The Role of Home Carers in the Management of Medicines
advertisement

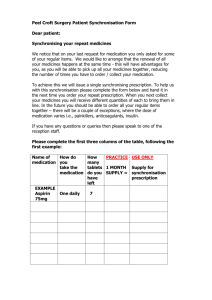
The Role of Home Carers in the Management of Medicines Highland Council & NHS Highland Warning – Document uncontrolled when printed Policy Reference: Date of Issue: July 2007 Prepared by:A. MacRobbie & B. Nott Date of Review: July 2009 Lead Reviewer:A MacRobbie & B Nott Version:3 Authorised by: Chief Officers Group Date: CONTENTS Page 1. INTRODUCTION 2 2. FLOWCHART 3 3. ASSESSMENT OF CLIENT MEDICATION NEED 6 4. LEVEL 2 ASSISTANCE 6 5. LEVEL 3 ASSISTANCE 7 A. B. C. D. E 7 7 8 8 8 Responsibility/Liability Consent Medication Chart Medication Administration Form Tasks Which May be Undertaken by Home Carers after Assessment and with Appropriate Additional Training from Healthcare Workers 6. TASKS WHICH MUST NOT BE COMPLETED BY HOME CARERS 8 7. DESCRIPTION OF TASKS WHICH MAY BE UNDERTAKEN BY HOME CARERS 9 8. SERVICE USERS WHO ARE UNABLE TO GIVE INFORMED CONSENT 12 9. GENERAL INFORMATION – HOW THE PHARMACIST CAN HELP 12 10. TRAINING 12 APPENDIX 1 Checklist for Assessing Client Medication Management Need APPENDIX 2 Emergency Procedures & Form APPENDIX 3 Medication Chart & Record of Medication Administration APPENDIX 4 Medication Permission Form (for level 3 service user) APPENDIX 5 Medicines Disposal Form APPENDIX 6 Client Information Leaflet APPENDIX 7 Information Leaflet for Health & Social Care Workers (Level 3) APPENDIX 8 Information Leaflet for Medication Compliance and Monitored Dosage Systems (Level 2) 1. INTRODUCTION The aim of the Home Care Service is to enable service users to choose to continue to live in their own homes. The range of care tasks which Home Carers are required to undertake will be from household to personal care. These tasks supplement self care and the support available from informal carers. The majority of service users are able to take responsibility for their own medicine management and it is important that people are supported to maintain as many self-care skills as possible. However service users may sometimes require assistance with medication. The assistance offered must be tailored to an individual’s needs and carried out in a professional manner by properly trained staff with the correct degree of competence. These guidelines aim to ensure that any assistance given with medication is carried out in a safe professional manner, within the knowledge and competence of Home Carers. It is imperative that Home Carers observe the guidance set out in this document. Home Care staff must feel confident to perform tasks correctly and safely. Home Care staff should never be involved in any medicine management task unless authorised to do so by the Home Care Senior/Manager. Home Care staff must not perform any activity out with the guidelines. Medicines Administration by Home Carers in the Community Flow Chart Identification of Client Medicine Management Problem from e.g. single shared assessment (SSA) ( by Home Carer, Care Manager, Community Nurse, GP, Community Pharmacist) Referral to Primary health care team for needs assessment GP Practice to assess level of assistance required with medicines and full medication review e.g. Discontinue unnecessary medication, review timing of administration to assist with compliance, synchronise prescription supply quantities etc Level 1 Level 2 Level 3 Level 4 Able to manage own medicines - no problems Able to manage medicines with minimal assistance (ie collection of prescriptions by home carer, return of unnecessary medicines by home carers to pharmacy) Require medicines to be managed and administered by others Require assistance with medication beyond scope of home carer e.g. injections Record outcome and planned next medication review date GP Practice to Update practice patient record, including medication record Communicate with Community Pharmacist to YES updateYESv medication records and to assist patient with appropriate compliance measures Communicate (written)with Senior Home Care officer Record outcome and planned next review date GP and Senior Home Care Officer communicate regarding agreement for medicines administration by home carer - Senior home care officer(SHCO) to update register of level 3 clients, flag Care First system and activate communication cascade to key stakeholders NO YES - - - - - GP to identify patient's preferred community pharmacy (all dispensing requires to go through one pharmacy for the service to operate effectively) GP to update and flag practice patient record (including medication record) and advise community nursing staff GP to include information on patient emergency summary to identify to unscheduled care additional records if prescribing or to flag if hospital admission is required SHCO to Communicate with Community Pharmacist to confirm client status and to update records SHCO to advise Community Nursing team Monitor for change in circumstances and/or review date for client/patient reached If no change in assessment - record, communicate outcome to stakeholders and continue If change in circumstances - commence from start of pathway Record outcome and planned next review date - GP Practice to Communicate with community nursing team - GP to advise SHCO Hospital Admission/Discharge of Previously Identified Level 3 Medication Patients Hospital admission - - Ward staff to identify if relative/carer involved in medicines administration and request if patient has SSA and obtain copy Flag PAS (Patient Administration System) system with 'Level 3 medication patient' if not already done Acute Hospital Discharge Community Hospital Discharge - - - Hospital Pharmacy process discharge prescriptions for both Acute Hospital and Community Hospitals PAS system flagged to identify level 3 patients Home care service (SCHO) require to be advised of discharge and medication needs by hospital social worker (new, temporary or ongoing, include level 2 patient needs ie prompting, compliance devices etc.) or ward staff as appropriate. 48 working hours notice required of changes. - Will be included in list of destination for register of level 3 patients Flag PAS system to identify level 3 patients Home care service (SCHO) require to be advised of discharge and medication needs (new, temporary or ongoing) - for RNI may be done by Raigmore hospital social worker or ward staff as appropriate. 