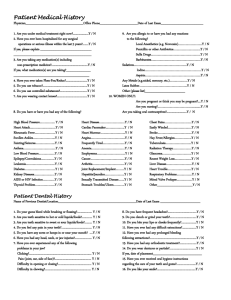
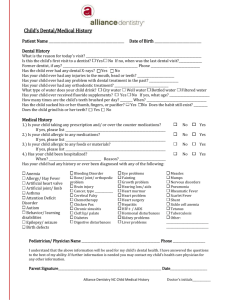
advertisement

Giving a Voice to the ‘Silent Epidemic’: Examining Existing Barriers and Oral Health Outreach for Low Income Mexican American Children By Victoria Benson 26 May 2009 Advisor: Eunice Rodriguez, Pediatrics Second Reader: Tania Mitchell, Comparative Studies in Race and Ethnicity Submitted to the Program in Comparative Studies in Race and Ethnicity in partial fulfillment of the requirements for the Undergraduate Honors Program i Abstract A 2000 Surgeon General Report declared oral health disparities among children of low socioeconomic status (SES) a silent epidemic. Research shows Mexican American children have disproportionately high occurrences of oral disease compared to their White counterparts. A community intervention of The Health Trust (THT) is examined using a phone survey (n= 168) and participant focus groups (n=19) to understand how oral health outreach prepares low SES Mexican families to address oral health barriers. Cultural oral health practices and their role in oral health disparities are also explored. Results indicate the program’s success in teaching preventative oral health practices, but improvement is needed to address lack of dental insurance (26.4%), language differences (16.5%), discomfort with available dentists (15.6%), and negative experiences with dentists. Cultural oral health practices do not appear to contribute to oral health disparities in Mexican American children; however, these practices reflect low SES conditions. ii Acknowledgements Writing this honors thesis has been an irreplaceable experience that would not have been possible had I not had the wonderful support and encouragement from the following individuals. To my family who have never stopped believing in me. Everyday I think about how fortunate I am to have the love and support you all provide. To Eunice Rodriguez who was bold enough to embark upon this project with me. Your guidance has allowed me to achieve more than I knew I could. To Tania Mitchell, your advice and dedicated presence (in the office and at your home) is greatly appreciated. I enjoyed working with you. I would not have challenged myself to start this project had it not been for Rand Quinn and Dr. Jeanne Tsai’s influence and enthusiasm. To THT, Aimee Reedy, Daryl Nguyen, and Mario Tercero for making this project possible. To Odette Avalos, Ernesto Castillo, Karla Martinez and Carlos Fonseca for providing the link between my participants and me. To every other CSRE student who embarked upon this project with me. You provided support and camaraderie just when I needed it. Thank you all so much. iii Table of Contents 1 Introduction 8 Literature Review 31 Methodology 42 Results 62 Discussion 78 Conclusion 82 Appendices 114 Bibliography iv Figures and Tables 46 Figure 1: Code Categories for Perception of THT 49 Figure 2: Code Categories for Oral Health Practices of Participants 53 Figure 3: Code Categories for Barriers in Maintaining Children’s Oral Health 61 Table 1: Sample Statements of Cultural Oral Health Related Practices v Acronyms and Foreign Words THT - The Health Trust SES – Socioeconomic Status Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment dental services program – EPSDT Community-Based Participatory Research – CBPR Promotores(as) – Lay health educators from Latino communities vi Introduction Oral health is often overlooked when considering necessary health care both by health care providers and by the general population. However, oral health plays a large role in everyday comfort and can also affect the health of other systems within the human body. For example, periodontal disease may, over time, increase the risk of heart disease and stroke. Periodontal disease is the development of various mixed bacterial infections that affect the soft tissues and bones supporting the teeth. This bacteria is thought to release toxins into the bloodstream that contribute to the formation of fatty plaques in the arteries, which eventually can block blood flow leading to serious health complications such as blood clots that cause strokes (Simple Steps to Better Dental Health, Periodontal Disease). Despite connections like this to the overall health of the body, and the importance of healthy teeth for oral health’s sake, the significance of dental health continues to be marginalized. This neglect of oral health has led to what the Surgeon General has declared as a “silent epidemic” within the United States (U.S. Department of Health and Human Resources, Office of the Surgeon General, 2000). While oral health is important to all people, it is the low socioeconomic status (SES) populations that suffer most from this epidemic. Unfortunately, racial and ethnic minorities, such as African Americans and Latinos are often hit the hardest by this health disparity (Watson et al., 34, 2001). For example, a Washington Post article, in 2007, told the story of a 12-year-old African American boy named 1 Deamonte Driver who died of a toothache. The bacteria from the abscess spread into his brain, eventually killing him. This was a terrible incident and should never have happened because oral disease is easily preventable and can be eradicated through dental procedures. Deamonte came home from school one day complaining of a headache and soon became very sick. He was rushed to the hospital and had an emergency brain surgery. He began to have seizures and underwent another operation and the infected tooth was extracted. Deamonte spent 8 weeks in the hospital before passing away. Deamonte’s Medicaid insurance should have covered dental care, however, Medicaid dentists are extremely difficult to find and at the time of his hospitalization, his insurance had temporarily lapsed. Incidents like this remind us of the importance of oral health and how it is far too often overlooked in health care. Deamonte had a younger brother, named DaShawn, who also suffered from intense oral pain. The Washington Post discusses his story as well. DaShawn had seen a dentist for his ailments; however, the dentist discontinued the treatments because he squirmed too much in the dentist chair. To put into perspective the severity of DaShawn’s ailments, it is important to know that DaShawn had abscessed teeth and his condition was so severe that his mother was so engrossed with getting professional help for his condition that she failed to realize that Deamonte’s teeth were also infected until he was in critical condition. What does this say about the dentist who discontinued treatment with DaShawn because he “squirmed too much?” DaShawn’s condition was not a 2 trivial one, yet the dentist stopped treatment because of being inconvenienced by the child’s behavior in response to pain and fear at the dentist office. How often does this happen? What are the perceptions that dentists have of their patients and how does this effect access to dental care? Do dentists consciously or subconsciously provide differential treatment to different patient populations? No matter what the root reason this dentist discontinued treatment with DaShawn, in his case, the dentist’s unwillingness to endure his squirming caused him to have zero access to dental care because his family was poor and his insurance status fluctuated back and forth from Medicaid to no insurance at all. Because many dentists do not accept Medicaid, his mother struggled for months to find another dentist and had to contact a lawyer from the Baltimore-based Public Justice Center for help in finding one to treat her son (Otto, B01, 2007). By the time she secured an appointment, they had lost their insurance coverage due to poor structuring of the Medicaid system. Situations like this should be further investigated to understand how they contribute to racial and socioeconomic disparities in oral health. Fortunately, not every case of untreated dental disease always leads to death, however Dashawn’s story shows that oral infections can greatly affect the everyday comfort and interactions children experience. A severe toothache is an excruciatingly painful experience. The intense pain caused by untreated oral decay can negatively affect other parts of children’s lives. Dental pain may interfere with concentration at school, affect self-esteem, and lead to a decrease in speech, which can affect speech development. Furthermore, dental decay can 3 interfere with children’s eating habits, thus, affecting the overall health of a growing body, and the child’s energy levels. Oral decay is the single most prevalent chronic infectious disease of childhood (National Maternal & Child Oral Health Resource Center Fact Sheet, 2004). Mexican American children between ages 2 to 5 are more likely than their non-Hispanic white and black peers to experience caries1 in primary teeth (National Maternal & Child Oral Health Resource Center Fact Sheet, 2004). Within California, “one-third of preschool children have untreated tooth decay” (First Smiles Oral Health, 2004). Furthermore, nationally and within Santa Clara County, minority children in the third grade are more likely to have incidents of dental caries than white children (Healthy People 2010, Table 21-1a.). Oral health has become an increasing problem because many dental care providers do not accept public health insurance and therefore underinsured children do not have adequate access to dental health care to prevent and treat oral decay. Furthermore, low SES plays a role in increasing the incidence of dental caries for many of these children because their parents are often not as well versed in promoting preventative oral health care. Unfortunately, the combination of factors influenced by low SES, such as exclusion from professional dental care and lack of knowledge of the importance of preventative 1 Dental caries: cavity formation in teeth caused by bacteria that attach to teeth and form acids in the presence of sucrose, other sugars, and refined starches; tooth decay 4 oral health care, places these children at a greater risk for dental disease. Additionally, these communities often do not realize that they can prevent the majority of oral diseases themselves because so many other factors in their lives seem to present more immediate attention than oral health care. Therefore, it is important that oral health interventions tailored specifically for the communities they intend to serve are initiated to confront and suppress this ‘silent epidemic’. The Health Trust (THT) is a non-profit organization dedicated to addressing these disparities and has implemented a home-based oral health program that uses the Promotores de Salud model (to be elaborated on in the literature review) to combat these inequities. I took a special interest in this program and chose to focus my research on evaluating it. I am specifically interested in understanding if the program addressed barriers that these families face in maintaining their children’s oral health, such as recognizing the importance of brushing and flossing, paying for dental visits, or even finding a dentist. There is a large gap in the literature regarding oral health cultural practices and often the oral health care systems attribute racial and ethnic disparities to cultural practices although little is actually known about these “cultural” practices they reference (Butani et al., 9, 2008). Therefore, I am also interested in what cultural oral health related practices Mexican Americans are accustomed to. It is dangerous to make claims that cultural practices of an already marginalized group led to detrimental oral health outcomes without having the facts to support it. It places the group at risk for further 5 marginalization by stigmatizing the group. By identifying cultural beliefs, values, and practices that influence oral health, we can better identify whether or not Mexican cultural practices actually increase risk of contracting oral disease. If they do contribute to the disparity, it is important to understand exactly how they impact this disparity in order to minimize oral disease incidence in this population. However, if cultural practices do not contribute to the disparity, it is important to continue to seek answers as to why this disparity is so prevalent among Mexican American children. By understanding the mechanisms that contribute to this disparity, we can work to reduce it. Mexican American children carry a disproportionate burden of oral disease. Many of these children are either underinsured or uninsured and face an access barrier to professional dental care services and to preventative oral health practices due to lack of knowledge. Obstacles generated by low socioeconomic conditions compound this issue. Existing literature has not yet identified the barriers at play in this situation in their entirety and therefore, has not been able to identify a sound method to reducing these disparities. THT’s intervention program seeks to address this ‘silent epidemic’ and the information that comes from examining this program’s effectiveness will contribute to understanding the broader picture. The driving questions for this research are: (1) How effective is oral health outreach to low SES Mexican families in addressing barriers parents face in maintaining their children’s oral health? (2) What cultural oral health related practices do Mexican families use to maintain oral health? 6 This paper will examine just how severe this disparity is among the Latino children population, with a focus on Mexican American children, what existing barriers have been identified, and the interventions that seek to address these inequities. The study aims to identify barriers that have been under-addressed and to find out how THT’s intervention can help parents of Mexican descent overcome these barriers. Cultural oral health related practices are of special interest because they have been cited as a contributing barrier to this disparity, yet they are not clearly understood. 7 Literature Review This section provides a background on the nature of oral health disparities among Mexican American children, the interventions that have been initiated to reduce these disparities, and what information is absent from the literature that could help to better understand this phenomenon. This information will provide understanding as to the motivations of this study. An overview of the current state of Latino Oral Health will provide information detailing the extent to which this disparity exists. The identified barriers parents of Mexican descent face in maintaining the oral health of their children are outlined. Existing oral health interventions that aim to address these barriers are discussed. Next, background information on THT and its oral health intervention are presented. Lastly, this section discusses what gaps are in the literature and explains the purpose and motivations of this study in its goal to further explore the barriers contributing to oral health disparities in Mexican American children. Current State of Latino Oral Health The Latino population has become the largest minority group in the country; therefore, research has been conducted to work to identify the health needs of this population. Studies show that Latino children are at a greater risk to have dental caries, untreated oral disease, and decayed and filled tooth surfaces. According to the 1988-1991 Third National Health and Nutrition Examination Survey (NHANES III), 10% of Latino children 8 years of age 8 received sealants2, compared with 29% of non-Hispanic white children (RamosGomez et al., 1232, 2005). Furthermore, “only 60% of 12 to 17 year old Mexican Americans have had their dental caries treated or filled, compared with 87% of 12 to 17 year old white children” (Flores et al., 84, 2002). Mexican American children have strikingly high occurrences of oral disease. This group is especially vulnerable because many of these families have a low SES and even when SES is controlled for, Mexican Americans still experience a high prevalence of oral disease. Research shows that when income was controlled for, 57% of non-poor Mexican American children ages 2-9 suffer from untreated decayed teeth as compared to 37% of same aged non-poor white children (Atchison, 21, 2003). Substantial differences in oral health outcomes persist even when income level is controlled for and these differences become more exacerbated when income level is not controlled for. Interestingly, oral disease is still prevalent when income level is controlled for. This means that families of Mexican descent who are not poor and most likely have oral health insurance or can afford to take their children to the dentist for dental cleanings and dental ailments still experience an oral health disparity. What is the reason for this? There may be other factors aside from being able to afford dental care causing this inequity. From this data it is clear that there is an urgent need to address this disparity, whether it be low SES or higher-income Mexican American children. 2 Sealants: A plastic resin used in dentistry to coat the chewing surfaces of the back teeth to prevent the growth of cavity-causing bacteria 9 Although little is known about how this disparity has manifested itself, practicing preventative oral health can effectively prevent most dental diseases and while many of these families may not be not fully aware of the importance of these practices, oral health education and health promotion programs are viable options for decreasing oral disease (Watson et al., 34, 2001). In order for these programs to have lasting positive effects, it is important that cultural, social, economic and other environmental factors that may influence oral health are considered. Additionally, it is important that community members are recruited as active participants in identifying their community’s health needs. This will promote community ownership of the program, which will lead to sustainability and ensure that the program adequately and appropriately addresses the community needs. Research has shown that interventions in which community participation is valued in the planning and implementation of the program are not only feasible and helpful for building upon existing local resources, but are a great option for addressing oral health concerns in populations that do not necessarily have access to traditional dental care, such as professional services (Watson, 39, 2001). While there is evidence that this specific type of program is effective for teaching oral health care and can possibly work to reduce oral health disparities, it is important to acknowledge that not all Latino communities are the same and each subgroup may require different considerations for designing culturally appropriate service-delivery models (Ramos-Gomez et al., 1238, 2005). Latinos differ in political, cultural, socioeconomic, and geographic aspects – which may 10 include variances in expectations regarding dental care needs, leading to differential access to dental care. Therefore, it is important to unravel exactly how these differences affect oral health. Despite these differences, there is a great disparity among health research literature that addresses the specific subgroups within the Latino population. According to the 2007 Census, the Latino population consists of 64% Mexican Americans, 9% Puerto Ricans, 3.4% Cubans, 3.1% Salvadoran, 2.8% Dominican, and other Latinos make up 17.7% of the U.S. Latino population (2006 American Community Survey, US Census Bureau). This particular study focuses on understanding oral health dynamics in Mexican American children with monolingual Spanish speaking parents, however, this literature review discusses Latino oral health when the subgroup is not specified in the literature. Although it is not clear how differences in subgroups directly affect oral health status, by examining THT’s intervention and the target community, which is primarily made up of Mexican Americans and first and second Mexican immigrants, it may be possible to identify the needs of this specific subgroup. Although a demographic break down of Latino subgroups is not available, as of 2007 25.7 percent of Santa Clara County was made up of Latinos and a large majority of Latinos in this area are of Mexican heritage (U.S. Census Bureau, Santa Clara County, California, 2007). It is important to be aware of the tendency to place all Latino subgroups together and treat them as one homogenous group. This umbrella effect is dangerous because it ignores the unique aspects of each group and could lead to poor assessments of subgroup 11 needs. This study specifically focuses on people with Mexican heritage and Mexican cultural practices and therefore, the findings are not necessarily universal to all Latino