Hematology Billing Procedures Policy | Medicare Compliance
advertisement

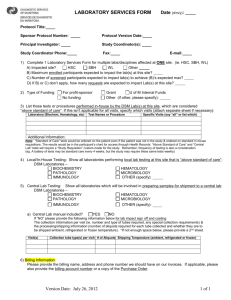
DEPARTMENT: Regulatory Compliance Support PAGE: 1 of 4 EFFECTIVE DATE: January 1, 2007 POLICY DESCRIPTION: BILLING - Hematology Procedures REPLACES POLICY DATED: 1/16/98, 3/1/99, 8/1/02, 2/15/03 (GOS.LAB.002); 3/6/06 REFERENCE NUMBER: REGS.LAB.002 SCOPE: All Company-affiliated facilities performing and/or billing laboratory services. Specifically, the following departments: Business Office Admitting/Registration Finance Administration Revenue Integrity Nursing Laboratory Health Information Management Utilization/Case Management Service Centers PURPOSE: To establish guidelines for billing hematology services in accordance with Medicare, Medicaid, and other federally-funded payer requirements. POLICY: Hematology tests billed to a federally-funded program must be based on a written order and be medically necessary. Hematology components will be bundled to the panel level when all of the tests in the panel are ordered and performed. Hematology tests which include all components of a panel must not be “unbundled” into individual procedures. Repeated hematology procedures, including overlapping components of panels, may be billed when the tests are medically necessary, which is indicated by reporting the 91 modifier. The 91 modifier may only be reported when in the course of treating a patient, it is necessary to repeat the same laboratory test on the same day to obtain subsequent test results. This modifier may not be reported when tests are rerun to confirm initial results; due to testing problems with specimens or equipment; or for any other reason when a normal, one-time, reportable result is all that is required. This modifier may not be used when other code(s) describe a series of test results (e.g., glucose tolerance tests, evocative/suppression testing). If a payer does not recognize/accept the 91 modifier, repeated laboratory tests may not be billed. PROCEDURE: The following steps must be performed when billing hematology services to Medicare and other federally-funded programs. IMPLEMENTATION 1. Facility personnel must review and verify applicable entries are present in the facility chargemaster and appropriately tied to the related Laboratory and Order Entry masterfiles/dictionaries as follows: a. Assign CPT /HCPCS codes listed below and attach revenue code 305 in accordance with the Company Standard Laboratory Chargemaster. 1/2007 DEPARTMENT: Regulatory Compliance Support PAGE: 2 of 4 EFFECTIVE DATE: January 1, 2007 POLICY DESCRIPTION: BILLING - Hematology Procedures REPLACES POLICY DATED: 1/16/98, 3/1/99, 8/1/02, 2/15/03 (GOS.LAB.002); 3/6/06 REFERENCE NUMBER: REGS.LAB.002 Components of Hematology Panels: CPT Code AMA Description 85004 Blood count; automated differential WBC count 85013 Blood count; spun microhematocrit 85014 Blood count; hematocrit (Hct) 85018 Blood count; hemoglobin (Hgb) 85041 Blood count; red blood cell (RBC) , automated 85048 Blood count; leukocyte (WBC), automated 85049 Blood count; platelet, automated Hematology Panels: CPT/HCPC Code AMA Description 85025 Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC and platelet count) and automated differential WBC count 85027 Blood count; complete (CBC), automated (Hgb, Hct, RBC, WBC and platelet count) G0306 Complete CBC, automated (HgB, Hct, RBC, WBC, without platelet count) and automated WBC differential count G0307 Complete CBC, automated (HgB, Hct, RBC, WBC; without platelet count) b. When all components of a panel are present, the components must be bundled to the appropriate panel. Fewer components may be ordered as a “panel” but must be billed as individual components, e.g., H & H (Hemoglobin and Hematocrit). 2. Business Office/Service Center personnel must verify that edits are present in the electronic billing system which: a. Bundle components to the panel level when all components are charged on the same patient on the same date of service. b. Identify outpatient claims for federally-funded payers which include repeated hematology panels and/or components performed for the same patient on one date of service. 