48 working hours notice required of changes. Medication dispensed by hospital pharmacy department Medication dispensed from community pharmacy on GP10 or HBP prescription Hospital discharge (IDL) - IDL information should match discharge medication labels Quantity of medicine supplied is ideally for a 28day period IDL copy sent to GP must record this is a level 3 patient for accuracy checking (so that copy of IDL can be sent to community pharmacy to trigger generation of medication chart from CP) Hospital discharge (IDL) - - IDL information should match discharge medication labels and checked by GP. IDL must record this a level 3 patient Quantity of medicine supplied is ideally for a 28day period IDL copy sent to community pharmacy by community hospital staff to trigger generation of medication chart from CP) GP to send checked copy of IDL marked Level 3 patient to community pharmacy with request for medication chart from community pharmacy for home carer CP prepares medication chart for home carer Hospital Discharge - GP10 or HBP script must record this as a Level 3 patient - script sent to CP for dispensing Role and Responsibilities for team Members involved with a Level 3 medication patient Senior Home Care Officer Responsibilities - liaison between home carer and health care team - obtainRole client consent for home carer medicine administration and Responsibilities for team Members involved with a Level 3 medication patient - authorises home carers to administer medicines and maintains supplies and storage of documentation (include carer ID) - trains and supports home carers - monitors and feeds into systems review - Hold, maintain and keep stakeholders informed of changes to register of level 3 patients Community Prescribers'/Practice responsibilities - advise senior home care officer of any changes in medication - advise community pharmacist of any changes in medication - all medicines prescribed with full directions. As required medicines need a maximum dose stated. - completes Incapacity forms if required - flagging clients with unscheduled care service and on own GP system - ensuring prescriptions/IDL identify patient as Level 3 medication patient when sending to community pharmacy - advise community nursing staff Community Pharmacist responsibilities - prepare and maintain medication record chart - update patient medication records including flag ‘level 3’ patient - Flag labels on patients medicine bottles with ‘level 3’ patient if needed - advise and support home carer on medicine related issues - communicate with prescribers and other stakeholders as appropriate - if available assist with collection/delivery service Home Carer Responsibilities - Orders, collects, arranges appropriate storage e.g. putting refrigerated items in fridge and administers medicines and maintain records of administration. - Arranges for disposal of medicines if required. - advise senior home care officer/GP practice of possible side effects/difficulties Unscheduled Care Responsibilities identifies patient on system as a level 3 patient when advised by GP practice - ensure GP, home care manager and Community Pharmacist advised of medication changes for level 3 patients - records medicines administration/prescription changes in home care documentation - advises hospital of Level 3 medication needs if patient admission required Community Nursing responsibilities - use of home care documentation for administration of medicines if necessary e.g. where home carer usually administers medication - liaise with senior home care officer to discuss administration issues where health care advice required (as indicated in policy) - administer medicines by routes identified as inappropriate for home carers to administer where required Family/other carer responsibilities - Use home care documentation if administering medications - Communicate concerns or changes to SHCO or GP Hospital responsibilities - obtain information of level 3 status by ward staff asking who look after patients medication at home or from single shared assessment - flag PAS system if not already done - Ward discharging nurse ensures IDL matches dispensed medication and if community hospital copy sent to community pharmacist - liaise with relevant stakeholders at discharge e.g. social work for home carer, ward staff for GP/Community Pharmacy/Community nurse Client responsibilities - consent to home carer administration of medicines - provide any equipment e.g. locked medicine cabinet necessary for effective management of medication 3. ASSESSMENT OF SERVICE CLIENT NEED Assessment of service client need is key to the whole process. This will identify what, if any, assistance is required. Assessment of need is the responsibility of a member of the GP Practice team and may not be carried out by the Home Carer Service. Assessment of need must be carried out in a structured manner using for example the checklist (Appendix 1.) The result of the assessment will be one of the following: Able to manage their own medicines (Level 1 user) These service users will retain control of their medication, preserving their independence and choice. This should be encouraged wherever possible. Able to manage their medicines with minimal assistance (Level 2 User) These service users will retain maximum control of their medicines and will require minimal input. The service user will retain overall responsibility for the management of their medicines. Assistance required (Level 3 User) These service users are unable to manage their medicines themselves. They will not retain responsibility for the management of medicines. The service user or their carer must agree to assistance being given. Assistance required beyond the knowledge and skills of Home Carers (Level 4 user) Any procedure other than those detailed for level 2 and level 3 users should only be performed by competent persons with medical knowledge and skill. The results of this assessment must be recorded and made available to all who will be involved in the care of the service user. Reassessment may be necessary at any time to take account of changes in the medication needs of the service user. Any change in medication needs should be notified to the Home Care Senior/Manager by the GP Practice Team. 4. LEVEL 2 ASSISTANCE The level 2 service user is responsible for the management of his/her own medicines but may, after assessment by the Home Care Senior/Manager, including risk assessment, be offered help with the following tasks. Ordering prescriptions from the medical practice at the request of the service user. The service user must indicate the medicines, dosages and quantities to be ordered. Collecting prescriptions from the medical practice and delivering to the pharmacy. Collecting medicines from the pharmacy. Confirming the reading of medicine labels. Opening containers such as medicine bottles, removing tablets/capsules from strip packaging. Assistance with opening compliance aids may only be given