populations. While research sometimes simplifies the Latino population as a homogonous group, it lacks richness of information in understanding the mechanisms that contribute to oral health disparities. Little is known about the cause for the current oral health epidemic among Latinos, especially among children, except that there is a great disparity between these children and their white counterparts. It is apparent, however, that early childhood caries is especially prevalent among children of low socioeconomic status, and this includes a large portion of Latino families. Furthermore, these families do not have easy access to professional dental care due to barriers such as lack of dental insurance, dentists who do not accept public dental insurance, possible cultural differences between patient and provider, and lack of parent knowledge of oral health needs (Flores, 196, 1998). It is important to identify all barriers that contribute to this disparity and strive to understand how to overcome these barriers to reduce this largely preventable epidemic. Existing Barriers: What we know Mexican American children are more likely to experience access barriers to dental care than their non-Hispanic white counterparts. Many factors contribute to this disparity. Although many articles note that a full understanding of this 12 phenomenon has not yet been elucidated, literature identifies “acculturation, cultural preferences for sugary beverages, putting infants to sleep with bottles, and mother-child transmission of carries-causing bacteria…lack of insurance, dearth of dentists accepting Medicaid, shortages of Latino dentists, and cultural and linguistic obstacles” as possible explanations for this disparity (Flores, et al., 85, 2002). Most of the barriers contributing to this disparity stem from SES factors, however for the purpose of examining these barriers, they have been divided in to several categories: financial barriers, which involve insurance and ability to pay, cultural and or class differences between the patient and provider, effects of low SES on family behavior, and knowledge and values of oral health. Many Mexican American children either do not have dental insurance or are on public health insurance such as Medicaid – these are considered financial barriers to dental services. As mentioned previously, many dentists do not accept Medicaid and even fewer of them are pediatric dentists. In fact, nearly 75 percent of dentists do not participate in the Medicaid program and therefore do not accept Medicaid-insured patients (Haden et al, 566, 2003). Reasons dentists have such low Medicaid participation include inadequate reimbursement funds, slow disbursement of Medicaid payments, arbitrary denials, prior authorization requirements for routine services, and many non-pediatric dentists are unwilling to treat young children (Inspector General Brown, 7, 1996 and Gehshan et al. 5, 2008). The low number of dentists willing to treat children and/or accept Medicaid complicates this financial barrier of access to dental care. Furthermore, children from immigrant Mexican and Mexican American families with 13 monolingual Spanish speaking parents are at even more of a disadvantage because they may have a difficult time finding a dentist who speaks Spanish. Although Medicaid has existed for many years, the implementers have not found a way to address these persistent issues regarding the difficulties dentists face in participating in public health insurance. Public policymakers often do not value oral health as much as general health and therefore marginalize it to a lower priority (Haden et al., 566, 2003). This is a substantial institutional factor that contributes to this disparity. Another barrier that involves institutional factors are cultural and/or class differences between patients and dentists. It is considered an institutional factor because the dental system is set in place to serve its patients, and dentists are paid to provide a service to them. Dental schools are expected to prepare their students to serve the United States and it is made up of a diverse population with many different cultures and classes, therefore, they should be prepared to serve patients from various backgrounds. The majority of the dental workforce does not possess cultural humility in their care practices for racially and ethnically diverse populations or even to the very young (Haden et al, 566, 2003). Therefore, the dental system, including dental schools, should work to prepare dentists to seek cultural humility in order to accommodate patient differences to ensure equal quality care. One study found that parents experienced a lack of concern or respect from dentists when they took their children for a dental check up. This caused the parents to question the quality of care the dentist was providing (Riportella-Muller et al. 1996, 76). This could be due to dentist-patient 14 cultural differences and perceptions that the dentist has of the parents due to SES or ethnic background as this trend has been identified in the medical field between physicians and patients (Smedley et al. 2003). The problem does not only stem from institutional factors, barriers due to low SES of the child’s family also contribute to the disparity. The following are barriers that stem from the effects low SES has on family behavior, such as motivation and ability to maintain children’s oral health. Families living in poor inner cities or even rural areas have difficulty getting time off from work to take their child to the dentist. Finding transportation, especially if the dentist is a long distance away, poses as a barrier as well. Furthermore, these families have a lot to deal with in terms of other medical health needs, bills, jobs, daycare, etc. and can overlook the importance of oral health, especially if they are not aware of the significant role it plays in their child’s overall health. Many low SES families give dental services low priority because they have many other competing family priorities. This causes parents not to seek services for dental care (Riportella-Muller et al. 1996, 71-76). Oral health is often neglected and is not considered an important part of overall health by the general population. This lack of knowledge and value of oral health acts as another barrier. This group includes, but is not limited to, many immigrant Mexican and Mexican American families unaware of its importance and the practices that can be done to prevent oral decay. This means that there is a “lack of knowledge about the prevention of oral health diseases and awareness of their clinical need” (Haden et al., 566, 2003). This 15 lack of knowledge could be exacerbated in communities of need because there are so many other stressors present due to socioeconomic conditions. Often, research attributes the lack of knowledge of oral health practices and high prevalence of oral disease in immigrant Mexican and Mexican American children to oral health related cultural practices (Flores et al., 85, 2002). However, little is known about exactly what oral health-related cultural practices are and how they contribute to increased prevalence of oral disease in children. Independent of SES, Mexican American children have high incidence of oral disease. Data previously presented shows that when SES is controlled for, Mexican American children still have higher incidences of untreated caries over their non-hispanic white counterparts. Several studies show that “the percentage of children who had never visited a dentist was highest among Mexican children (17.7%)” and have had the lowest levels of dental visits in the United States (Ramos-Gomez et al., 1232, 2005). This suggests that Mexican American children are more likely to experience access barriers to dental care compared to non-Hispanic white children. Literature has not clearly elucidated the reasons why Mexican American children, in particular, experience this barrier. No matter where this barrier stems from, it is clear that other factors outside of SES contribute to oral health disparities in this population. Existing Interventions As described previously, oral disease is very prevalent among Latino children, especially those living in low socioeconomic conditions. Interventions 16 and government programs have been initiated to combat this inequity, however, this problem has persisted for the past 3 decades (CDC, 293, 2007). This section discusses existing oral health interventions that target low socioeconomic communities and seek to improve public health. These include government funded public health programs and non-profit organized interventions. There are many different methods and structures of community interventions. Examples include school-based programs that provide health education, fluoride rinse and tablets, and/or oral examinations and referral, programs that prevent early childhood caries, and public, professional, and school-based education (CDCMMWR, 3, 2001). These programs may be run by dentists or other dental professionals and generally take the traditional approach to interventions. This approach involves a public health expert doing research to assess the community need, developing an intervention, and implementing it in the target community. There is little to no collaboration with the community in developing and executing the intervention. Medicaid’s oral health program, a community based participatory research (CBPR) intervention, and THT’s home-based oral health program will be discussed in greater detail. Medicaid is a program that provides insurance to low SES children and therefore has the potential to have a major impact on oral health disparities, whereas other programs lack the power of the government to offer substantial material aid to a large population. The CBPR intervention is focused on because it aims to address the issue in a comprehensive manner by addressing power dynamics and working to empower the community it serves. 17 Lastly, THT’s program is the focus of this paper because it seeks to tailor the program to a specific community by making it a home-based program that comes to the community and has a community member disseminate the information, and therefore, it has similar elements of CBPR. Furthermore, it provides a vehicle to examine the existing barriers present in this particular community. In 1967, Congress enacted Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) dental services program, which was intended to be a comprehensive health program that would provide initial, periodic, and medically necessary follow-up examinations in an effort to remove financial barriers to health for poor children. It has expanded substantially since its enactment. This program included dental care and was to be provided to eligible children from birth to age 20 (Inspector General Brown 1996:1). EPSDT has two primary operational premises, access and utilization. The EPSDT requirements encompass both coverage and arranging for care. The benefits required under EPSDT include preventive dental care, as well as all dental care that is medically necessary to restore teeth and maintain dental health (including orthodontics), as well as assistance in arranging for covered services, including scheduling and transportation. Gehshan et al. 2008:4 This means that the program planned to actively conduct outreach services through mailing, pamphlets, phone calls, and home visits to raise awareness of EPSDT. Furthermore, it is required to provide transportation for families to their appointments, health education for parents regarding normal growth and development of their child, immunizations, and assistance in making 18 appointments. All of this is ‘free of charge’ as long as you qualify for Medicaid (Riportella-Muller et al. 1996:71-72). This program undoubtedly has great potential to reduce health and oral health disparities among poor children, however, over 40 years into the implementation of the program roughly two-thirds of all children on public health insurance had not visited the dentist in the last year (Gehshan et al. 2008:5). Program participation varies from state to state. In 1993, less than 30% participated in three-fourths of the States, and no State provided care to more than 50% of qualifying children (Inspector General Brown 1996:6). Even though the program is having significantly low participation, it has been continued for almost a half of a century. Revisions to the EPSDT program have been made (i.e. Omnibus Budget Reconciliation Acts of 1989 and 1990), yet the program continues to have discouraging participation outcomes. Why does the EPSDT program have such low participation after being active for over 40 years? Let’s examine some of the limits and pitfalls of the program to understand why so few eligible children actually receive preventative dental services. One primary reason why EPSDT candidates do not receive oral health care is because a small number of dentists actually participate in Medicaid. Specifically, “approximately 80% of the States attribute the low utilization rate to a shortage of dentists willing to accept Medicaid” (Inspector General Brown 1996:7). Why do so few dentists accept public health insurance? Many dentists do not participate in Medicaid because it has such low payment rates that dentists end up losing money by serving these patients. What's more, Medicaid 19 is set up in such a way that the administrative requirements are complex and laborious to complete. These issues detour dentists from committing to the Medicaid insurance system, thus Medicaid insured children have a difficult time finding dentists who will serve them. (Inspector General Brown 1996:7 and Gehshan et al. 2008:5). Although the program has existed for many years, the implementers have not found a way to address these persistent issues. Additionally, many children who qualify for Medicaid are from minority groups, including Mexican American children. This means that the program should have created strategies to make it a program that includes cultural humility3, however, the program does not emphasize this important factor in outreach strategies. EPSDT also failed to provide the transportation and assistance promised to participants, creating more barriers to accessing a dentist. Many Mexican families live in rural areas and traveling 15 miles to the dentist without a means of transportation can make it almost impossible to seek dental care when these families have many other pressing issues to deal with (Riportella-Muller et al., 78 1996). Limited clinic hours and loss of Medicaid eligibility after making an appointment, further disrupts access to dental care (Riportella-Muller et al., 75, 1996). These logistical barriers have persisted and must be addressed. Furthermore, the EPSDT outreach needs to be altered to better inform parents of 3 Cultural humility is distinct from the more commonly used term, cultural competence, a competence that may never be truly achievable in another culture. Cultural humility refers to ‘a lifelong commitment to self-evaluation and self-critique’ to redress power imbalances and ‘develop and maintain mutually respectful and dynamic partnerships with communities’” (Wallerstein and Duran, 316, 2006) 20 preventative measures they can take to maintain their children’s oral health, and on the importance of receiving dental care. While EPSDT has many areas that need improvement, the program has the potential to have a substantial impact on oral health disparities because it provides financial support for professional dental care on a national level. A relatively new form of research developed in the public health field known as Community Based Participatory Research (CBPR) has emerged in the past few decades to reduce health disparities. CBPR addresses social, structural and physical environmental inequities through actively involving organizational representatives, community members, and researchers in every aspect of the research process. It uniquely integrates social action, education, and research strategies to reduce health disparities and improve health. This form of research focuses on fostering a trusting relationship between the community and outside researchers. A fundamental element of CBPR is the significance of the participation and impact of nonacademic researchers in the process of attaining knowledge and understanding the social phenomenon being studied. In CBPR, each partner “contribute[s] ‘unique strengths and shared responsibilities’ to enhance understanding of a given phenomenon and the social and cultural dynamics of the community, and integrate the knowledge gained with action to improve the health and well-being of community members” (Israel et al., 177, 1998). This is unique from other forms of health interventions, which place the majority of control over the project in the hands of public health researchers who are considered the health ‘experts’. The community itself is 21 acknowledged as a unit of identity with irreplaceable expertise in terms of knowledge of the structure of the community, what the community needs, and how to best address that need. The outside research team is equipped with expertise in terms of research techniques and resources that may not be readily available within the community. CBPR principles stress that the research team, recognizing the community as a unit of identity, builds on existing resources and strengths within the community, involves a cyclical and iterative process, and promote co-learning and empowerment between the research team and the community (Israel, et al., 1998). Many interventions are adopting this method when working with communities because it is believed that CBPR “enhances the relevance, usefulness, and use of the research data by all partners involved,” brings together partners with a variety of skills and knowledge to address complicated problems, “strengthens the research and program development capacity of the partners,” aims to enhance the well-being and health of communities involved by directly focusing on identified needs and indirectly by giving them more control and power over the research process. (Israel, et al. 181, 1998). Within the field of oral health, there have been limited applications of CBPR in reducing oral disease among at-risk populations. Most oral diseases are preventable without the assistance of dental professionals; oral health is one realm of health that individuals themselves can greatly control when given correct information on how to prevent oral disease. However, many high-risk populations are not aware that most oral diseases can be prevented and controlled through preventative 22 practices such as daily brushing and flossing. Therefore, the CBPR model is a particularly good fit for oral health interventions because it focuses on getting the community members involved and once the information is disseminated, the community has a great potential to sustain outcomes of the intervention themselves. This aspect is especially important now, when funding for community interventions are low and funding for professional dental care is difficult to accrue. One such initiative focused on an inner-city Latino community, primarily of Central American descent located in Mount Pleasant, a neighborhood in Washington, DC. The intervention was a pilot project with the purpose of investigating the feasibility of creating and implementing an oral health community participatory program framework in conjunction with the PRECEDEPROCEED model (Watson et al., 35, 2001). The program focused on early prevention of caries by targeting parents of children of pre-school age and pregnant mothers. The program fulfilled eight CBPR principles. Specifically, the initiative tailored the approach to the specific target population by taking into account the identity of the community. Existing resources within the community were built on, and collaborative partnerships from members of the community were fostered throughout the entire project. This approach facilitated mutual benefit for all partners involved and promoted co-learning, integrated knowledge and action, and community empowerment. The program also strived to engage in a cyclical and iterative framework by constantly fine-tuning the program and approaching oral health with the comprehensive lens of overall well-being. 