3. Laboratory and Business Office/Service Center personnel must educate all staff associates responsible for ordering, charging, or billing laboratory services on the contents of this policy. 4. Monitoring activities should be completed in accordance with the Billing – Monitoring Policy, REGS.GEN.001. DAILY 1. It is recommended but not required that laboratory personnel review daily charge reports (e.g., Ancillary Charge Report, NPR charge reports, etc.) to verify compliance with this policy as 1/2007 DEPARTMENT: Regulatory Compliance Support PAGE: 3 of 4 EFFECTIVE DATE: January 1, 2007 POLICY DESCRIPTION: BILLING - Hematology Procedures REPLACES POLICY DATED: 1/16/98, 3/1/99, 8/1/02, 2/15/03 (GOS.LAB.002); 3/6/06 REFERENCE NUMBER: REGS.LAB.002 follows: a. Duplicate hematology components which are not medically necessary are not billed to federally-funded programs. b. Repeated hematology panels and components are billed to federally-funded programs only when medically necessary. c. Hematology components are bundled to the appropriate panel defined as follows: 85025 85004 85013(14) 85018 85041 85048 85049 85027 85013(14) 85018 85041 85048 85049 G0306 85004 85013(14) 85018 85041 85048 G0307 85013(14) 85018 85041 85048 Any exceptions noted on the daily charge reports should be corrected on the individual patient accounts. This will ensure that your accounts receivable system remains updated with actual billing data. 2. Business Office/Service Center personnel must review electronic billing edit / error reports daily and perform the following: a. Bundle hematology components into the appropriate panel when all components are present. b. Identify presence of more than one hematology panel and determine if documentation is present to support medical necessity of repeated panels. i. Append the 91 modifier to repeated hematology procedures which are medically necessary. ii. Eliminate repeated tests/panels which are not medically necessary. Modify number of units and related charges in the electronic billing vendor system to reflect the appropriate charge and CPT for the panel being billed. c. It is recommended but not required to modify the number of units and related charges in the Accounts Receivable system to match the corrected claim in electronic billing system. (Note: Utilize ancillary charge codes rather than correcting claims with adjustment codes. Corrections made subsequent to final bill should be processed through your patient accounting system late charge cycles.) This will ensure that your accounts receivable system remains updated with actual billing data. The Facility Ethics and Compliance Committee is responsible for implementation of this policy within the facility. Special Considerations: DO NOT CHARGE FOR services reported as a result of a calculation. 1/2007 DEPARTMENT: Regulatory Compliance Support PAGE: 4 of 4 EFFECTIVE DATE: January 1, 2007 POLICY DESCRIPTION: BILLING - Hematology Procedures REPLACES POLICY DATED: 1/16/98, 3/1/99, 8/1/02, 2/15/03 (GOS.LAB.002); 3/6/06 REFERENCE NUMBER: REGS.LAB.002 DO NOT CHARGE FOR both manual and automated differential on the same patient for the same date of service. When a physician specifically orders a CBC with automated differential, the lab can only bill CPT code 85025, even if a reflex manual differential is performed as a result of an approved reflex test. Medicare considers the reflex to the manual differential as part of the steps necessary to complete the physician's order. It would not be appropriate to bill for the reflex test even if your instrument flags the test and you also perform a manual differential. For additional information regarding reflex test refer to REGS. LAB.010 – Reflex Orders. DEFINITION Encounter: Each date of service. REFERENCES: Medicare Reimbursement Manual for Clinical Laboratory Issues; National Edition, 1997. Washington G-2 Reports, Washington, D.C. Medicare Hospital Manual, U.S. Dept. of Health and Human Services, CMS – Pub. 10 thru T703, Rev. 7/97. Billing Procedures Section 437. U.S. Department of Justice, Subpoena dated December 27, 1996 (Exhibit A regarding: Outpatient Laboratory Billings To Medicare and Medicaid Programs) American Medical Association Physician’s Current Procedural Terminology CPT American Medical Association’s CPT Changes 2003 – An Insider’s View 1/2007