if these have been dispensed by a Pharmacist. Administration, where agreed by Senior Home Care Officer (SHCO), of short term temporary medications e.g. post surgical eye drops, where client is otherwise able to manage their own medication. Returning unwanted medicines to the pharmacy at the request of the service user. The service user must indicate those medicines to be returned and the medicines disposal form (Appendix 5) be completed. Home carers should ascertain which pharmacy is preferred by the service user and use this pharmacy at all times (see how the pharmacist can help). The home carer must not fill compliance aids, e.g. dosette boxes. All requests for assistance other than those listed above and agreed by Home Care Senior/Manager must be reported to the Home Care Senior/Manager. GP Practices will be informed by the Home Care Senior/Manager of service users being supported at level 2 Mismanagement of Medicines If the Home Carer suspects that a service user is not taking his/her medicines as prescribed they should discuss their concerns with the service user and try to support them to take their medicines appropriately. If this fails the Home Carer should inform the Home Care Senior/Manager who will in turn contact the appropriate GP Practice team member in writing to ask for a re-assessment. 5. LEVEL 3 ASSISTANCE Before assistance can be given to a service user at level 3, a review of medicines must be undertaken by the GP Practice team or pharmacist. All medicines must be prescribed with specific directions – the use of the term ‘as directed’ must be avoided. A. Responsibility/Liability Home Carers may only give medication to service users in their own homes after authorisation by the Home Care Senior/Manager as an agreed task on the Care Plan (see later). Procedures to be followed in emergency situations are set out in Appendix 2 to these guidelines e.g changes to medication, hospital discharge and verbal instructions. As a general rule, Home Care staff should be able to provide assistance with oral medication, some skin care and eye/ear/nasal preparations. Individual needs may also be provided following guidance and demonstration with the individual service user (see later). The Home Carer Service has the responsibility for ensuring that Home Carers assisting with medication have had proper training and receive appropriate support and that medication administration charts (Appendix 3) are completed. Home Carers will only assist with medication if a Medication Permission Form (appendix 4) has been signed. If the Home Carer has any concerns about any aspect of a service client’s medication regime, she/he must notify the Home Care Senior/Manager immediately. It is the responsibility of the service user to purchase any compliance aids or locked medicine cabinet necessary for the proper management of their medication. B. Consent Following an Assessment of Need, the Senior Home Care Officer/Manager will discuss medication issues with the service user and/or his/her representatives, agree the task to be undertaken and complete the Medication Permission Form. (See Appendix 4). The Senior Home Care Officer/Manager will liaise with all others providing support to the service user (i.e. formal and informal carers, health care team) so that each party is aware of the input being provided. It will be emphasised that, in the interests of safety, any other carers involved in administration of medication must agree to use the medication administration form. This will be documented in the Care Plan. Any difficulties will be reported by the Home Care Senior/Manager to the GP Practice. C. Medication Chart Responsibility for assisting service users with medication at Level 3 will only be taken after the completion of a Medication Chart. (See Appendix 3). This responsibility will be undertaken by the pharmacist except in areas where dispensing practices are in place and the GP practice team will undertake this. A review of medication by a member of the GP Practice team, which could include the pharmacist, should take place to ensure that all medication continues to be indicated. The Home Care Senior/Manager will be advised of any changes to the medication chart and it will be his/her responsibility to ensure that any new task is within the competency of the Home Carer. D. Medication Administration Form Senior Home Care Officers/Managers will be responsible for ensuring Home Carers complete the Medication Administration Forms (See appendix 4), for monitoring record-keeping and supporting and supervising staff. Home Carers will be responsible for following instructions from the Medication Chart and for recording actions showing date and time of actions in the Medication Administration Form. Any problems encountered with the administration of medication must be recorded on the reverse of the Administration Record under the headings “Date”, “Problem”, “Actions Taken” and “Outcome” Medication Administration forms will be removed from the service user’s home on a monthly basis by the Home Care Senior/Manager and a new sheet supplied. Old medication charts will be stored in the service users file. E. Tasks Which May be Undertaken by Home Carers after Assessment and with Appropriate Additional Training from Healthcare Workers (Level 3) 6. Changing catheter leg bag, where this does not disturb the catheter Changing colostomy bags Changing dressings, simple dry dressings, covering a minor wound with sticking plaster or as a first-aid measure until medical advice is sought Application of creams, ointments or lotions Eye drops, eye ointments Ear drops, ear ointments Nasal drops, nasal ointments PEG feeding Inhalation devices, nebulisers, oxygen. Insertion of pessaries if agreed appropriate by the health care team. Insertion of suppositories or microenemas if agreed appropriate by the health care team. Mouthwashes TASKS WHICH MUST NOT BE UNDERTAKEN BY HOME CARER (Level 4) Filling compliance aids Any invasive procedures, for example Injections Removal of stitches Insertion of catheters Changing of dressings, unless simple dry dressings Stoma care in post-operative phase Testing for diabetes Eye drops/ointments/creams/lotions when medical or nursing assessment indicates trained health staff should be involved Administration of medicines which need skilled observations either before or after administration (e.g. taking pulse) which have been so designated by the health care team. 7 DESCRIPTION OF TASKS WHICH MAY BE UNDERTAKEN BY HOME CARERS LEVELS 2&3 Ordering Prescriptions This will involve ordering prescriptions from the medical practice. At level 3 only those medicines which are listed as regular