23 Additionally, the program disseminated the findings and outcomes to the community. The CBPR approach employed in this pilot program provided a useful foundation in addressing the oral health disparities in Mount Pleasant and delivering greatly needed oral health advice from dental care professionals to a community with minimal access to traditional dental care. Not only was the CBPR approach feasible, but it was also useful in building on existing local resources and increasing interested and awareness of oral health disparities and the importance of preventative oral health care. Workers in community-based organizations recognized the importance of oral health and were motivated to go beyond their normal boundaries to work with others and get involved in oral health prevention-related activities (i.e. serving as health promoters). The program instigated lasting effects such as local community and religious centers hiring part-time dental hygienists who promote oral health education and apply sealants and fluorides, incorporating oral health screening in medical well-baby visit forms, including oral health information in teen-promoters training program manuals. These small changes on the micro-level may result in large benefits in the macro-level, however, at the time of publication of the results of the program, the long-term effects could not be evaluated yet. Although this initiative was able to recruit local dentists, community representatives of community-based organizations, and health educators, it was not as successful in involving lay community members in the steering committee, which assisted in program planning, implementation, and evaluation. Other 24 limitations of the program were that implementers were not able to utilize a rigorous process evaluation. A third intervention is the subject of this research. The Health Trust (THT) is a nonprofit foundation dedicated to reducing health disparities among communities of color and has launched one such initiative that serves Latino communities in Santa Clara County. In an effort to counteract growing disparities, The Health Trust started several oral health promotion initiatives such as its partnership with The Children’s Dental Group to open a Children’s Dental Center in East San Jose that accepts public health insurance companies such as Denti-Cal. Another initiative they began was the Home-Based Oral Health Education Program in which lay oral health educators visit local families in their homes and advise them of how to prevent oral disease, inform them of the importance of oral health, as well as provide them with resources to help them access professional oral health care. THT adopted the Promotores(as) de Salud model for the intervention. This model recruits lay community members, called Promotores(as), who become trained in a specific health topic and advocate health in their own communities. They are unique social workers that provide a link between their communities and health care services. Promotores(as) have knowledge of their specific community’s needs and integrate information on health and health services into their community in a culturally appropriate and comprehensive manner. Furthermore, their expertise in understanding their community helps to make health care systems more responsive to these communities because 25 Promotores(as) can give feedback to medical systems on what is effective in improving health in the community and what is not. Specifically for this intervention, THT conducted research to assess the need for an oral health intervention and to identify which communities were at the greatest risk of oral disease. The results of this research led to a 5-year grant from the Knight Foundation to “provide oral health education and preventative, restorative and specialty dental services to 3,750 medically underserved children and families in the Mayfair, Seven Trees/Solari and Gilroy neighborhoods of San Jose” in December 2003. The Health Trust planned to collaborate with local agencies already serving those communities with the goal of meeting the requirements stipulated by the grant objectives. Eventually the collaborative fell apart and THT assumed the major role in achieving the goal of the grant. As the program progressed, the Knight Foundation awarded THT with another grant to evaluate the program for the last three years (2005-2008). The program strategy used the Promotores(as) model and the THT staff recruited “Hosts”, community members who volunteered to host an oral health meeting in their home, and recruited family and friends to attend. Promotores(as) were trained to recruit Hosts and lead the Home Meetings and in the fourth year of the program pre and post tests were administered during the Home Meetings. Unfortunately, the ideal structure of the program was not able to be perfectly executed and THT staff was unable to develop and recruit Promotores(as) in Mayfair and Gilroy and therefore, THT staff administered the Home Meetings up until 2008. Another important note is that a standard 26 curriculum was not developed until the fourth year of the program because initially, the home-based meetings were participant and discussion driven and therefore the discussion leader focused on oral health issues of interest to the group. THT initial program plan captured many CBPR principles, such as working with existing community agencies, in an effort to build on the strengths of established resources. The Promotores(as) model de Salud utilizes working with community leaders to draw on the skills from the non-profit organization personnel along with the community leader’s skills. The main item that differentiates THT’s program from CBPR is that THT’s program does not define itself as a research project, but rather an intervention with the main objective of disseminating knowledge about preventative oral health practices, rather than collecting and analyzing data, and then adapting an intervention. However, it is important to note that research was executed to assess the oral health need of the target community. Existing Barriers: What we want to know While these identified barriers may all play a role in this oral health disparity, the internal barriers are often emphasized, which focus on the actions of the community and therefore, place a large degree of fault on the marginalized group. In fact, most papers mention Latino cultural practices as a primary reason for this disparity even though little research has been done to examine exactly how cultural oral health-related practices contribute to this overwhelming inequity (Butani, et al., 8, 2008). If it is not clear why this disparity exists, and has existed 27 for nearly three decades, why does the literature so frequently point to Latino cultural oral health-related practices as the cause for oral health disparities? What is the definition of cultural practices that this literature is working from? Although most articles do not define cultural practices that contribute to oral health disparities, a comprehensive definition that could be used to examine oral health and culture includes five domains of cultural information: 1) General beliefs about health, 2) diet, 3) beliefs about teeth and oral cavities, 4) helpseeking for oral conditions (i.e. traditional home remedies, going to the dentist), 5) oral hygiene practices (Butani, et al., 9, 2008). It is possible that cultural oral health-related practices may contribute to oral health disparities, but it is imperative that quality research is conducted to confirm this assumption, rather than making inferences about a particular group’s cultural values of oral health. This can only further marginalize an already underserved population. In addition, if improvement in the oral health status of Latinos is to be achieved, understanding exactly what these cultural oral healthrelated practices are is the first step. If it is not known what the cultural practices are in the first place, it is impossible to understand how they contribute to this disparity. More research has been done on understanding racial/ethnic health disparities than on understanding oral health racial/ethnic disparities. Mechanisms of the pathway for these disparities have been proposed and often, the role the medical system and physician play have been linked with contributing to health disparities, however there is little – if any – oral health 28 literature that points to dentists’ interactions with patients as playing a role in the low oral health status of Latino populations (and other racial groups for that matter). Research should be done to examine what external factors, such as dentist’s perceptions and treatment of Latino patients, contribute to this disparity. What causes might be contributing to the fact that Mexican American children have had the lowest dental visits in the U.S. this past year. What are the untold perspectives of parents of Mexican decent in regards to maintaining their children’s oral health? It is apparent that Mexican American children are at a greater risk of contracting oral disease than all other children. There are existing interventions in place working to reduce these barriers, but there is substantial information missing from literature regarding the mechanisms that contribute to this phenomenon. While some barriers have been identified; for example, low SES effects the ability to get professional dental care and can make it difficult to maintain good oral health, other barriers, such as cultural practice barriers, have been identified as contributing to the disparity without adequate evidence. This study aims to examine the effectiveness of oral health outreach to low SES Mexican families in addressing barriers parents face in maintaining their children’s oral health and how these barriers can be addressed. Additionally, this study seeks to help identify Mexican cultural oral health related practices used to maintain oral health and what role they play in oral health disparities in Mexican American children. 29 Methodology This project involves a combination of quantitative and qualitative data collection. The Health Trust conducted an internal evaluation through phone surveys and I conducted focus groups to collect qualitative data. Utilizing both types of data collection provides a well-rounded picture of the impact of the oral health program and the perceptions of the participants. For the purposes of this paper, the quantitative data from THT will serve predominantly as supporting data, while the focus group results will serve as the heart of this research project. In current social and behavioral research, mixed methods are being used extensively to answer practical research questions. “A major advantage of mixed methods research is that it enables the researcher to simultaneously answer confirmatory and exploratory questions, and therefore verify and generate theory in the same study” (Tashakkori and Teddlie, 15, 2002). This research methodology uses THT’s quantitative phone survey data as preliminary data to guide the formation of focus group questions. In this case, the focus groups are used to help interpret results from the phone survey (Krueger and Casey, 13, 2009). The qualitative data from the focus groups provides information to inform the phone survey results and also explores new topics not addressed in the phone survey. Specifically, the focus groups examine cultural practices, which could not be easily addressed in the phone survey. Quantitative Data Collection 30 The phone survey was administered by THT, however, for the purposes of my project, I was able to include four questions in the survey. THT’s motivation for this evaluation was to collect evidence of the outcomes of the program to the funder (The Knight Foundation), and provided information for future program development. THT identified five main evaluation questions to address (Reedy, 4, 2009): 1. To what extent did the oral health home-based education influence participants’ children’s access to and utilization of dental care? 2. To what extent did the oral health home-based education program influence participants’ children’s oral health knowledge and practices? 3. What are the participants’ perceptions about home-based health education? 4. What are the parents’ perceptions about the quality of the health educator? 5. What are the parents’ interests in future home-based health education opportunities? The phone survey was first created in English and was then translated into Spanish because most participants are English learners. The survey was pilot tested with three Promotores(as) (community health lay workers) who participated in the home meetings. Adjustments were made according to their suggestions (see Appendix A.1 and A.2 for the survey instrument in English and Spanish). 31 THT’s initial goal was to collect responses from 100 participants from each of the three years of the program to total 300 responses. The final total was 168 respondents: 20 from year 1 (2006), 40 from year 2 (2007), and 108 from year 3 (2008). The reason for low numbers in years 1 and 2 was largely due to disconnected or out-of-service home and cell phone numbers. All but 5 respondents reached agreed to participate in the survey (for an acceptance rate of 97%). Data from the phone survey was collected from November to December 2008 and the Promotores(as) who conducted the Home Meetings made the calls. A subsection of the sample (n=32) completed the surveys in person during a home visit. All surveys were administered in Spanish. THT descriptive statistics and regression analysis for quantitative survey measures and thematic analysis for narrative survey items were used for data analysis. Qualitative Data Collection For this study, focus groups were chosen as an ideal research method because the project is looking for a range of ideas/feelings from immigrant Mexican and Mexican American parents on how the program could better address barriers they face related to maintaining their children’s oral health and how the program could address these issues better. Furthermore, as discussed previously, there is a gap in literature regarding the cultural oral health related practices of Latino families. Focus groups create space for a wide range of input from participants on this topic. This is particularly helpful since there is little 32 groundwork on cultural practices/factors that could influence the current status of Latino oral health. The results from the focus group can help guide future studies such as survey research. The purpose of a focus group is to gather a wide range of opinions between a group of people who have certain characteristics in common that relate to the focus group topic – in this case, having participated in the homebased oral health program. To prevent limiting of ideas, participants are encouraged to contribute a wide array of opinions and avoid conforming to a consensus. The group must be small enough for everyone to have the opportunity to share their insight, between 5 to 10 participants. This is a more natural environment than a one-on-one interview because participants are influencing and are influenced by other participants – as in real life situations (Krueger and Casey, 6, 2009). Questions must be open-ended and unguided to be effective. They are carefully crafted and sequenced after much consideration and feedback. The questions begin with general ideas on the topic and progress to more specific ideas and are usually more useful to the researcher. The facilitator and research focuses on emotions, comments, and thought processes of the participants. The motivation of focus groups is to help researchers, community leaders, and organization leaders make informed decisions about a service, product or opportunity. Decisions are not made during the focus group by the participants, but after analysis and understanding the range of perspectives on an issue. The 33 focus groups for this research are meant to help understand the effectiveness of a program and are considered a feedback or outcome evaluation because they are used to guide decision making for further program development (Krueger, Casey, 2-13, 2009). The aim of this study is to reveal barriers that influence behavior and inhibit parents of Mexican heritage from maintaining the oral health of their children. Focus groups are particularly useful in this case because they promote an emergence of ideas from the group. This means that the group provides more than just the sum of parts, but rather presents concepts that evolve past what an individual can alone present. The information collected from this qualitative research will contribute to the literature on an under-examined topic and will provide more detail on the effectiveness of the home-based oral health program, complimenting the quantitative data collected by THT. Preparation for focus groups began in early November to prepare to submit the focus group questions and the research protocol to the Institutional Review Board by the beginning of January. The development of the questions took a cyclical path and revisions were made several times before piloting the questions and submitting them after making final adjustments. In total, 15 questions were submitted to the IRB, however, before the actual focus groups 3 questions that were considered to be unnecessary and/or redundant were excluded (see Appendix B.1 and B.2 for English and Spanish versions). Two focus groups were organized and a $25 gift card for Target was supplied by THT as an incentive to recruit participants. 34 The majority of participants were first or second generation immigrants from Mexico and therefore, two moderators were hired to lead focus groups in Spanish. Two research assistants were also hired to take notes during the focus groups, watch the participant’s children, and transcribe and translate the audio from the sessions. This process included working with THT to locate moderators and interviewing Stanford students who are native Spanish speakers for research assistant positions. The obligations of the moderators were to recruit participants, moderate focus groups, take notes and observations, and debrief after the sessions. The obligations of the research assistants were to translate all documents necessary for focus group sessions, watch over the participant’s children during focus groups, facilitate setting up the focus group sessions, take notes during focus groups, debrief after sessions, and transcribe and translate audio data. Research assistants were instructed to translate documents as close to the English version as possible while maintaining the general feel of the questions. There was an emphasis on using short words and short sentences to keep the questions jargon-free and easy to understand. In order to pay these individuals and fund this project I applied for and received a grant from Stanford Undergraduate Research. One of the moderators helped to locate and reserve a location (St. Maria Goretti Church in San Jose) for Friday, February 20, 2009. Both focus groups were held on the same day with two moderators, one leading discussion and the other taking notes, and one assistant recording observations. Childcare services were offered for focus group participants and one of the assistants watched the 35 children in the other room. I planned to remain in the room during the focus groups to observe the dynamics of the discussion, however, due to unexpected circumstances, was only present in the room during the first focus group and was supervising the participant’s children during the second focus group. THT’s moderators conducted the recruiting process of the participants. Initially, each focus group was supposed to have 8 participants for each focus group, for a total of 16 participants. THT advised moderators to recruit 12 participants for each focus group because some participants may choose not to show up. During the recruitment process, initially it was confirmed that there would be 12 in the first focus group and 8 in the second focus group. However, in actuality, the focus groups had 8 participants for the first session and 11 for the second session. Four participants did not show up to the first session and the evening before the focus groups, another Health Trust employee made phone calls to recruit more participants for the second group, which increased the number to 11. The focus group staff debriefed on how the sessions went overall and mentioned any interesting comments/observations they made after the focus group sessions were completed. The sessions were audio recorded and loaded onto a computer to be transcribed and translated by the research assistant. After focus group data was transcribed and translated, a transcript-based analysis was conducted. Because this study had only two focus groups, a classical analysis strategy was utilized (Krueger and Casey, 118, 2009). Themes 36 and categories that emerged from the data were identified by systematically reading through the transcripts, identifying if the participant answered the question and grouping responses accordingly. Once participant answers were sorted into categories, comments that were expressed frequently, revealed a nuanced idea, were specific and provided detail, comments where participants showed emotion, and extensiveness4 were given more weight and attention. The results were structured around themes rather than around the focus group questions. Limitations While focus groups were an appropriate data collection method for the purposes of this research project, there are limitations to this study. One of the most difficult parts of conducting the primary research for this project has been that the focus groups had to be in Spanish, which created an element of separation between the data and myself. This issue became especially prevalent when reading through the transcripts because I had given directions that were not adhered to as closely as I would have preferred. Furthermore, because the moderators were not involved in developing the questions, it made it difficult for them to know when to probe further and when to push the conversation along. The majority of the limitations stem from this distance between the primary researcher and the data collection process. “Extensiveness is how many different people said something.” It is different than frequency, which is how many times something is said (Krueger and Casey, 122, 2009). 4 37 Some focus group responses were trivial and did not provide depth on the issue. These short one-worded answers were especially prevalent when participants were asked about cultural oral health related practices they used in their country of origin. In order to understand more about the cultural practices mentioned in the focus group, it was necessary to do additional research using Internet search engines, such as Google Scholar, on the hygiene and ailment remedies participants mentioned. During the first focus group, the research assistant noted that one individual in particular tended to dominate the focus group and could have therefore influenced results. Moderators did their best to suppress this effect to ensure that all participants could reflect on the questions without feeling pressure to conform to the individual’s ideas. After the first focus group, the moderators mentioned that participants had trouble understanding the language used in one of the questions. This question was part of the key questions and therefore, this may have stifled some of participants’ responses. In order to avoid this very situation the research assistants were asked to proofread each other’s translated documents to make sure they maintained the jargon-free format of the English version. However, this problem still occurred. This is another limitation that emerged due to conducting research in a different language than the researcher’s because it was impossible to have complete control over the focus groups and therefore made it difficult to personally check every document before the focus group sessions. 38 Although participants were informed that no THT staff involved in the home-based oral health program were present at the focus group sessions and were therefore told to be completely honest about how they felt about the program, it is possible that participants did not give completely honest opinions about the program due to feeling pressure to please moderators. Sometimes, focus groups make it difficult to tap into emotions to find reasons driving behavior (Krueger and Casey, 13, 2009). In this case, parent and child behavior in maintaining oral health was the focus. Individuals may not be aware of the emotions that influence their behavior and even if participants were aware, these emotions may be considered private and therefore individuals may be disinclined to share them with a group. To draw out emotions behind behavior the moderator must ask questions about feelings. Furthermore, if participants feel comfortable with the moderator and other participants they are more likely to be willing to share their emotions. The moderators were of Mexican descent and did their best to make participants feel comfortable. As mentioned previously in this section, I was not able to be physically present during the second focus group because one of the research assistants failed to be present during the second focus group. Therefore, there was no one to supervise the participant’s children except for myself. This was unfortunate, however, the research assistant present made sure to pay special attention to body language and expressions in her observation notes and took time to discuss them with me in detail. 39 Due to resource and time limitations, it was not possible to conduct more than two focus groups, although three or more are cited in the literature as the ideal amount (Krueger and Casey, 21, 2009). Although only two focus groups were conducted, there is relatively little literature on how interventions aid immigrant Mexican and Mexican American parents in overcoming barriers in maintaining their children’s oral health. Furthermore, there is even less information identifying cultural oral health related practices and how they contribute to oral health disparities among Mexican American populations. Therefore, this research provides more information on what the barriers are and how culture influences (or does not influence) oral health outcomes. 40 Results The THT’s phone survey data in general suggests an increase in positive oral health practices for the respondents (n= 168) after participating in the homebased oral health program. Participants appreciated the home-based program style and the Promotores(as), showed increased knowledge and awareness of the importance of oral health, and improved their dental practices among families. The findings from the phone survey will be discussed along with the results of the focus group study (See Appendix C for phone survey data). A total of 19 people participated in the study: 16 women and 3 men of Mexican decent with the mean age of 38.7 years old. Two participants, one male and one female did not disclose their age. All participants’ primary language was Spanish and the focus groups were conducted in Spanish. Predetermined eligible participant criteria included: having participated in the program within the past two years (2007-2008), having at least one child between the ages of 2-12, and participation of only one parent from a household. The criteria was met except: one 58-year-old female participant did not have a child aged 2-12, however she was a grandmother of children between the ages of 2-12, and due to an unexpected miscommunication, a married couple participated. THT home-based oral health program was initiated in three areas: Mayfair, Seven Trees, and Gilroy. The participants in this study lived either in Seven Trees or Mayfair where there is a large population of first and second-generation Mexican immigrants. 41 Therefore, being Mexican is a very salient part of their cultural identity so I will use the terms Mexican and Mexican-American interchangeably. The three locations were identified as low SES communities in need of oral health education by a dental needs assessment report conducted by THT. The report identified these neighborhoods as low SES and most individuals, if not all are at or below the federal poverty level ($1,200 a year/individual). The focus group data was analyzed using the classical analysis strategy as defined in Krueger and Casey, 4th edition Focus Groups: A Practical Guide for Applied Research. Participant statements were systematically organized into themes that emerged from the data and placed into code categories. Analysis of data shows that overall, participants felt that THT program was successful. Perceptions of THT program were positive and participants displayed thorough knowledge of positive oral health practices. Several different themes and code categories emerged regarding perceptions of THT’s program. The following describes the code categories that emerged from focus group data and refers to quantitative findings from phone surveys when appropriate. Community engaging: the program was described in the focus groups as engaging with community members for several reasons. The program came to community member’s homes, which gave participants a sense of comfort because they could learn about oral health in the comfort of their own neighborhood or home. Participants liked that children and parents participated in the program together to learn about the importance of oral health. The Promotores(as) (health educators), are members of the community and 42 therefore participants felt especially connected to the program. The phone survey found that more than one-third (n=55) of the participants appreciated the teaching approach of the Promotores(as) and home venue of the program. Participants appreciated that people from their own community and ethnicity led the oral health discussions. This statement illustrates this idea of comfort and trust that program participants felt: Well for a while I had an impression of comfort. They go to your home, you feel comfortable, you don’t have to go out or anything. That was an impression of community and comfort. And, well, the people can be confided in, they are from the community. - Mother Program provided helpful incentives: Focus group participants appreciated receiving toothbrushes as gifts after participating in the program. Phone survey results also show that participants found this as a positive aspect of the program (n=12). Comprehensive Curriculum: Phone survey data showed that participants recalled knowledge about brushing (89.1%), flossing (63.8%), healthy eating (43.1%), communication with dentist (38.5%), and seeing a dentist every six months (3.5%). Focus group participants supported these findings. Information provided to participants was considered to be comprehensive because participants showed thorough knowledge of why oral health is important, good oral health practices, healthy eating, and knowledge of the importance of visiting a dentist twice a year. Participants were knowledgeable about poor oral health practices and why they are damaging to teeth. 43 Ways to Improve: While the program provided thorough information on preventative practices and why oral health is important, focus group participants voiced more information on the need to know how to find affordable dental services for their children, especially if they do not have dental insurance. Phone survey results show that only 54 percent of the participants reported having taken their childe to the dentist in the past six months. It is not clear from the survey whether or not the program influenced participants to take their children for a dental visit or if this is an increase from before the program. Participants also felt that the program could target the adults as well in order to help them find more affordable dental care. This statement captures suggestions for improvement: Well, I think that I would add that if a family doesn’t have a medical insurance, then the information needs to be given to them to help them find… services. - Mother Statements falling into code categories for perceptions of THT’s program occurred with the following frequency: community engaging (5), impressions (2), program provided helpful incentives (1), ways to improve (4), and a comprehensive curriculum. Within the comprehensive category, the content surrounded three basic areas: knowledge of oral health practices, knowledge of healthy eating, and knowledge of professional dental care. Within the knowledge of oral health practices, the frequencies of statements are given: correct brushing (19) and correct flossing (8). The occurrence of responses regarding the other topics follows: knowledge of healthy eating (10) and 44 knowledge of professional dental care (6). Figure 1 provides the layout of code categories for perceptions of THT’s home-based oral health program. Figure 1: Code Categories for Perceptions of THT This figure displays the code categories identified from focus group discussions regarding participants’ perceptions of THT. The comprehensive curriculum code category has three subcategories that emerged from the data as shown in the figure. Furthermore, according to self-reports from focus groups, oral health behavior and attitudes improved for participants after participating in the program. The following describes the code categories for oral health practices of participants before and after the program: 45 Oral Health Behavior Pre-Program: Before participating in the program participants did not focus on incorporating oral health care into the routine of their children’s lives. Practices varied between not brushing at all and periodic brushing, sometimes with toothpaste, and sometimes without. Some parents noted that “in reality, they didn’t do anything,” while others mentioned that they “where brushing teeth in the wrong way.” Oral Health Behavior Post-Program: Participants discussed how they began to incorporate oral health practices into their children’s daily routines after participating in the program. They also made statements about how their children would be concerned about eating healthy and brushing their teeth because it became more important to them. For example, one mother said that “the kids they say, ‘mommy, I have to brush my teeth,’ and I tell them, ‘well I also have too.’ Now it is a routine.” Phone survey data supports these findings showing that 74 percent of participants revealed that after participating in the home-based oral health program, their children’s frequency of brushing increased. Frequency of flossing, however, showed only a 56% increase. In fact, phone survey results show that nearly one out of four participants’ children never floss. Attitude Change Post-Program: Parents expressed ultimately feeling happier about oral health after participating in the program because they knew the importance of it and learned good oral health practices. Also, they felt that they now knew how to prevent their children from experiencing pain from toothaches. Oral health became as important to participants as general health. 46 Parents also mentioned a change in children’s attitude after participating in the program and “they began to take more responsibility in taking care of their teeth.” Children were more eager to brush their teeth and had better selfesteem knowing that they were keeping their teeth healthy and white. Participant statements about oral health practices before participating in the program (oral health behavior pre-program) emerged 6 times. Frequency of comments on oral health behavior change occurred in both children (15) and adults (14). Comments regarding attitude change towards oral health appeared 11 times for children and 10 times for adults. Statements regarding behavior before partaking in the program emerged 6 times. Figure 2 shows the code categories that emerged from the influence THT’s program had on oral health practices. Figure 2: Code Categories for Oral Health Practices of Participants 47 Figure 2 displays the code categories that emerged from focus group data analysis on the oral health practices of the participants before and after the program. Behavior and attitudes about oral health appeared to change after participating in the program. Both adults and children displayed a change for behavior and attitude change post-program. Helpful factors that arose from the discussion regarding the effectiveness of THT program include the comprehensive information provided to participants regarding positive oral health practices. A large part of the discussion in the focus groups concentrated on what good oral health practices are and how participants incorporate them into their lives now that they and their children understand the importance of oral health. This statement displays how the families have incorporated what they learned about oral health into their daily lives: 48 Well, look. I think that they, well first my children brushed their teeth, but not with the importance that they saw after the class. Because, they brush because we send them to, “wash your teeth because you have to keep washing them”. But, after taking the class, they saw the importance, how the teeth can become damaged, and how the bottle, pacifier, and all that…er…they began to take more responsibility in taking care of their teeth. But, before they didn’t do it. They did it because they were told to. They didn’t do it just because. - Mother When asked about barriers in maintaining their children’s oral health, parents discussed several factors that still hinder them from maintaining their child’s oral health (see Figure 3 for a layout of the code categories): the cost of dental visits and dental products (7), having a hectic schedule (10), negative perceptions of/experiences with dentists (15). Of the barriers discussed, participants identified these three barriers as the most important in their lives. The cost of maintaining oral health was difficult to manage in two aspects: affording dental services (6), and also affording dental products (1). Hectic schedules were also mentioned for contributing to barriers in maintaining oral health of children. Parents discussed three main ways in which scheduling impacts oral health: having to constantly remind children to brush their teeth (5), not actually being with the child at ideal times to monitor teeth brushing (4), and remembering when children are due for a dental visit (2). Participants described negative perceptions of/experiences with dentists in several facets: general negative experiences (5), perceived negative treatment (by dentist) due to race/ethnicity (3), and a fear of the dentist on both the part of the parent (2) and 49 the child (5). Each barrier is discussed in greater detail and special attention will be given to the barrier: negative perceptions of/experiences with dentists in the following section. Cost: Participants discussed in the focus groups how the cost of dental services without insurance was too expensive for them to afford and phone survey data shows that lack of dental insurance was identified as the number one barrier (26.4%). Focus group participants noted that purchasing special toothpaste for children and for adults was also difficult to manage. The following statements display this view: Also, the insurance companies should help us. For us it is extremely expensive. I want to take them regularly but I can’t. It is a purely economical thing. - Father Look, for us, the economic crisis already changed everything… I can no longer buy the special kid toothpaste… there is no money… - Father Hectic Schedule: Phone survey data show that 15.3 percent of parents felt that being too busy was a barrier. Focus group data shed light on details of this barrier. Although participants were aware of how often children should brush and thought it was important that their children follow those guidelines, many expressed that it was difficult to ensure that children actually adhered to these practices. The following account illustrates how getting their children to brush is a barrier: 50 …my children, that they sometimes don’t want to [brush their teeth] because they think that rinsing is enough. No. That, that is enough. A rinse. But since the class, I worry for their teeth and I explain it to them. Only then do they understand. Only then do they understand. - Mother Participants also expressed that not being able to be with their children makes it challenging to make sure that they follow good oral health practices. Parents felt that there was not enough time to be with their children when they need to brush their teeth because they have to brush “the three times” and often, during those times, parents “are working.” During lunch, children are at school and sometimes parents are at work in the evening when the children are getting ready for bed. Another issue that emerged was remembering when the child is due for a dental checkup. Parents found it difficult because one has to “write [it] down” when their child last saw the dentist and remember six months later that they are due for a check-up again when there are so many other factors in daily life for parents to take care of. 51 Figure 3: Code Categories for Barriers in Maintaining Children’s Oral Health This figure provides a visual of the code category breakdown of the barriers identified as most important to participants in the focus groups. Subcategories are also displayed in the figure. For example, the code category of hectice schedules can be subcategoriezed into remembering to go to the dentis and not being with child at times of brushing. The most compelling information arising from these focus group discussions was the interaction between ethnicity and oral health. Two major concepts in understanding oral health in Mexican families emerged: Negative perceptions of/experience with dentists and cultural oral health related practices in Mexican families. Although focus group comments falling into these themes did not always come up with high frequency, the richness of the statements are extremely important in understanding and voicing the beliefs, experiences, 52 practices, and ideas of Mexican parents regarding the oral health of their children. Focusing on these themes will shed light on untold stories that may contribute to existing oral health disparities in immigrant Mexican and Mexican American communities. As described previously, participants expressed having negative experiences with and perceptions of dentists. Phone survey data found that language differences (16.5%) and being uncomfortable with available dentists (15.6%) were the text top barriers after cost. Statements relating to this issue made in the focus groups are as follows: general negative perception of/experiences with dentist, perceived negative treatment due to race/ethnicity, and fear of the dentist from both the parent and child. Specific issues mentioned included that dentists had failed to provide adequate care to participant’s children, appeared negligent, and were not good at working with children. Sometimes these perceptions were deemed attributable to public health insurance or racism. A few statements attributed harsh treatment of children due to the race of the dentist, in this case Asian. Participants discussed past negative experiences with dentists and believed that they had an essential right to go to the dentist and deserved to receive adequate treatment. After participating in the program, it became more apparent whether or not the dentist was providing thorough treatment for their children. The following statement captures this sentiment: Really being in the oral hygiene class, I learned a lot. What impacted me most, were my rights to go to the dentist. 