medicines on the Medication Chart should be ordered. The chart will also indicate the frequency of ordering and the amount to order. Requests for repeat prescriptions are usually made to the medical practice 48 hours in advance of collection, although this interval may be longer if a weekend or public holiday intervenes. Collecting Prescriptions This will involve collecting prescriptions from the medical practice and delivering to the pharmacy. Many pharmacies collect prescriptions directly from the medical practice. Collecting Medicines This will involve collecting medicines from the pharmacy. Many pharmacies have collection/delivery services. The Home Care Senior/Manager should ascertain if one is in operation locally and use this if possible. She/he will also ascertain whether family or friends can undertake this task. Collection of medicines will only be undertaken after an assessment of risk to the Home Carer by the Home Care Senior/Manager. Home carers should be provided with a means of identification (badge or letter of introduction) for use at the surgery/pharmacy when ordering/collecting prescriptions or medicines. Requests for purchasing over the counter (OTC) medicines - Home carers may purchase OTC medicines for Level 2 clients where agreement has been sought from the community pharmacist or GP. Purchase should ideally be made from the pharmacy supplying the clients prescribed medication. The client must be able to manage these medicines themselves. Returning medicines which are no longer required for disposal - this is the responsibility of the client or family. In exceptional circumstances, following risk assessment by the SHCO, the carer may be given permission to return medicines for disposal. LEVEL 3 Storage of Medicines Medicines should be stored in a cool dry place or refrigerator as appropriate (i.e. preferably not in bathrooms or kitchens) and out of direct sunlight. Medicines must be stored so as to ensure that they cannot be taken inappropriately by the service user or any visitors to the house, particularly children. Medicines should be stored in their original containers as dispensed from the pharmacy; they should not be decanted into other containers. When the administration of medicines is the responsibility of the Home Carer they should be stored in a sealed container labelled in a manner to inform relatives/friends not to administer medicines (unless part of the written agreement) without informing the Home Carer. The label of the medicine should be inspected for special storage instructions such as store in the fridge. Medicines stored in the fridge should be placed in a container (e.g. plastic box) and kept separate from food and other consumables The “Medication Chart” should be stored in the client's care plan or alongside the medicines. All medicines in the service user’s home should be stored in one place unless there is special instructions for storage. Creams and ointments should be stored in a separate container from other medicines. Administration of Medicines The following procedure should be followed on every occasion that medicine is administered to a service user 1. Check the name on the container is that of the service user. 2. Check the name and strength of the medication. 3. Check the time of administration 4. Check the dose to be administered. 5. Check for any other specific instructions, such as timing of administration in relation to meals 6. Compare this with the information on the medication chart. If there is any discrepancy or if the Home Carer is unsure about any aspect of giving the medicines, the Senior Home Care Officer/Manager or primary care professional e.g. NHS 24 if out of hours, should be contacted . 7. Check the expiry date of the medicine. 8. . Check the record sheet to ensure the medicine has not already been given. Where appropriate, double check with the service user that they have not already received the medication The Home Carer should then: 1. Explain the procedure to the person to ensure they know what to expect and what to do. 2. Ensure good hygiene by washing hands before and after administering medicines and by keeping everything as clean as possible. 3. Help the person into a comfortable upright position. 4. In order to avoid handling the medicine, the appropriate numbers of tablets or capsules should be tipped into the lid of the container and then placed into a clean medicine cup or the service user’s hand. In the case of foil wrapped medicines, the appropriate dose can be pressed out or torn out of the wrapping into a clean medicine cup or the service user’s hand. The service users will take their own medicine, but the Home Carer should encourage them to wash over tablets/capsules with approximately half a tumblerful of water to ensure that the medicine is washed down into the service user’s stomach. 5. For soluble tablets, the dose should be measured out from its original container as previously described, but it should then be placed in half a tumblerful of water and allowed to dissolve before giving to the service user to drink. If the service user wishes, a cold drink may be taken after. 6. For buccal tablets (i.e. tablets from which the medication is absorbed through the lining of the mouth) the tablet should be placed high up between the upper lip and the gums to either side of the front teeth, where it will soften and adhere to the gum. For service users who wear dentures, the tablet should be placed in any comfortable position between the lip and the gum. 7. For sublingual tablets (i.e. tablets to be placed under the tongue) the tablet should be placed under the tongue and left to dissolve. 8. In the case of liquid medicines, first shake the bottle then measure the appropriate dose into a clean 5ml spoon, medicine measure or oral syringe. When pouring the medicine, tip the bottle with the instruction label facing upwards so that if any of the medicine dribbles down the bottle it will not mark the instruction label. Give the measured dose to the service user to take. Unless it is inappropriate for the particular medicine (e.g. indigestion remedy, cough linctus), a cold drink may be taken after if the service user wishes Wipe the neck of the bottle and any liquid which may have dribbled down the side of the bottle with a clean tissue prior to replacing the lid. 9. Giving Medicine from a Compliance Aid Home Care staff will not give tablets from a compliance aid, only from a labelled bottle. Compliance aids can only be used by level 2 service users who take responsibility for their own medication. Administration of medicines must be recorded on the medication administration form. ‘As Required