53 Because my boy of 2 years, eh, I took him, since he got his first tooth. And they always told me, oh he’s fine, he’s fine. And when I learned that those little black points, my boy had cavities on all of his teeth and the dentist told me that he they were fine. And there, they gave me the information. They helped me to move, to go to a dentist for children. And…er, well, they helped me a lot. Because they had to work on all of his teeth. But now, well, now he doesn’t have any cavities. Through the information we received. - Mother This statement shows how THT’s program promoted agency within participants because they felt that they should and could have more control over the oral health of their children. This applies in two folds: parents learned that the majority of oral disease can be prevented through brushing and flossing, and furthermore, they felt that they had more of a right to question the dental services their children were receiving. Phone survey results show that 10.3 percent of respondents found locating an accessible dentist as a barrier. It is possible that this barrier is due to the small number of dentists that participate in public health insurance. Furthermore, focus group participants attributed having public health insurance, such as Medi-cal, as a reason behind why some dentists were not attentive to them and their children. This statement demonstrates this opinion: And sometimes you stay with a dentist, because you have an insurance like Medi-Cal and where they attend you, they don’t do their job well...you have to check them out. - Mother The literature has identified low quality public health dental service is an access barrier. This statement shows how marginalized communities are especially 54 subject to poor dental care because many live in low socioeconomic conditions. Large populations of Mexican Americans and other minority groups either do not have access to insurance or only have access to public dental health insurance, which has been identified as truly low quality (see Literature Review), thus, further marginalizing this underserved community and perpetuating the existing disparity. Others felt that negative experiences with dentists were due to the dentist’s lack of skill in knowing how to work with children. This comment displays how finding a dentist who is good at working with children was one of the largest barriers for some parents: To me the hardest is finding a dentist that knows how to deal with kids… mine only treats them roughly, and doesn’t even say hello to them… that I don’t like. - Mother It is difficult to find a pediatric dentist and even more difficult to find one that accepts patients with public health insurance or no insurance at all. Dental visits for children and parents, as the data from this research shows, can be unnerving. When dentists are not prepared or trained to work with children, this further exacerbates this fear, which may deter parents from taking their children to the dentist. Some participants even attributed this lack of skill in knowing how to work with kids to Asian American dentists in particular. They expressed having “bad experiences with Asian dentists” and felt that the difference in race of the dentist was a possible factor in contributing to this experience. This perception and 55 possible avoidance of Asian American dentists, although prejudiced, may contribute to access barriers to dentists. Families of Mexican heritage may be self-selecting away from Asian American dentists. Furthermore, it may be that negative interactions with Asian dentists lead patients to perceive them to have low cultural humility. Therefore, cultural humility may be very important for parents in taking their children to the dentist. Other negative perceptions of/experiences with dentists stemmed from perceptions of the dentist being careless due to racist beliefs held against the patient. This statement illustrates these feelings: You have to check the dentist that one goes to a lot, because sometimes they are very negligent with people and are racists. - Mother This statement expresses the idea that it is important for Mexican parents to be cautious of what dentist their child sees because there is a substantial probability that dentists do not provide equal care to their children due to their Mexican heritage. This may be consciously or subconsciously, but many studies in the Medical field have identified this phenomenon (see literature review). Whether or not this is perception is a reality, this is another access barrier parents feel they must deal with in maintaining their children’s oral health. Participants voice that one strategy to reduce this barrier would be for parents to find a dentist who is Mexican. One man said he would like to find an affordable dentist and had a “preference to a Mexican.” Other participants in this focus group laughed in agreement. 56 Lastly, many participants expressed fear as a barrier that impedes them from going to the dentist. Both parents and children felt this fear: For me, my children, I have to go with them to the dentist. I’ve also been sent to a children’s specialist and they say…that time that I went, a dentist told me, she explained to me, and I even more don’t want to take my children. Well, there’s a place where they tie them. Well now I’ve struggled a lot because they say, “Not me, No I won’t go to the dentist. I’ll just brush my teeth.” Because they are afraid of the dentist - even the youngest one’s hands tremble when we are about to take him. That’s the problem that I have, that they are afraid of going to the dentist. - Mother This statement displays the sentiment felt by both parents and children. Ideas regarding poor treatment of children by dentists, such as tying them down, whether they are accurate or not, act as a barrier for parents. If a parent does not trust the dental care system, and they observe pronounced fear in the child, such as trembling hands, this would lead to a cognitive dissonance for these parents. Now that they know the importance of oral health, parents would want to take their child to the dentist, however, if there is still a fear and lack of trust in available dentists, this could cause parents to have difficulty judging what the right decision is. It is possible that parents who are not aware of the importance of oral health would be greatly deterred from taking their children to the dentist if the fear and lack of trust in dental services is present. After discussing the barriers that were most important to participants, the participants we asked to discuss ways in which THT’s program could incorporate solutions to those barriers in the program. These results and suggests are discussed in greater detail in the following discussion section. 57 The focus group discussion uncovered cultural oral health related practices participants recalled their families exercising in Mexico. This theme was broken down into three categories: oral hygiene (18), help-seeking for oral ailments (8), and cultural beliefs of oral health (5). Table 1 provides a sample of quotes for the described cultural oral health related practices. Oral Hygiene: participants provided examples of practices used to clean teeth that are commonly used from Mexico, their country of origin. These practices range from using ground up burnt tortillas (2), cloth (2), soap (1), dental floss made from stings or leaves of trees (2), soft thin plastic (3), thread from socks (1), mashed mint leaves and salt (1), aloe vera (1), lime (1), baking soda (2), and (calcium) carbonate (2). Burnt tortilla grounds, cloth, and soap, were described as being used to clean the surface of the teeth and strings from the leaves of trees or the edges of thin plastic bags, or thread from socks are used to floss. Both mashed mint leaves with salt and aloe vera are used as homemade toothpaste. Lime, baking soda and (calcium) carbonate are used for whitening teeth. Participants said carbonate was used for oral health care in Mexican culture, but the term “carbonate” is commonly used when actually referring to calcium carbonate. Calcium carbonate, which is often used as a substitute for baking soda, is another homemade method for whitening teeth. Help-Seeking for Oral Ailments: Participants gave examples of helpseeking for oral ailments that are used in Mexican culture. These include cloves (3) avocado seeds (1), alcohol (2), cumin spices (1), and tying a string to one’s tooth and a doorknob and closing the door to remove the tooth (1). Cloves were 58 mentioned several times for use on a toothache to reduce pain sensations. Avocado seeds were suggested as being helpful in treating tooth decay. Alcohol on a piece of cotton is to be placed on the tooth and bit on until pain is relieved. Wine and cumin spices were also mentioned as reducing pain. Lastly, loose teeth are removed using string tied to the tooth and the doorknob and then shutting the door. The participants laughed during this explanation and mentioned that this does not actually work very often. Cultural Beliefs of Oral Health: Participants said that oral health was not emphasized as being important in Mexico (2) and also said that professional oral health care was less expensive in Mexico (3). After participating in THT program participants mentioned that they realized that the importance of oral health was emphasized more in the U.S. than in Mexico. They also mentioned that it is less expensive to get oral health treatment in Mexico than in the U.S. and that if possible, they travel to Mexico for that purpose. 59 Table 1: Sample Statements of Cultural Oral Health Related Practices This table displays the statements participants made that fall into three identified code categories, oral hygiene, help-seeking for oral ailments, and cultural beliefs of oral health. These codes are described in detail in the results section. 60 Discussion The present study sought to identify the effectiveness of THT’s program in addressing and helping parents overcome barriers in maintaining their children’s oral health, while also looking to understand Mexican cultural oral health related practices. This study provides support on previous findings and also identifies several novel findings. First, participants recognize THT’s home-based oral health program as helpful, comfortable, and important to their community. It provided a comprehensive preventative oral health curriculum to participants. Parents demonstrated a thorough knowledge of the importance of oral health from brushing and flossing to healthy eating and the importance of visiting the dentist. Furthermore, participants noted positive changes in the oral health behavior of their children (and themselves) post-program, including: improved brushing skills (brushing longer and with the correct circular technique), brushing more often, eating healthier, and using dental floss. Overall, the THT’s program proved to be effective in providing oral health education to the target community. Major barriers discussed in focus groups show that the cost of dental care still acts as a major barrier for parents after participating in the program. Focus group data elucidated more information on barriers parents experience that were listed on the phone survey. Specifically, being too busy was considered a substantial barrier from phone survey results and focus group data reveals that having a hectic schedule (i.e. being at work in the evenings) prevents parents from monitoring children’s oral health practices and remembering when it is time 61 to take children to the dentist. Also, having to constantly remind children to brush in combination with not being able to be with them to remind them posed as a barrier as well. Having negative perceptions of and experiences with the dentist was identified as another substantial barrier that may explain why 15.6 percent of parents were uncomfortable with available dentists and therefore, found that to be a barrier. Perceived negative treatment due to race/ethnicity and fear of the dentist by both the parent and the child were identified as major reasons for negative perceptions and experiences with the dentist. How do these identified barriers fit into the broader picture? The following sections discuss how the barriers identified in this study fit into the barrier categories identified in the literature review. Financial Barriers: Cost The focus group data provides more information on barriers the parents of Mexican heritage face in maintaining the oral health of their children, while also shedding light on barriers that previous literature does not address. Parents identified the cost of dental care as one of the predominant barriers they face. Parents who did not have dental insurance expressed an inability to finance visits to the dentists, children’s toothpaste, and changing toothbrushes every six months. Parents who had public health insurance felt that they did not receive adequate dental care from the dentists who accept insurance plans, such as Medicaid. Therefore, although they were insured, they felt they did not receive 62 quality oral health care for their children. If parents had access to a non-public health insurance, it is less probable that they would feel that they are receiving poor dental services. The literature supports this because most dentists do not accept public health insurance due to the low payment rates and complicated, non-standard administrative paper work. Therefore, it is not surprising that some dentists provide a lower quality of care for those on public health insurance. If a dentist does not feel that they are getting compensated adequately, it is likely that they will be less motivated to provide quality dental services. In fact, dentists who accept public health insurance may be so unmotivated to provide quality care that they neglect patients who appear to be more complicated and/or stressful to deal with. This could include patients of different cultures, SES, and age – such as children. While this is a predictable outcome when considering the difficulties dentists who participate in public health insurance face, it is not acceptable. Providing unequal treatment due to being inconvenienced by extra paper work is unethical. Furthermore, this displays a lack of compassion for patients. It is disheartening to know that low payment rates can lead dentists to knowingly neglect cavities. Something must be done to reduce this iniquity. Public health insurance polices and structure should be revamped to make public health insurance more attractive to dentists. The paper work system should be simplified to make it easier for dentists to deal with administrative business. Or, information should be provided to make the paper work process more clear. Furthermore, an incentive for dentists who participate in public health insurance should be incorporated into the Medicaid program. Perhaps 63 dental supply companies could collaborate with public health programs, such as Medicaid’s EPSDT, to make it more affordable for dentists to treat children on public health insurance. Let’s revisit the story of Deamonte and DaShawn Driver discussed previously in the introduction of this paper. Deamonte was an adolescent who died from a bacterial infection in his tooth that spread to his brain and DaShawn, his younger brother, lost his dentist because he “squirmed too much” in the seat. Both boys qualified for Medicaid (EPSTD), however, because of the low number of dentists participating in public health insurance, it was difficult for them to locate a dentist, and in Deamonte’s case, this lead to his death. DaShawn managed to find a dentist accepting Medicaid, however his dentist discontinued service because he was a difficult patient to deal with, even though DaShawn had developed abscesses from dental infection. While focus group data does not provide intimate details of exactly how and why parents felt that they received poor quality dental services from public health insurance, the fact that parents mentioned it as a barrier and the stories of Deamonte and DaShawn provide important evidence that dentist-patient relationships should be more deeply examined to understand how they play a role in oral health disparities for different groups, in this case, Mexican American children. Not having access to private insurance and having perceived negative experiences with dentists who accept public health insurance acts as a financial barrier that also could possibly be compounded with cultural and/or class differences between patient and dentist. Participants voiced having negative 64 experiences with and perceptions of dentists due to other barriers that can be seen as cultural and/or class differences between patient and dentist. The limited number of dentists who participate in Medicaid poses as a problem for white children on Medicaid, but it is even more of an issue for those who are minorities, in this case, children of immigrant Mexican and Mexican American parents. Most dentists are white and do not live in highly Latino populated areas. Specifically, within California, Latino dentists make up only 4.6% of the total dentist workforce, while California is 32.4% Latino. This means that one in every three Californians are Latino, while only one in every 20 California dentists are Latino (Hayes-Bautista et al., 229, 2007). Participants mentioned that a way to reduce barriers they face in taking their child to the dentist would be to have a Mexican dentist. Latino dentists are important in improving the dental health of the Latino community because they are more likely to speak Spanish and have offices located in highly Latino-populated areas and thus, they can reduce language barriers and location/transportation barriers while increasing dentist-patient concordance (Hayes-Bautista et al., 227, 2007). If the pool of dentists who accept Medicaid is already small, the pool of Latino dentists who accept Medicaid is likely to be even smaller, creating a double barrier in accessing dental care. Cultural and/or Class Differences as a Barrier: Negative Perceptions of/Experiences With Dentist 65 Parents expressed having negative experiences with and/or negative perceptions of dentists as a substantial barrier they faced in maintaining their children’s oral health. This is an under-examined barrier due to cultural and/or class differences between the patient and dentist. These results shed light on data from the phone survey THT conducted. When asked what barriers participants still face in taking their child to the dentist, 15.6 percent of the respondents expressed being uncomfortable with the dentist. Focus group participants expressed general negative perceptions of/experiences with the dentist and also identified specific negative perceptions, such as the perception that dentists are racist towards them and a fear of dentists. The statements mentioned in the focus groups could be the reasons that nearly 16% of