Drugs’ Some service users may only need to take medicine on an ‘as required’ basis. In this situation, assistance with medication (Level 2) rather than management of medication (i.e. Level 3) is what the Home Carer can offer since the service user will need to be able to let the Home Carer know of their need for the ‘as required’ medicine. This will generally mean that people who cannot make an informed choice about this will be unable to be supported to take ‘as required medicines’. It is acknowledged, however, that some level 3 service users, while incapable of managing their own medication, may still be able to make informed choices about the need for some medication such as analgesics. In these cases as required, drugs may be given by the home carer if the GP Practice team indicate that it is appropriate for this particular patient. The Home Care Senior/Manager will be responsible for assessing this with Health Care Staff. Instructions regarding the reason for administration (indication) and maximum dosage must be clearly stated on the label. Refusal to Take Medication The Home Carer must not force a person to take their medication against their will. The Home Carer should note on the medication administration form that medicines were refused. The Home Carer should inform the Home Care Senior/Manager as soon as possible who in turn will inform the appropriate Health Care Staff member. Under no circumstances should home carers become involved in concealing medication e.g. in food or drinks, in order to get a service user to take medication. Health Check GP Practice team will make the Home Care Senior/Manager aware of any specific side effects of particular medication to be reported back to them. The Home Care Senior/Manager will, in turn, ensure this information is brought to the attention of the Home Carers involved. The Home Carer will be responsible for reporting any concerns back to the Home Care Senior/Manager (or GP Practice team in an emergency) who, in turn, will report to the relevant GP Practice team. The Home Carer should also report back any other health related concerns. Alcohol If the service user appears to have taken excessive amounts of alcohol at the time medicines are due to be administered, the carers should arrange to speak to the GP practice or NHS 24 as soon as possible and this recorded on the Medication Administration Form. Some medicines should not be given even if a small amount of alcohol has been ingested. This will be clearly stated on the label of the medicine. If excessive alcohol consumption is known to be a problem this will be recorded in the care plan drawn up with the help of the service users GP. 8 Disposal of Medicines If the Home carer notices there are medicines in the house which are no longer used, or have reached expiry date he/she should contact the Home Care Senior/Manager who will ask the appropriate GP Practice team member to identify current and discontinued medicines. The Home Care Senior/Manager will then get the service user or their representative’s agreement to take the medicines to the nominated pharmacy for safe disposal using the Medicines Disposal Form. (see appendix 5). This form, signed by the pharmacist should then be kept with the service users documentation If the Pharmacy provides a delivery service it may be more convenient to wait to hand over drugs when new drugs are delivered. Return of drugs to the pharmacy by the Home Carer will only be considered by the Supervisor after an assessment of risk to the Home Carer has been undertaken. SERVICE USERS WHO ARE UNABLE TO GIVE INFORMED CONSENT Anyone who lacks the capacity to give informed consent to medical treatment, whether or not they are compliant with the treatment, should have a Certificate of Incapacity signed by their GP which gives authority for the treatment. This applies even if the person is already subject to Guardianship. Medication must not be administered to service users without this authority. 9 GENERAL INFORMATION – HOW THE PHARMACIST CAN HELP The local community pharmacist can provide a range of services which may help carers. Many pharmacies have leaflets detailing the services they provide. The services offered may differ but are likely to include: Delivery service/collection of unwanted medicines Provision of plain tops on medicine bottles on request Advice on compliance aids to assist with taking medicines. All prescriptions should be taken to the same pharmacy as this will allow the service user records to be kept up to date. The pharmacist is not at liberty to discuss a service user’s medicines in detail with a carer but will be able to provide advice on administration and other medication related issues. 10. TRAINING All Home Carers will receive training in the management of medicines and they must adhere to the guidelines taught in the training programme. Home carers will receive general training on the management of medication, which will cover: Basic information on the collection and storage of medicines Basic information about the types of medical conditions which would require home carers to administer or aid the administration of medication to service users Practical demonstrations on how to administer medication, using different forms and types of medication and dosage aids Disposal of unwanted medicines Commonly occurring side effects of medicines Discussion of problems with administration should a service user refuse, or staff forget to administer Recording procedures. Home Carers will be assessed on their knowledge of the content of these guidelines. Competence to administer medicines will be determined by observation. APPENDIX 1 CHECKLIST FOR ASSESSING CLIENT MEDICATION MANAGEMENT NEED Name____________________________________ Date of Birth/CHI no__________________________ Address__________________________________________________________________________ Tick Medication Dose Tick Medication Dose Person Responsible for Administering Medication: QUESTION Circle Answer If answer to question is 'NO', what action is to be taken (please tick) 1. Does computer record match the medicines being taken? YES / NO Refer to GP 2. Are medicines being taken as prescribed? YES / NO Information to client/carer Medicine Information Sheet Referral Refer to GP 3. Is the client free from medication related problems such as constipation, nausea, difficulty swallowing, drowsiness etc? YES / NO Information to client/carer Medicine Information Sheet Referral Refer to GP 4. Does the client understand the reason for taking medication? (optional question) YES / NO Information to client/carer Medicine Information Sheet Referral Refer to GP 5. Is the client able to read labels? YES / NO 6. Can the client open all their containers? YES / NO 7. Does the patient have:Monitored dosage system (e.g. Dosett) Inhaler Other device (……………...…..) Carer assists or alternative arrangements in place Referral letter to community pharmacist Carer assists or alternative arrangements in place Referral letter to community pharmacist Information to client/carer Refer to GP Negotiate further support from GP, carer, pharmacist or clinic And do they a. use them correctly? b. Have access to a suitable system for filling YES / NO YES / NO 8. Are the client's medicines suitably stored? YES / NO Advice given to client/carer 9. Has the client/carer returned all discontinued medicines to their pharmacy/GP? YES / NO Advice given to client/carer 10. Has the client acceptable quantities of their present medicines? YES / NO Too much - refer to GP Too little - advice to client/carer 11. Which over the counter (OTC) medicines are being taken on a regular basis? Aspirin Laxatives Other (please specify) 12. Has the completed assessment identified that the client has the necessary ability and skills to selfmedicate without supervision? YES / NO Vitamins NOTES/PROBLEMS Creams Paracetamol If 'NO', what further action needs to be taken? Signature of Assessor……………………………………………….Date……………………………………………. Checklist for Assessing Client Medication Management Need. Day/Week_____________________________ Date: Can the client read and interpret the labels? Can the client measure the correct dosage? Can the client manage to take all the medicines without any assistance? Does the client return the medicines to the storage area? Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Time Yes/No Day/Week_____________________________ Date: Can the client read and interpret the labels? Can the client measure the correct dosage? Can the client manage to take all the medicines without any assistance? Does the client return the medicines to the storage area? Time Yes/No Day/Week_____________________________ Date: Can the client read and interpret the labels? Can the client measure the correct dosage? Can the client manage to take all the medicines without any assistance? Does the client return the medicines to the storage area? Time Yes/No APPENDIX 2 EMERGENCY PROCEDURES PERSONAL HOME CARERS MAY NOT ADMINISTER MEDICATION UNLESS IT IS DOCUMENTED ON THE MEDICATION CHART OR ON AN EMERGENCY PROCEDURES FORM CHANGES TO MEDICATION When additional medication is prescribed it is the responsibility of the primary health care team to ensure : a. That a check has been made with the SHCO that the home carer is competent to carry out the task b. Ensure that the Medication Chart is updated before the next dose of the medication is due to be administered. If new medication has been prescribed and not added to the Medication Chart the Personal Home Carer must contact the Home Care Senior/Manager or (if unavailable) the G.P. Practice for advice. When medication is discontinued it is the responsibility of the of the primary health care team including pharmacist to ensure that the entry is scored out on the Medication Chart. If the Personal Home Carer is advised by the client or a non-professional carer that medication has been discontinued and the Medication Chart has not been amended they should withhold the next dose and contact the Home Care Senior/Manager or (if unavailable) the G.P. Practice to obtain confirmation of the discontinuation. It is the responsibility of the Senior Home Care Officer/Manager to ensure that the Personal Home Carer is competent to carry out the new task. HOSPITAL DISCHARGE If a hospital medication chart has been provided the Personal Home Carer may administer medication according to this chart. A Home Care Medication Chart must be provided by the home care manager within 72 hours. If a medication chart has not been provided by the hospital the Personal Home Carer must contact the Home Care Senior/Manager. VERBAL COMMUNICATION When information about medication changes is made verbally (e.g. by telephone) the recipient of the information must read back the information given including spelling out the name of the medication to be administered. The information provided must include the strength of the medication, the number of dose units to be administered and the time of administration. The relevant section of the Emergency Procedures Form must be completed with the date and time and the name and designation of the person giving the information. A separate emergency procedures form must be completed on each occasion. APPENDIX 2 cont. EMERGENCY PROCEDURES FORM Service User Name Address Form completed by Verbal information (if applicable) Received from Designation Date/Time Designation Date MEDICATION TO BE ADMINISTERED Code Medication name, form and strength Number of dose units to be given Breakfast Administration times Midday Teatime Bedtime meal Reason for giving/Special Instructions Other times ADDITIONAL INFORMATION This form to be kept with and on top of the Medication Chart and removed and retained by the Home Care Senior/Manager when a revised medication chart is provided APPENDIX 3 CLIENT NAME MEDICATION CHART - CURRENT MEDICATION DATE OF BIRTH PREPARED BY DATE ADVERSE MEDICINE REACTIONS (IF KNOWN) NAME OF MEDICINE (include form and strength) A B C D E F G H J K L M ORDERING RECORD Amount to Order TIME OF DOSAGE Breakfast Date Ordered Frequency A B C D E F G H J K L M Amount of Dosage Lunch Drugs Obtained Teatime Bedtime Date Ordered Other Information Drugs Obtained Reason For Taking Date Ordered Drugs Obtained Date Started Drugs Ordered Date Stopped Initial when stop Drugs Obtained MEDICATION RECORD This is a list of your current medication. Please show this to any healthcare professional looking after you. Take this with you, along with all your medication if you attend hospital. If your medication changes ask your pharmacist to update this record. NAME OF PATIENT: ADDRESS: TELEPHONE NUMBER: NAME OF PHARMACY: ADDRESS: TELEPHONE NUMBER: NAME OF DOCTOR: ADDRESS: TELEPHONE NUMBER: NAME OF CONTACT PERSON: ADDRESS: TELEPHONE NUMBER: MEDICATION ADMINISTRATION RECORD Month/Year Date 1 2 3 4 5 CLIENT NAME CONTACT HEALTH PROFESSIONAL 6 7 8 9 10 DoB APPENDIX 4 11 12 13 14 15 Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Meds Breakfast Time Refusal SIGN Midday Mealtime Refusal SIGN Evening Mealtime Refusal SIGN Bedtime Refusal SIGN Other Times Refusal SIGN Date Breakfast Time Refusal SIGN Midday Mealtime Refusal SIGN Evening Mealtime Refusal SIGN Bedtime Refusal SIGN Other Times Refusal SIGN Instructions for completion of medication administration chart: Identify the medication