phone survey participants reported being uncomfortable with dentists. This example of a negative experience one participant had with a dentist discussed in the results section provides substantial support and justification for having difficulty in finding a dentist for their child: …My boy of 2 years, eh, I took him [to the dentist], since he got his first tooth. And they always told me, oh he’s fine, he’s fine. And when I learned that those little black points, my boy had cavities on all of his teeth and the dentist told me that he they were fine…they had to work on all of his teeth. -Mother This example clearly shows that the dentist was neglecting the child. It is possible that the dentist was taking advantage of the parent’s lack of knowledge of oral health by seeing the child as a patient, but not actually providing restorative care to child’s caries. Perhaps this child had public health insurance 66 and the dentist wanted to save money by not filling the cavities since dentists do not make a large amount of money from public health insured patients. It is also possible that the dentist was not trained properly and did not detect the caries, however, considering there was caries on all of his teeth, this is highly unlikely. Regardless of the reason, the dentist provided inadequate service and allowed a child to continue on with decaying, untreated caries. The dentist-patient relationship is surprisingly unexamined in oral health literature, yet, the study of this dimension of oral health issues may help to better understand the causes of oral health disparities among marginalized communities. Perceived Negative Treatment due to Race/Ethnicity Focus group participants also mentioned that race/ethnicity sometimes seemed to be the reason dentists did not provide adequate care. Specifically, one participant expressed the need to “check the dentist that one goes to a lot, because sometimes they are very negligent with people and are racist.” This perception of receiving lower quality dental services because of one’s race, whether it is reality or a perception the patient has, is a significant problem. Further research must be conducted to understand if dentists are providing unequal treatment due to race/ethnicity or if this is just a perception Mexican and Mexican American parents have. If dentists are not providing unequal treatment (due to racism), it is important to identify why parents feel this way. Language differences can further complicate this issue of cultural differences between the dentist and patient and could lead parents of Mexican descent to perceive 67 racism. This barrier demonstrates the importance of stressing cultural humility in dentistry. A method to increase cultural humility in dentistry is for dental schools to initiate required courses on how to serve patients of different social and cultural backgrounds. Focus group participants also expressed that dental school students should work in underserved communities during dental school to both help the community and the students. …but, also, to ask all of these students that are studying, to give more services to the community. Like the students, those who are studying to be dentists, that they give more services to the community. That way, it helps them and us also. - Mother Increasing public service for dental students will provide them with more experience in dentistry and help communities receive affordable dental services. Furthermore, dental schools could initiate CBPR projects in neighboring communities of the school to better understand how to serve the community, increase awareness of the importance of oral health, and even possibly increase the interest of Mexican American youth in seeking professions in the dental field. Fear Participants expressed that both they and their children had a fear of the dentist. While this seems like a common perception people have of dentists, not specific to culture, perhaps there is a cultural element present. Participants described the difference on the emphasis of the importance of oral health in 68 Mexico versus the United States. They expressed that oral health was not given very much importance in Mexico as compared to the United States. I think that the first impression is that you realize that people do care about the health of teeth and moreover the health of, the oral hygiene of the teeth. Because, regularly in our countries, this isn’t done and the information isn’t available that, that is presented here. - Mother Perhaps this difference in emphasis on oral health contributes to the fear of dentists and the idea of the unfamiliar Mexican families seemed to express towards dentists. Possible reasons why oral health is not emphasized as important in Mexico may be due Mexico’s rural structure. The remoteness of the country may make access to health care in general difficult and a common trend among many populations is to prioritize general health over oral health, rather than include it in the category of general health. Literature on fear of dentists in children identifies one of the sources as a fear of strangers in general (Milgrom et al., 318, 1995). Perhaps fear of strangers as an origin of childhood fear of the dentist is complicated by the added component of differing cultures between patient and dentist. There is little research on how race and ethnicity differences between patient and dentist influence (or do not influence) fear of the dentist. Further research should be conducted to understand this relationship. Fear of the dentist has been correlated with “utilization of the dentist during childhood: relative to children with little fear, children with high dental fear 69 are about twice as likely to not make a dental visit, all other things equal” (Milgrom et al., 313, 1995). In considering other factors that Mexican and Mexican American parents face in maintaining their children’s health, such as the perception that dentists do not treat their child properly, one could imagine that this would add to fear that both parents and children have of the dentist. If both child and parent perceive the dentist as unfriendly and harsh, this could deter Mexican American children from making dental visits. As identified in the literature review, Mexican American children had the lowest dental visits in the U.S. during this past year (see literature review). Perhaps one of the reasons for this is due to a unique fear Mexican American children and their parents have of the dentist. THT’s community oriented program made participants feel very comfortable and even moved participants to want to get more people in their community involved in the cause: Well, in my case, the first impression was that the program was very good and that it was finally arriving to the houses of the people with information regarding oral hygiene with the purpose of creating a healthier community… the greatest part of the programs nowadays are directed towards writing, towards reading, and very few programs are directed to oral health. It was a very good first impression, and my intention was to keep this going, to get more people involved… - Mother This statement demonstrates how THT’s approach falls in line with several CBPR principles and its approach to reducing public health disparities. The homebased structure of the program and the familiarity of the Promotore(a) as a fellow 70 community member with a similar cultural background, promotes community cohesiveness and motivates participants to instigate further social change. Research done within the community can raise awareness of the importance of oral health and “expand social structures and processes that contribute to the ability of community members to work together to improve health” by building on strengths and resources within the community (Israel et al., 178, 1998). By involving the community in the cause to reduce oral health disparities, there is a greater potential for Mexican American community members to decide to work in the dental field so that they can play a more active role in oral health awareness. Additionally, the exposure to oral health care research could lead to increased diversity in dentistry. If more Mexican Americans become dentists, this could increase participation in Medicaid because of a desire to reach out to one’s own community and other low-income children. However, more CBPR and CBPRrelated programs must be initiated and evaluated on a long-term scale to confirm these potential outcomes. Effects of Low SES on Family Behavior Hectic Schedules Living in low socioeconomic conditions is known to increase stress levels (McEwen and Seeman, 30, 1999). Increased stress levels are often due to the increased pressure to provide for the family and maintain it’s overall well-being. Where does oral health fit in here? As parents have to work more hours to make ends meet, it becomes more difficult to maintain all aspects of well-being for the 71 family – in this case, oral health. Focus group participants expressed frustrations in having time to ensure that their children brush their teeth and floss. Reasons for this include not being with children at ideal times of brushing such as lunch and the evening time, having to constantly remind children to brush their teeth, and having difficulty remembering and making time to take children for dental visits. Living in low SES makes it difficult for parents to juggle all of these issues, therefore, parents may place less emphasis on oral health, especially if it is not perceived as being as important as medical health. It is important to raise awareness that oral health is part of general health and can contribute to other health complications outside of the oral cavity. Cultural Oral Health Related Practices The Mexican cultural oral health related practices identified in this study did not appear to be poor oral health practices that could increase risks of oral disease. Oral hygiene practices identified were ones that are considered natural oral cleansing practices. Using a mashed up burnt tortilla is similar to using charcoal toothpaste, which is a product made in several other countries, such as Japan. Using a salt and mint mixture as toothpaste is considered an herbal way of cleaning teeth (http://www.consultation.ayurvediccure.com/herbal-ways-ofcleaning-teeth/). Aloe vera has been studied for its healing qualities and has been found to be effective in killing bacteria that develop on the teeth as long as 70% of the mixture contains pure aloe vera (http://www.enhancedtoothpaste.com/AloeVeraforDentalHealth.htm). Using string and thin plastic as floss has not been shown to increase risk of oral 72 disease. What these practices do show, are that they are not the ‘mainstream American way’ of cleaning teeth. And while, they may not be the ideal form of cleaning teeth, it is apparent that they are not bad oral health practices. Many of these practices are alternative methods of cleaning teeth when other more ideal forms are not available for socioeconomic reasons. In fact, some statements made by participants show that they know the correct technique of brushing teeth, which is in a circular motion: With my grandma, “you don’t have a toothbrush? Use a cloth and with that try to circul…circulate.” - Mother Information regarding help-seeking for oral ailments specific to Mexican culture include using an avocado seed as a natural filling for a decaying tooth. The avocado seed has natural soothing qualities that provide a temporary filling for the tooth. Cloves are used as a natural pain reliever for toothaches and can help ease the pain when a tooth is being removed. Cumin spices have also been used to relieve oral pain. Many of these practices are not limited to Mexican culture but are used in other cultures as well. Cumin spices were used in Ancient Egypt and as mentioned above, charcoal is used in Japan to clean teeth (http://www.herbco.com/p-353-cumin-seed-powder.aspx). Again, these practices have not been shown to damage teeth. These home remedy practices could be a result of cultural differences – or, they could be a result of a difference in socioeconomic conditions. If one is not in a financial position to replace toothbrushes for every family member every 3 months and purchase separate toothpaste for children, using the next best practice is the logical step. Many of 73 these families are living in low SES and come from Mexico, which is in a lower economic status than the United States; therefore, oral health may seem less of an urgent need for these families. This study has some limitations. First, THT’s program did not have a control group to compare actual oral health practice improvements so it is difficult to be certain that the participant’s oral health practices actually improved. Furthermore, the evaluation of changed oral health behaviors was self-reported and this could lead to inaccurate information due to participants providing responses that they feel the researcher wants to hear. Another limitation of this study was that it was done in another language than the researcher’s. This presented to be difficult in overseeing the quality of the research methods after documents were translated from English into Spanish. In order to minimize the compromise of the quality of the research, efforts were made to provide clear directions to research assistants and moderators (who spoke Spanish) to ensure that the translated documents delivered the same message as the English versions. To ensure accurate document translation, other Spanish speakers also reviewed the translated documents. Another limitation to this study is that this information cannot be directly applied to other Latino populations because it is specific to Mexican and Mexican American populations in Santa Clara County. However, interventions that do not acknowledge the specific characteristics of target populations are often less effective in raising awareness of the specific intervention issue. Therefore, in 74 terms of internal validity, the specificity of the target population can also be viewed as a strength in this study. This study identified cultural oral health practices that have not been thoroughly identified in the literature. Additionally, it elucidated more information regarding barriers Mexican American children and their families face in maintaining oral health that have not been focused on. This includes negative perception of and experiences with the dentist, such as fear of the dentist and feelings of unequal treatment due to race/ethnicity. The collaboration in this study with THT provided a more in-depth look at the effectiveness of the program because both quantitative and qualitative data were used to examine the program and the oral health status of the community. 75 Conclusion This study found that THT’s home-based oral health program was overall successful in raising awareness about oral health in immigrant Mexican and Mexican American communities in Santa Clara County. However, one area of improvement identified in the focus groups was to include more information on how to navigate locating an affordable dentist. One participant identified another oral health program at her child’s school that provides detailed and helpful information on finding a dentist. The woman explains that the program: …give[s] us a lot of information there [at her child’s school]…they tell us where we can go, if we need any help. If we don’t have insurance…where we can go. They tell us where our children can be attended. And that helps us. That’s were we got that plan of the dentist. - Mother While THT’s program possesses similar characteristics of CBPR, it could potentially improve by placing more of an emphasis on partnering with existing community programs. In particular, THT could collaborate with the school program mentioned above and therefore bolster their program by using the school’s curriculum on locating an affordable dentist to other locations not near the school, such as Gilroy. THT’s program proved to be successful in tailoring the program to the specific community and making a positive impact on participants. For example, a participant was able to identify that her child has caries on every single primary tooth after participating in the program. Even though the participant was already 76 seeing a dentist before the program, the knowledge she obtained from the homebased meeting about her child’s teeth enabled her to take her child to another dentist to get her child’s teeth restored (see results). This shows that the program provided participants with not only oral health knowledge, but a sense of social motivation to take ownership of their children’s oral health and get involved in the community. Cost was emphasized as a continued barrier for parents who participated in THT’s program. Under-examined barriers were identified in this study as well. Specifically, negative perceptions of and experiences with dentists stemming from parent and child fear and perceived as motivated by racism. Hectic family schedules, such as remembering children are due for a dental visit and not being with the child to remind and monitor oral health practices, also were identified as barriers. The cultural oral health practices identified in the focus groups did not appear to act as a barrier contributing to the prevalence of oral disease in Mexican Americans. This finding should be taken into account in following studies in order to limit the possible stigmatization of this already marginalized group as having poor oral health status due to their cultural practices. THT could incorporate solutions to these barriers by brainstorming with parents. Participants from the focus groups felt that the high cost of professional dental care could be addressed by setting up payment plans with dentist on dental check-ups and procedures. Furthermore, the government programs, such as Medicaid could be revamped to manage the issues of complicated paper work and under paying of dentists. As mentioned previously, increasing dental student 77 community service requirements while at dental school could also make dental treatment more affordable for these parents. To address hectic schedules, time management skills were discussed to help make time to brush and take children to the dentist. Focus group participants noted that “think[ing] about a routine” and incorporating brushing and flossing teeth into the daily schedule helps participants to combat having a hectic schedule. Participants also suggested making brushing teeth a game to encourage children to brush their teeth. Another form of encouragement in overcoming the barrier of fear is to motivate children to go to the dentist by taking them somewhere they really enjoy after going to the dentist and supporting them while they are at the dentist. Another way to allay child fears of the dentist is by communicating with the dentist about what the child is afraid of and how to make the child more comfortable. One parent found this technique to be especially helpful for her little girl: I think that one has to talk with the dentist to see what the fear is. For example, one of my daughters doesn’t like them to put water and when she sees that they’re going to grab the little hose, that’s, well, it’s crying and crying and crying. But, the dentist, I talked to him and he lets her get up and rinse. - Mother Communication with the dentist may also reduce parent’s negative perceptions of dentists. If part of the negative perception has to do with the parents’ fear as well, then by becoming more familiar with the child’s dentist, parents may become less skeptical and more trusting of the provider. 78 While the program was overall successful, there is a glass ceiling that non-profit out reach programs face in helping underserved communities find professional dental care. That is, that no matter how much the program works to help parents navigate locating a dentist, the program has little influence on the negative perceptions and experiences that these parents have of dentists. Dental institutions and dentists themselves can only address this dentist-patient relationship. These systems need to allocate energy into promoting the importance of making all patients feel comfortable and trusting of the service that they are receiving. This could be done by requiring dental students to take courses on cultural awareness and looking for applicants that value cultural humility. By increasing the awareness of dental disparities in communities of color among dental institutions and the dissemination of oral health awareness by interventions, such as THT’s home-based oral health program, it is possible to remedy this ‘silent epidemic.’ 