you are administering from the medication chart. When you have administered write the code for that medication, a,b,c,d, etc. in the correct box for the date and time of day. If the service user refuses the medication write code for that medication in the correct refusal box for the date and time. Initial legibly to show you have administered the medication and completed the chart. MEDICATION ADMINISTRATION: DATE PROBLEM ACTION TAKEN OUTCOME HOME CARER APPENDIX 4 MEDICATION PERMISSION FORM (for level 3 service user) I give my permission for the Home Care Service to undertake the management of my medication in accordance with my care plan. NAME ________________________________________________ ADDRESS _________________________________________________________________ _________________________________________________________________ SIGNED _______________________________________________ DATE ________________________________________________ For people who are unable to give informed consent (may need Incapacity Act Form Completed) SIGNED CARER/ADVOCATE _________________________________________________ RELATIONSHIP TO SERVICE USER ___________________________________________ DATE _____________________________________ APPENDIX 5 MEDICINES DISPOSAL FORM I give my permission for the following medicines to be removed from my home by ________________________________________ my Home Carer, for safe disposal by the local pharmacist. Name of Drug Quantity (approximate) _________________________________ __________________________________ _________________________________ __________________________________ _________________________________ __________________________________ Name of Service Client____________________________________________________________ Address ____________________________________________________________ ____________________________________________________________ Signature of Service User/Representative ______________________________________________ Date ______________________________ For Pharmacy Use Only I __________________________________ (Pharmacist) confirm the above mentioned drugs have been handed in for destruction. Signed _______________________________________________ Address _______________________________________________ Date _______________________________________________ Pharmacy Stamp Information Leaflet for Home Care Clients If you are receiving care at home provided by the Highland Council you may need some help with ensuring that you are able to take your medication safely and effectively. This leaflet tells you what home care staff can do to help you. Taking the medication prescribed by your general practitioner safely and effectively is one of the best ways of ensuring that you enjoy the best possible health and remain in your own home as long as possible. Care at Home Service Help with Medication There are different levels of help that people may need, maybe just the collection of prescriptions or the return of any unused or unwanted medication to the pharmacy. Others may need a carer to identify which medication they should be taking and to administer it to them at the correct time. Home Care staff will work with your local GP practice and you to identify the level of support you need. This will then be recorded when we are planning your care. What can carers help with? Do you need help with: Ordering medication? Collecting prescriptions? Taking medication? Applying medication? Disposing of unwanted medication Ordering and collecting prescription medication. Returning unused or unwanted medication to the pharmacy. Administering prescribed medication in tablet or liquid form. Applying prescribed creams and drops with instruction from community nurses. Inserting prescribed suppositories and micro enemas with instruction from community nurses. What can carers not help with? Injections Diabetic testing Insertion or removal of catheters Administration of complementary or over - the - counter medication unless agreed by the G.P. Constantly changing medicine requirements Administering medication from compliance devices, e.g. blister packs or dosette boxes. Filling compliance devices How can I be sure that the help I get is safe? The role of the Pharmacist Carers who assist with medication management are trained using a programme developed with NHS pharmacy staff. You will need to get your medicines, whether prescription or bought, from the same community pharmacy each time. Your pharmacist is an expert in the management of medication. If you are experiencing any difficulty taking any of your medicines e.g. side effects, difficulty swallowing or anything is worrying you about the medication itself the pharmacist can help you. You can contact the pharmacist yourself or ask your carer to help you to do this. Sometimes the pharmacist can visit you at home to give advice. Carers will complete records which show what they have done when assisting with medication management. They will also record any problems encountered. Carers cannot be responsible for the safekeeping of your medication when they are not in your home but they will work with you to identify the best place to store both the medication and the records. The Role of Relatives Helpful Contact Details: If carers are administering your medication but you also have relatives or friends who also do this at times then they need to let the local care at home manager that they are doing this. The care at home manager will discuss with them how to complete the administration of medication record that the carers use. This will ensure that you receive your medication as effectively and safely as possible. The role of your Doctor or Community Nurse Your Doctor will discuss your medicines with you. S/he may ask to see all the medicines you take including: Medicine prescribed by your Doctor that you currently take Medicine prescribed by your Doctor which you think are no longer needed All other medications you have bought or take Your Doctor and the healthcare professionals at the surgery will work with you, your pharmacist and Care at Home staff to decide what sort of help you need to take your medication to give you the most benefit. GP……………………………………………………………………………. Contact no:…………………………………………………………………… Community Pharmacist……………………………………………………… Contact no…………………………………………………………………… Other NHS 24 Tel: 08454 242424 Further information on this service may be obtained from the Head of Home Care at Highland Council Headquarters, Glenurquhart Road, Inverness Information Leaflet for Health and Social Care Workers Home Carer Administration of Medicines Background There has been a growing awareness that some people in