79 Appendix A.1: The Health Trust Internal Evaluation Survey Note: Questions I contributed are highlighted START TIME:____________ INTERVIEWER:_______________ INTERVIEW DATE:_______ HOME MEETING DATE: Introduction Hello, my name is ________ and I work for The Health Trust. A while back, you participated in a home meeting on oral health. We are gathering information from people who participated in an oral health home meeting to evaluate and improve our program. Your answers will remain confidential and anonymous and will be combined with answers from many other participants. Can we take a few minutes of your time? If no: Are you sure? It would help us to understand what you think of our services. If no, again: Thank you for your time. Proceed to next participant on list. If yes: Proceed with next paragraph. We have several questions we would like to ask you related to the oral health education you received. Your feedback is very important to us. Do you have any questions before we get started? 80 FAMILY INFORMATION 1. Do you remember participating in a home meeting on oral health? (REMIND RESPONDENT OF MONTH/YEAR OF HOME MEETING) Yes…………………………………………. No………………………………………….. IF YES, CONTINUE WITH INTERVIEW, ASK QUESTION 2. IF NO, THANK YOU FOR YOUR TIME. END INTERVIEW. 2. How many children do you have at home? Number of children………………______ 3. What are their ages? Child 1 ___ Years ___ Months Child 2 ___ Years ___ Months Child 3 ___ Years ___ Months Child 4 ___ Years ___ Months Child 5 ___ Years ___ Months 4. How many adults live in your home? Number of adults…………………_______ ORAL HEALTH EDUCATION AND ACCESS TO AND UTILIZATION OF DENTAL CARE 5. When was the last time your child/children visited a dentist? (RECORD FOR MOST RECENT VISIT) Month ____ Year_____ My child/children has never visited a dentist……………………………………………... 81 IF NO VISIT, SKIP TO NUMBER 10 6. Why did you decide to take your child to the dentist? (OPEN ENDED QUESTION, DO NOT READ THE LIST. CHECK CLOSEST RESPONSE OR WRITE IN OTHER RESPONSE) Due for a check up…………………………….. Teeth/mouth hurt………………………………. School/day care recommended or required…………………………………..……... Health care provider recommended………….. Health educator at home meeting recommended…………………………………... Other ________________________................ 7. Where did you take your child for dental care? (OPEN ENDED QUESTION, DO NOT READ THE LIST. CHECK CLOSEST RESPONSE OR WRITE IN OTHER RESPONSE) Primary Care Dentist………………………….. Community Dental Clinic..……………………. Mobile Dental Unit.……………………..……... Other…………………………………..……….. 8. How did you pay for the dental care? (CHECK ALL THAT APPLY) 82 Dental insurance………………………………… Self-pay……………..…………………………….. Free service………………………………………. Other _______________________.................... 9. Before this visit, how long had it been since your child/children visited a dentist? (OPEN ENDED QUESTION; CHECK CLOSEST RESPONSE; THEN, SKIP TO NUMBER 11) Less than six months……………………………. Between six months and one year……………… More than one year ………………………………. This was first visit…………………………………. 10. Why has your child/children not seen a dentist? (OPEN ENDED QUESTION, DO NOT READ LIST; CHECK ALL THAT APPLY) No dental insurance…………………………….. Can’t afford to pay………………………………. Doesn’t need one ………………………………. Don’t know how to find a dentist………………. Other ________________________.................. 11. I’m going to read a list of barriers that sometimes prevent some parents from taking their children to the dentist. Please let me know, which of the following barriers you have experienced by answering yes or no. Lack of dental insurance Yes…………………………………………. No………………………………………….. Transportation to the dentist Yes…………………………………………. No………………………………………….. Language differences Yes…………………………………………. No………………………………………….. You are too busy Yes…………………………………………. No………………………………………….. Inconvenient dental appointment hours Yes…………………………………………. No………………………………………….. Lack of accessible dentists Yes…………………………………………. 83 No………………………………………….. Finding a dentist you are comfortable with Yes…………………………………………. No………………………………………….. Are there other barriers you have experienced? IF NO BARRIERS CHECKED, SKIP TO #13 12. On a scale of 1 to 5, with 1 being not at all helpful and 5 being extremely helpful, How helpful was the oral health program in providing you with information or resources to overcome these barriers? (CIRCLE RESPONSE) Not at all helpful Extremely Helpful 1 2 3 4 5 ORAL HEALTH KNOWLEDGE AND BEHAVIOR CHANGE 13. What is one thing you remember from the home meeting on oral health? (OPEN ENDED QUESTION, DO NOT READ THE LIST. CHECK ALL THAT APPLY OR WRITE IN OTHER RESPONSE) Brushing…………………………………………. Flossing…………..……………………………… Communication with Dentist…………………… Healthy Eating…………………………………… Other ________________________................. Can’t remember anything specific….................... 14. Was this information you remember from the home meeting new information for you? (PROBE: DID YOU LEARN THIS FOR THE FIRST TIME AT THE HOME MEETING?) Yes…………………………………………. No………………………………………….. 15. Does every child in your home own his/her own toothbrush? (OPEN ENDED QUESTION, DO NOT READ LIST. CHECK CLOSEST RESPONSE OR WRITE IN OTHER RESPONSE.) Yes, everyone has his/her own toothbrush……… No, children share toothbrushes…………………… No, children don’t have toothbrushes……………… Other______________________________............ 84 IFANSWER IS “NO”, ASK WHY NOT? _____________________________________________ 16. How often does your child/children brush his/her teeth each day? (READ EACH OPTION AND CHECK ONE) After every meal……………………………………… Three times/day………………………………………. Two times/day…………………………………………. Once a day…………………………………………….. Other _______________________________........... 17. Did the number of times your child/children brushes his/her teeth each day (READ EACH OPTION AND CHECK ONE) Increase after the home meeting? ………………………. Decrease after the home meeting? …………………….. Remain about the same after the home meeting?.……. 18. How often does your child/children floss his/her teeth? (READ EACH OPTION AND CHECK ONE) At least once a day…………………………………… About 5 times/week…………………………………… About 3 times/week…………………………………… About 1 time/week…………………………………….. Less than 1 time/week………………………………… Never…………………………………………………… 19. Did the number of times your child/children flosses his/her teeth each day (READ EACH OPTION AND CHECK ONE) Increase after the home meeting? ………………………. Decrease after the home meeting? …………………….. Remain about the same after the home meeting?.……. 85 20. How often does your child/children eat candy or other sweets? (READ EACH OPTION AND CHECK ONE) At least once a day…………………………………… About 5 times/week…………………………………… About 3 times/week…………………………………… About 1 time/week…………………………………….. Less than 1 time/week………………………………... Never…………………………………………………… 21. Did your child/children eat candy or other sweets (READ EACH OPTION AND CHECK ONE) Less often after the home meeting………………… More often after the home meeting………………… About the same after the home meeting. …………. 22. How often does your child/children eat fruits and vegetables? (READ EACH OPTION AND CHECK ONE) At least three times a day…………………………… About 1 time/day……………………………………… About 3 times/week…………………………………… About 1 time/week…………………………………….. Less than 1 time/week………………………………... Never…………………………………………………… 23. Did your child/children eat fruits and vegetables (READ EACH OPTION AND CHECK ONE) More often after the home meeting………………… Less often after the home meeting…………………. About the same after the home meeting. ………….. PERCEPTIONS ABOUT HOME-BASED HEALTH EDUCATION 24. Was this the first time you received any kind of health education? Yes…………………………………………………….. No…………………………………………………….... 86 25. Was this the first time you received health education in someone’s home? Yes…………………………………………………….. No……………………………………………………..... 26. Is there anything you didn’t like about the home health education? (OPEN-ENDED QUESTION; RECORD RESPONSE) _______________________________________________ 27. Is there anything you especially liked about the home health education? (OPEN-ENDED QUESTION; RECORD RESPONSE) ________________________________________________ 28. On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the oral health education you received? (READ NUMBERS AND CIRCLE NUMBER SELECTED) Poor 1 Excellent 2 3 4 5 87 PERCEPTIONS ABOUT HEALTH EDUCATOR 29. On a scale of 1 to 5, with 1 being VERY LITTLE KNOWLEDGE and 5 being A LOT OF KNOWLEDGE, how would you rate the health educator’s knowledge about oral health? (READ NUMBERS AND CIRCLE NUMBER SELECTED) Very Little 1 30. A Lot 2 3 4 5 Was the health educator able to answer all your questions? Yes……………………………………………………. No……………………………………………………... If no, do you still have questions? What are they? 31. Is there anything in particular you remember about the health educator that you would like to share? (OPEN ENDED; RECORD RESPONSE; if nothing, write “nothing”) _______________________________________________ 32. On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the COMMUNICATION SKILLS of the health educator? (READ NUMBERS AND CIRCLE NUMBER SELECTED) Poor 1 33. Excellent 2 3 4 5 On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the overall EFFECTIVENESS of the _______________________________________________ health educator? (READ NUMBERS AND CIRCLE NUMBER SELECTED) Poor 1 Excellent 2 3 4 5 FUTURE HEALTH EDUCATION OPPORTUNITIES 34. Are you interested in attending future home health education meetings? Yes……………………………………………………. No……………………………………………………... If yes, what health topics would you like to learn about? (OPEN ENDED) 88 ________________________________________________ 35. Would you consider hosting a home health education meeting at your home? Yes……………………………………………………. No……………………………………………………... 36. If yes, can we give your name and phone number to someone to follow-up with you? (IF YES, NOTE ON THE HOME MEETING LOG) Yes……………………………………………………. No……………………………………………………... 37. On a scale of 1 to 5, with 1 being VERY UNLIKELY and 5 being VERY LIKELY, how likely is it that you would recommend a home health education meeting to your friends, family, or neighbors? (READ NUMBERS AND CIRCLE NUMBER SELECTED) Very Unlikely 1 38. Very Likely 2 3 4 5 Is there anything else you would like to tell us about your experience with the home meeting on oral health? (OPEN-ENDED QUESTION; RECORD RESPONSE) ________________________________________________________________________________________________________________________ Thank You This brings us to the end of our questions. Thank you for providing us with this important feedback. We greatly appreciate your time. Would you like to participate in a small group conversation about your experience with this program? The group would be meeting in a convenient location for about 45 minutes. ($25 gift card was offered for them to participate). 89 IF YES: Record name and contact information on a separate roster Tell them: Someone from The Health Trust will call you with more details in the coming month. END TIME: _______________ 90 Appendix A.2: The Health Trust Internal Evaluation Survey in Spanish Hora de inicio: ____________ Entrevistador: ____________Fecha de entrevista: _______ Fecha de la reunión en casa: Introducción Hola, mi nombre es ________ y trabajo para The Health Trust. Hace algún tiempo, usted participo en una reunión en casa con información de salud oral. Nosotros estamos recopilando información de personas que participaron en una reunión en casa para evaluar y mejorar el programa. Sus respuestas serán confidenciales y anónimas y serán combinadas con respuestas de otros participantes. ¿Puede usted regalarnos unos minutos de su tiempo? Si la respuesta es no: ¿Esta usted seguro/a? Nos ayudaría a entender que piensa usted sobre nuestros servicios. Si la respuesta en nuevamente, no: Gracias por su tiempo. Proceda con el siguiente participante en la lista. Si la respuesta es, si: Proceda con el siguiente párrafo. Tenemos algunas preguntas que nos gustaría hacerle en relación a la información sobre salud oral que recibió. Sus respuestas son muy importantes para nosotros. ¿Tiene usted alguna pregunta antes de que comenzar? INFORMACION FAMILIAR 1. Recuerda usted haber participado en una reunión de casa que ofrecía información de salud oral? (Recuerde al entrevistado el mes y año de la reunión en casa) Si......................................................................................... .. No.......................................................................................... SI LA RESPUESTA ES SI, CONTINUE CON LA ENTREVISTA, HAGA LA PREGUNTA No. 2 SI LA RESPUESTA ES NO, GRACIAS POR SU TIEMPO. FINALIZE LA ENTREVISTA 2. ¿Cuántos niños tiene usted en su casa? Número de niños………………______ 91 3. ¿Quė edades tienen? Niño 1 ___ Años ___ Meses Niño 2 ___ Años ___ Meses Niño 3 ___ Años ___ Meses Niño 4 ___ Años ___ Meses Niño 5 ___ Años ___ Meses 4. ¿Cuántos adultos viven en su casa? Número de adultos……………_______ EDUCACION DE SALUD ORAL Y ACCESO A LA UTILIZACION DE CUIDADO DENTAL 5. ¿Cuándo fue la última vez que su niño (s) visitó al dentista? (ANOTE LA VISITA MAS RECIENTE POR CUALQUIER NIÑO) Mes ____ Año_____ Mi niño (s) nunca han visitado al dentista……………………………………………................ .. SI NO HA VISITADO, SALTE A LA PREGUNTA NUMERO 10 6. ¿Porquė decidió llevar a su niño (s) al dentista? (PREGUNTA ABIERTA, NO LEA ESTA LISTA. SELECCIONE LA RESPUESTA MAS CERCANA O ESCRIBA OTRA RESPUESTA) Para una revisión................................................................... Dolor de dientes/boca............................................................ Recomendación o requisito de la escuela y/o guardería................................................................................ Recomendación del proveedor de salud............................... El educador de salud de la reunión en casa me lo recomendó............................................................................. Otro ________________________...................................... 7. ¿Donde llevo a su niño (s) para cuidado dental? (LEA ESTA LISTA Y MARQUE LA RESPUESTA) Su dentista regular................................................................ Clínica comunitaria dental.................................................... Unidad dental Mobil.............................................................. Otro ________________________..................................... 8. ¿Cómo pago por el cuidado dental? (MARQUE TODAS LAS QUE APLICAN) 92 Seguro dental....................................................................... Pago en efectivo................................................................... Servicio gratis....................................................................... Otro ________________________..................................... 9. Antes de la visita, ¿Cuánto hacia que su niño (s) no visitaban al dentista? (PREGUNTA ABIERTA; SELECCIONE LA RESPUESTA MAS CERCANA; LUEGO,) Hace menos de seis meses................................................ Entre seis meses y un año................................................... Hace más de un año............................................................ Esta era la primera visita...................................................... SALTE A LA PREGUNTA NUMERO 11 10. ¿Porquė su niño (s) no han visto a un dentista? (PREGUNTA ABIERTA, NO LEA ESTA LISTA. MARQUE TODAS LAS QUE APLICAN) No tengo seguro dental....................................................... No puedo pagar................................................................... No necesito un dentista....................................................... No se como encontrar a un dentista................................... Otro ________________________..................................... Continua en el siguente pagina 93 11. Voy a leerle una lista de impedimentos que algunas veces evitan que los padres puedan llevar a su niño (s) al dentista. Por favor, dígame contestando a cual de estos impedimentos se a enfrentado. Falta de seguro dental Si............ No.......... Transporte para ir al dentista Si............ No.......... Diferencias en el lenguaje Si............ No.......... Usted esta muy ocupado/a Si............ No.......... Horas inconvenientes para las citas dentales Si............ No.......... Falta de dentistas accesibles Si............ No.......... 94 Dificultad para encontrar un dentista con quien se sienta cómoda Si............ No.......... ¿Hay algún otro impedimento que usted ha experimentado? _______________________________________________ SI NO HAY IMPEDIMENTOS SELECCIONADOS, SALTE A LA PREGUNTA #13 12. En una escala de 1 a 5, donde 1 significa que no ha sido de mucha ayuda y 5 significa de mucha ayuda, ¿Cuánta ayuda y recursos cree usted que le ofreció la información ofrecida por el programa de educación para vencer esos impedimentos? (CIRCULE LA RESPUESTA) No de mucha ayuda De mucha ayuda 1 2 3 4 5 CONOCIMIENTO DE SALUD ORAL Y CAMBIO EN LOS HABITOS 13. ¿Cuál es una de las cosas, relacionadas con higiene oral, que usted recuerda de la reunión en casa? (PREGUNTA ABIERTA, NO LEA ESTA LISTA. MARQUE TODAS LAS QUE APLICAN) Cepillado.............................................................................. Uso de hilo dental................................................................ Comunicación con el dentista................................................................................ Alimentación saludable....................................................... Otro ________________________..................................... No puede recordar nada específico..................................... 95 14. ¿Es esta información que recuerda de la reunión en casa, información nueva para usted? (VERIFIQUE: USTED APRENDIO SOBRE ESO POR PRIMERA VE EN LA REUNION DE CASA? Si.................................................................................. ...... . . No................................................................................. ...... . 15. Cada uno de sus niños (as) en la casa, ¿Tienen su propio cepillo dental? (PREGUNTA ABIERTA, NO LEA ESTA LISTA. SELECCIONE LA RESPUESTA MAS CERCANA O ESCRIBA OTRA RESPUESTA) Si, cada uno tiene su propio cepillo dental........................ No, ellos comparten cepillo dental....................................... No, los niños no tienen cepillo dental................................... Otro______________________________.......................... SI LA RESPUESTA ES “NO”, PREGUNTE ¿Por qué NO? _____________________________________________ 16. ¿Cuántas veces su niño (s) se lavan sus dientes al día (sin o con ayuda suya)? (LEA CADA OPCION Y SELECCIONE UNA) Después de cada comida................................................... Tres veces al día.................................................................. Dos veces al día................................................................... Una vez al día.................................................................. .. .. Otro _______________________________................... . .. 17. El número de veces que su niño (a) se lava sus dientes diariamente (sin o con ayuda suya) (LEA CADA OPCION Y SELECCIONE UNA) Aumento después de la reunión en casa..................... ..... .. Disminuyo después de la reunión en casa...................... .. . Continúa igual después de la reunión en casa............... .. 18. ¿Cuántas veces usa el hilo dental su niño (a) (sin o con ayuda suya)? (LEA CADA OPCION Y SELECCIONE UNA) 96 Al menos una vez al día...................................................... Alrededor de 5 veces a la semana...................................... Alrededor de 3 veces a la semana...................................... Alrededor de 1 vez a la semana.......................................... Alrededor de 1 vez al mes................................................ ... Nunca................................................................................ ... 19. El número de veces que su niño (a) usa el hilo dental diariamente (sin o con ayuda suya) (LEA CADA OPCION Y SELECCIONE UNA) Aumento después de la reunión en casa............................. . Disminuyo después de la reunión en casa.......................... Continúa igual después de la reunión en casa.... ............... 20. ¿Cuán seguido su niño (s) comen dulces? (LEA CADA OPCION Y SELECCIONE UNA) Al menos una vez al día...................................................... Alrededor de 5 veces a la semana....................................... Alrededor de 3 veces a la semana....................................... Alrededor de 1 vez a la semana........................................... Alrededor de 1 vez al mes.................................................... Nunca........................................................................ ........... 21. Su niño (s) comen dulce (LEA CADA OPCION Y SELECCIONE UNA) Mas seguido después de la reunión en casa.................... Menos seguido después de la reunión en casa................ Continúa igual después de la reunión en casa.................. 22. ¿Cuán seguido su niño (s) comen frutas y verduras? (LEA CADA OPCION Y SELECCIONE UNA) Al menos tres veces al día.................................................. Alrededor de una vez al día................................................ . Alrededor de 3 veces a la semana....................................... Alrededor de 1 vez a la semana........................................... Menos de una vez a la semana............................................ Nunca................................................ ................................... 97 23. ¿Come su niño (s) frutas y verduras (LEA CADA OPCION Y SELECCIONE UNA) Mas seguido después de la reunión en casa................. ... Menos seguido después de la reunión en casa................. Continúa igual después de la reunión en casa................. PERCEPCION ACERCA DE LA EDUCACION DE SALUD DE LAS REUNIONES EN CASA 24. ¿Fue esta la primera vez que usted recibió educación de salud? Si................. .......................................................................... No................. ......................................................................... 25. ¿Fue esta la primera vez que recibió información de salud en la casa de alguien? Si................. .......................................................................... No................. ......................................................................... 26. ¿Hubo algo que a usted no le gustara de la educación de salud en casa? (PREGUNTA ABIERTA; ESCRIBA LA RESPUESTA) _______________________________________________ 27. ¿Hay algo en especial que a usted le haya gustado de la educación de salud en casa? (PREGUNTA ABIERTA; ESCRIBA LA RESPUESTA) ________________________________________________ 28. En escala de 1 a 5, donde 1 significa POBRE y 5 significa EXCELENTE, como diría usted que fue la educación de salud oral que recibió? (LEA LOS NUMEROS Y CIRCULE EL NUMERO SELECCIONADO) 98 Pobre 1 Excelente 2 3 4 5 PERCEPCION ACERCA DEL EDUCADOR DE SALUD 29. En escala de 1 a 5, donde 1 significa MUY POCO CONOCIMIENTO y 5 significa MUCHO CONOCIMIENTO, ¿Cuánto conocimiento cree usted que el educador tiene sobre salud oral? (LEA LOS NUMEROS Y CIRCULE EL NUMERO SELECCIONADO) Muy poco 1 30. Mucho 2 3 4 5 ¿Pudo el educador de salud contestar a todas las preguntas? Si................. .......................................................................... No................. ......................................................................... Si la respuesta es no, ¿Tiene usted todavía preguntas? ¿Cuáles son? _______________________________________________ 32. En escala de 1a 5, donde 1 significa POBRE y 5 significa EXCELLENTE, ¿Cómo definiría LA HABILIDAD DE COMUNICACION del educador de salud? (LEA LOS NUMEROS Y CIRCULE EL NUMERO SELECCIONADO) Pobre 1 33. Excelente 2 3 4 5 En escala de 1a 5, donde 1 significa POBRE y 5 significa EXCELLENTE, ¿Cómo definiría la EFECTIVIDAD del educador de salud? (LEA LOS NUMEROS Y CIRCULE EL NUMERO SELECCIONADO) Pobre 1 Excelente 2 3 4 5 OPORTUNIDADES FUTURAS DE LA EDUCACION DE SALUD 34. ¿Esta usted interesada en asistir a reuniones en casa con información de salud? Si................. .......................................................................... No................. ......................................................................... Si la respuesta es si, ¿Sobre que tipo de información le gustaría aprender? (PREGUNTA ABIERTA) 99 ________________________________________________ 35. ¿Consideraría usted invitar a una reunión de información de salud en su casa? Si................. .......................................................................... No................. ......................................................................... 36. Si la respuesta es si, ¿Me permite dar su nombre y número de telėfono a alguien para hacer seguimiento con usted? (SI LA RESPUESTA ES SI, ANOTE EN EL LIBRO DE REUNIONES DE CASA) Si................. .......................................................................... No................. ......................................................................... 37. En escala de 1 a 5, donde 1 significa NO ME GUSTARIA y 5 significa ME GUSTARIA, le gustaría recomendar las reuniones de casa con información de salud a sus amigos, familiares o vecinos? (LEA LOS NUMEROS Y CIRCULE EL NUMERO SELECCIONADO) No me gustaría 1 38. Me gustaría 2 3 4 5 ¿Hay algo más que a usted le gustaría añadir acerca de su experiencia en la reunión de salud oral en casa? (PREGUNTA ABIERTA; ANOTE LA RESPUESTA) ________________________________________________________________________________________________________________________ Hora de finalizada la entrevista: _______________ 100 Appendix B.1: Focus Group Questions Note: The things in brackets are not to be read out loud, they are reminders to help guide you through the focus group discussion. [GIVE INTRODUCTION] [Opening Question (ask all participants to respond – i.e. go around the circle for responses)] 1. Give your first name, how many children you have, and tell us quickly, your favorite activity to do with your kids. [Transition into topic questions] [Introductory Question] 2. What comes to mind when you think about healthy teeth? [Assistant moderator writes down people’s different ideas of things that contribute to healthy teeth and the GOAL is to get array of different ideas. Do not call on people, but use fingers and eyes] [Transition Questions] 3. Think back to when you participated in the oral health program. What was your first impression? 4. Before you participated in the program what practices did your children use to keep their teeth clean? 5. Now that you’ve participated in the program what practices do your children use to keep their teeth clean? 101 a. [If oral health practices have changed then PROBE] How do you feel about these different/new practices your children do? b. [PROBE] Have you noticed a difference in your child’s attitude about oral health? 6. Are there any different practices that parents from your country of origin do to keep their children’s teeth healthy? If so, what are they? OR What practices do people from your country of origin do to keep their children’s teeth healthy? [Really try to draw out different ideas on this question if possible] 7. a. What are some things that get in the way of keeping your children’s teeth healthy? [PROBE] They could be things that are in your control and/or not in your control. Write them on a piece of paper. These lists are anonymous. You do not need to write your name on the paper. i. [Wait for about 3-5 minutes and THEN tell them] Now, place the paper in this bowl and _______(either Ernesto or Odette) will jot down these ideas. [Assistant moderator passes around bowl and collects participant’s responses] [Have assistant moderator compile list on a piece of butcher paper. Have participants expand on the ideas listed that are unique/surprising – I will provide you with a list/ideas of things that we may see and not want to necessarily focus on.] 102 [Key Questions] 8. How do these things [listing 3 things that are unique/surprising factors] : ____, _____, and ______ get in the way of keeping your children’s teeth healthy? a. [PROBE] Are there any things listed that you disagree with? 9. Is there anything listed that the program helped you with? If so, how? 10. Is there anything from the list that still gets in the way of keeping your children’s teeth healthy? a. [PROBE] How do these things get in the way? b. [PROBE] What could be done to overcome these? 11. Of the three things we’ve been focusing on: _____, _____, _____, how would you incorporate these issues in an oral health program? First, let’s talk about _____. [Discuss their ideas, then after a few minutes, move to the next topic, then finally move on to the last topic] [Ending Questions] 12. Our big picture goal is to understand what gets in the way for you, as parents, in keeping your children’s teeth healthy, and how we can help with these issues. That being said is there anything you would like to add that we missed? [CLOSING] Thank you for your participation. Your ideas will help others like you who participate in the oral health program in the future. 103 Appendix B.2: Focus Group Questions in Spanish Borrador de Preguntas Para Grupo de Enfoque Nota: lo que se encuentra en paréntesis cuadrados no se debe de decir en fuerte, son guías para ayudar a moderar al grupo de enfoca. [Dar Introducción] [Pregunta de Apertura (se pide que todos los participantes respondan, por ejemplo, ir en círculo para que todos den respuestas.)] 1. Díganos su nombre, número de hijos y, de una manera concisa, la actividad que más le gusta hacer con sus hijos. [Transición a preguntas del tópico] [Preguntas de Introducción] 2. ¿Qué es lo que se le viene a la mente cuando piensa en dientes saludables? [Moderador Asistente escribe las diferentes ideas que contribuyen a dientes sanos y la meta es tener una gama de ideas diferentes. No se le llama a personas, pero se usan ojos y dedos.] [Preguntas de Transición] 3. Pensando en el tiempo en el que participó en el programa de salud oral, ¿Cuál fue su primera impresión? 4. ¿Antes de que participara en el programa, que practicas usaban sus hijos para mantener dientes saludables? 104 5. ¿Ahora que ya participo en el programa, que practicas usan sus hijos para mantener dientes saludables? a. [Si las practicas han cambiando, hacer sondeo] ¿Cómo se siente acerca de estas nueves practicas que sus hijos hacen? b. ¿Ha notado alguna diferencia en la actitud de sus hijos con respecto a la salud oral? 6. ¿Hay prácticas diferentes que los padres de su país de origen usen para mantener dientes saludables en sus hijos? ¿Cuáles son? Ó ¿Qué practicas usa la gente de su país de origen para mantener los dientes de sus hijos saludables? 7. a. ¿Qué factores hacen que sea difícil mantener la salud oral de sus hijos? Sondeo: Estos factores pueden estar bajo su control y/o no estar bajo su control. Escriba sus respuestas en un papel y en un momento los compartiremos unos con otros. Estas respuestas son anónimas, no necesita escribir su nombre. i. [Esperar por 3-5 minutos y después pedirles] Ahora, por favor pongan sus respuestas en este platón y ____ (Ernesto u Odette) escribirán rápidamente estas ideas. [Moderador asistente pasa el platón y recolecta las respuestas] 105 [El moderador asistente escribirá estas ideas en un papel. Haz que los participantes comenten sobre las ideas que son únicas o sorprendentes. Yo voy a darles una lista de cosas que queremos o no queremos ver en la lista] [Preguntas Clave] 8. ¿Cómo hacen estos factores (mencionar 3 factores que fueron únicos o sorprendentes): ___, ____ y ___, sea difícil mantener la salud oral? a. Sondeo: ¿hay algo en la lista con lo que usted no esta de acuerdo? 9. ¿Hay algo en la lista con lo que el programa le ayudo? 10. ¿Qué de lo mencionado sigue interfiriendo con que sus hijos tengan dientes sanos? a. [Sondeo] ¿Cómo interfieren estas cosas? b. [Sondeo] ¿Qué se puede hacer para sobrepasar estas dificultades? 11. ¿De las tres cosas en las que nos hemos enfocado: ___, ___ y____, como las incorporaría usted en un programa de salud oral? Primero, hablemos de ___. [Se discuten esas ideas y en un par de minutos se pasa al siguiente tema, y luego al último.] [Preguntas Finales] 12. Nuestra meta en el panorama completo es entender que dificultades usted encara como padre en mantener la salud oral de sus hijos, y como podemos tratar con ellas mejor. ¿Habiendo dicho esto, hay algo que nos haya faltado? [Clausura] Gracias a todos por su participación. Sus ideas ayudaran a otras personas como usted que participaran en el programa de salud oral en el futuro. 106 Appendix C – THT Data from Phone Survey Oral Health Service Utilization When did you last take your child to the dentist? N Percent Within the last six months 76 53.9% More than six months ago 59 41.8% 6 4.3% 141 100.0% My child has never visited a dentist Total Why did you decide to take your child to the dentist? N Due for a check up Percent 115 87.8% Teeth/mouth hurt 6 4.6% School/day care recommended or required 5 3.8% Health care provider recommended 1 0.8% Health educator at home meeting recommended 1 0.8% Other Reason 3 2.3% 131 100.0% Total What barriers have you experienced in taking your child/children to a dentist? Percent of total N Lack of dental insurance 37 26.4% Language differences 22 16.5% Not being able to find a dentist you are comfortable with 21 15.6% Your being too busy 21 15.3% Inconvenient dental appointment hours 18 13.3% Lack of accessible dentists 14 10.3% Transportation to/from the dentist 11 7.4% 107 On a scale of 1 to 5, with 1 being not at all helpful and 5 being extremely helpful, how helpful was the oral health program in providing you with information or resources to overcome these barriers? N Percent 1 - Not at all helpful 1 1.7% 2 0 0.0% 3 1 1.7% 4 8 13.8% 5 - Extremely helpful 48 82.8% Total 58 100.0% Knowledge about Oral Health What is one thing you remember from the home meeting on oral health? N Percent Brushing 155 92.3% Flossing 111 66.1% Communication with Dentist 67 39.9% Healthy Eating 75 44.6% 168 100.0% Total Oral Health Practices How often does your child/children brush his/her teeth each day (with or without your help)? N Percent After every meal 5 3.8% Three times/day 19 14.5% Two times/day 96 73.3% Once a day 11 8.4% 131 100.0% Total 108 How often does your child/children floss his/her teeth (with or without your help)? N Percent At least once a day 58 44.3% About 5 times/week 2 1.5% About 3 times/week 25 19.1% About 1 time/week 9 6.9% About 1 time/month 5 3.8% Never 32 24.4% Total 131 100.0% How often does your child/children eat fruits and vegetables? N Percent At least three times a day 61 46.9% About 1 time/day 43 33.1% About 3 times/week 21 16.2% About 1 time/week 3 2.3% About 1 time/month 1 0.8% Never 1 0.8% 130 100.0% Total Oral Health Education Delivery Model On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the oral health education you received? N Percent 1 - Poor 0 0.0% 2 0 0.0% 3 1 0.6% 4 21 12.8% 5 - Excellent 142 86.6% Total 164 100.0% 109 On a scale of 1 to 5, with 1 being VERY LITTLE KNOWLEDGE and 5 being A LOT OF KNOWLEDGE, how would you rate the health educator’s knowledge about oral health? N Percent 1 - Very little knowledge 0 0.0% 2 0 0.0% 3 1 0.6% 4 19 11.7% 5 - A lot of knowledge 143 87.7% Total 163 100.0% On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the COMMUNICATION SKILLS of the health educator? N Percent 1 - Poor 0 0.0% 2 0 0.0% 3 1 0.6% 4 18 11.0% 5 - Excellent 144 88.0% Total 163 100.0% On a scale of 1 to 5, with 1 being POOR and 5 being EXCELLENT, how would you rate the overall EFFECTIVENESS of the health educator? N Percent 1 - Poor 0 0.0% 2 0 0.0% 3 1 0.6% 4 15 9.3% 5 - Excellent 145 90.1% Total 161 100.0% 110 Bibliography "American Community Survey - ACS Demographic and Housing Estimates: 2006." Factfinder.census.gov. 2006. U.S. Census Bureau. 8 Dec. 2008. Atchison, Kathryn A. "Understanding health behavior and perceptions." Dental Clinics of North America 47 (2003): 21-39. Theclinics.com. <http://www.dental.theclinics.com/article/PIIS0011853202000514/fulltext# BIB6>. Bertness, Jolene, and Katrina Holt. Promoting Awareness, Prevention Pain: Facts on Early Childhood Caries (ECC). Washington D.C.: National Maternal and Child Oral Health Resource Center, 2004. Butani, Yogita, Jane A. Weintraub, and Judith C. Barker. "Oral health-related cultural beliefs for four racial/ethnic groups: Assessment of the literature." BioMed Oral Health Central 8 (2008): 8-26. "Cumin seed, Powder." 2005. Monterey Bay Spice Company. 10 May 2009. Flores, Glenn. "Barriers to Health Care Access for Latino Children: A Review." Family Medicine 30 (1998): 196-205. Flores, Glenn, Elena Furentes-Afflick, and Et al. "The Health of Latino Children: Urgent Priorities, Unanswered Questions, and a Research Agenda." The Journal of the American Medical Association 288 (2002): 82-90. Haden, N. K., Frank A. Catalanotto, Charles J. Alexander, and Al Et. "Improving the Oral Health Status of All Americans: Roles and Responsibilities of Academic Dental Institutions." Journal of Dental Education 5th ser. 67 (2003): 563-83. Hayes-Bautista, David E., Mariam I. Kahramanian, Erin G. Richardson, Paul Hsu, Lucette Sosa, Cristina Gamboa, and Robert M. Stein. "Rise and Fall of Latino Dentist Supply in California: Implications for Dental Education." 111 Journal of Dental Education 71: 227-34. 2007. 18 Mar. 2009 <http://www.jdentaled.org/cgi/reprint/71/2/227>. "Herbal Ways of Cleaning Teeth." AyurvedicCure.com. 14 Jan. 2009. 8 May 2009. Israel, B. A., E. A. Parker, and A. B. Becker. "Review of community-based research: Assessing partnership approaches to improve public health." Annu Rev Public Health 19 (1998): 173-202. Krueger, Richard A. Focus Groups: A Practical Guide for Applied Research. Ed. Mary Anne Casey. 4th ed. Thousand Oaks: Sage, 2009. McEwen, Bruce S., and Teresa Seeman. "Protective and Damaging Effects of Mediators of Stress: Elaborating and Testing the Concepts of Allostasis and Allostatic Load." Annals of the New York Academy of Sciences 896 (1999): 30-47. Wiley InterScience. 18 Mar. 2009 <http://www3.interscience.wiley.com/cgibin/fulltext/120755487/PDFSTART>. Milgrom, Peter, Lloyd Mancl, Barbara King, and Philip Weinstein. "Origins of Childhood Dental Fear." Behav. Res. Ther. 33 (1995): 313-19. 25 May 2009. "Oral Health And Your Body." Simple Steps To Better Dental Health. 2002. Aetna Dental Plans, Columbia University. 2 Dec. 2008 <http://www.simplestepsdental.com/ss/ihtss/r.wsihw000/st.31848/t.31848/ pr.3.html>. Otto, Mary. "For Want of a Dentist." The Washington Post: Pr. George's Boy Dies After Bacteria From Tooth Spread to Brain 28 Feb. 2007: B01. Ramos-Gomez, Francisco, Gustavo D. Cruz, Maria R. Watson, Maria T. Canto, and Augusto E. Boneta. "Latino oral health: A research agenda toward eliminating oral health disparities." The Journal of the American Dental 112 Association 136 (2005): 1231-240. Reedy, Aimee. Evaluation of the Wellness Access and Education Program's Oral Health Education Services. Rep. no. 1. Vol. 1. 2009. Riportella-Muller, Roberta, Maija L. Selby-Harrington, Lenora A. Richardson, Patricia L. Donat, Kathryn J. Luchok, and Dana Quade. "Barriers to the Use of Preventive Health Care Services for Children." 111 (1996): 71-77. Smedley, Brian D., Adrienne Y. Stith, and Alan R. Nelson. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. National Academies P, 2003. "State & County QuickFacts." 2007. U.S. Census Bureau. 24 May 2009 <http://www.quickfacts.census.gov>. Tashakkori, Abbas, and Charles Teddlie. Handbook of Mixed Methods in Social & Behavioral Research. Sage, 2002. Thompson, Damon. "First-Ever Surgeon General's Report on Oral Health Finds Profound Disparities in Nation's Population." Office of the Surgeon General. 25 May 2000. U.S. Department of Health & Human Services. 8 Dec. 2008 <http://www.hhs.gov/>. United States. Center for Disease Control. MMWR. 30 Nov. 2001. CDC. 24 May 2009 <http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5021a1.htm>. United States. Center for Disease Control. Prevention and National Center for Health Statistics. 2007 Health, United States, 2007 with Chartbook on Trends in the Health of Americans. 2007. 11 Mar. 2009 <http://www.cdc.gov/nchs/data/hus/hus07.pdf#076>. United States. Department of Health and Human Services. Office of Inspector General. Children?s Dental Services Under Medicaid: Access and Utilization. By June G. Brown. 113 United States. National Academy for State Health Polocy. Kaiser Commission on Medicaid and the Uninsured. Filling an Urgent Need: Improving Children?s Access to Dental Care in Medicaid and SCHIP. By Shelly Gehshan, Andrew Snyder, and Julia Paradise. 2008. Wallerstein, Nina B., and Bonnie Duran. "Using Community-Based Participatory Research to Address Health Disparities." Health Promotion Practice 7 (2006): 312-23. Sage Pulications. 7 June 2006. Sage. 12 Mar. 2009 <http://hpp.sagepub.com>. Watson, Maria R., Alice M. Horowitz, Isabel Garcia, and Maria T. Canto. "A Community Participatory Oral Health Promotion Program in an Inner-city Latino Community." Journal of Public Health Dentistry 61 (2001): 34-41. Wolfe, D.D.S., Bill. "Aloe Vera: An Ancient Plant for Modern Dentistry." Dr. Wolfe's Naturally Enhanced Toothpaste. 10 May 2009. "Why Is Oral Health Important." First Smiles Oral Health. 2004. 11 Dec. 2008 <http://www.first5oralhealth.org/default.asp>. U.S. Department of Health and Human Services. Healthy People 2010. 2nd ed. With Understanding and Improving Health and Objectives for Improving Health. Dec. 2001, Table 21-1a. 114