the community have difficulty with administering their own medication. The majority of home care service users are able to take responsibility for their own medicine management and it is important that people are supported to maintain as many self-care skills as possible. However service users may sometimes require assistance with medication. A policy which will enable home carers to administer medication as safely as possible has been agreed between the Highland Council Social Work Services and NHS Highland and we are now rolling out implementation. Local stakeholders include: GPs, Community Pharmacists, Community Nurses, Home Carers, Unscheduled Care Sevices and Home Care managers. Community Hospital staff, Discharge liaison staff along with others identified as having a key role. Identifying Potential Beneficiaries Which Medicines are Involved People who have difficulties managing their medicines may be identified by any of the stakeholders above, a relative or informal carer or may identify a need themselves. Where individuals have difficulties beyond those which can be resolved following a compliance assessment ( see information leaflet on compliance assessment and monitored dosage systems), a medication needs assessment will be carried out by a primary health care professional (usually the GP) the home care manager and discussed with the individual. This service can only be provided for individuals who are on a stable medication regime. Home carers may administer all oral medications. They may also be involved in assisting administering, eye, ear and nose drops, applying creams, ointments and lotions, assisting with with percutaneous endogastroscopy feeding, inhalation devices and mouthwashes. There are 3 levels of medicines management capability identified within the policy Level 1 – Able to manage their own medicines themselves Level 2 – Able to manage their own medicines with minimal assistance ie understand what their medicines are for, ask for medicines to be reordered or disposed of but require someone to carry out the task, will remember and know which medicines to take if prompted, may require someone to open medicines container tops, can use a monitored dosage system if appropriate Level 3 – Unable to manage medicines as a result of e.g. memory or physical impairment , sight impairment, mental incapacity The individuals to whom this service applies are those assessed at level 3. Medicines which are to be administered on an ‘as required’ basis will require careful assessment and have clear directions for when to administer, maximum doses etc. Community nurses will continue to administer medicines which require invasive procedures or specific clinical monitoring. Informing Key Stakeholders The Home Care Services Manager will maintain a record of all clients requiring this service within their geographical area of responsibility and informing key stakeholders of patient agreed as requiring the service. They will also advise stakeholders of patients no longer requiring the service either on a temporary or permanent basis. The policy identifies the responsibilities of each of the key stakeholders involved in the process. Documentation Medication Charts The community pharmacist will provide medication charts which enable the home carer to administer the medicines. It is vital that these medicines charts are kept up to date. Any changes made to medication regimens require a new chart to be prepared. Patients requiring this service will not receive medicines dispensed in monitored dosage systems. Unscheduled Care The GP practice will ensure that these individuals are appropriately identified to the unscheduled care service using the faxed patient contact form. Emergency Procedures Forms Should medication be changed as a result of a home visit, it is important that the emergency procedures forms are completed at the time of the visit. Home carers cannot administer medicines which are not identified on the medication chart, the emergency procedures form or where the directions on the bottle label do not match those on the medication chart. practice to enable new medication charts to be prepared around the time of discharge for continuity of care. Relatives and Informal Carers If relatives and informal carers are involved at any time in the administration of medicines for a patient receiving a level 3 service from home carers, they must agree to complete the home care medicine administration records. Summary The management of chronic diseases relies heavily on the appropriate use of medicines by those for whom they are prescribed. Inappropriate management of medicines has been identified as being involved in approximately 10% of hospital admissions. Solutions to this problem have been difficult to implement. This new service should assist in addressing this problem and enable individuals to be cared for within their own homes for as long as possible. Further information may be obtained from the, Head of Home Care at Highland Council Headquarters, Glenurquhart Road, Inverness Hospital Admissions/Discharge It should be identified on the single shared assessment form that patients receiving level 3 medicine administration assistance from home carers. The patient should be identified on the hospital patient registration system to enable communication to take place with the GP Prepared by A MacRobbie February 2007 Information Leaflet for Health and Social Care Workers An MDS will only be provided if compliance cannot be addressed by other methods. The pharmacist will review the patient at one week and one month and check that the patient is able to use the MDS. Medication Compliance and Monitored Dosage Systems (MDS) The ability to take medication as prescribed is one of the key tasks that must be supported if a person is to remain well and independent in their own home. Patients who live on their own and have difficulties taking their prescribed medication may be referred to a community pharmacist for review of compliance issues. Referral can be made by nurses, hospital clinicians on discharge, social workers, carers (either formal or informal), the patient, their GP or the community pharmacist. It is important for referrers to include appropriate information about the facts of the difficulties being experienced by the patient and avoid anticipation of particular outcomes prior to formal assessment. The pharmacist will assess compliance issues and decide what steps can be taken to help patients take medication as prescribed. A report will be sent to the referrer. NB. Research has identified that MDS are suitable for less than 20% of patients referred for assessment. MDS are NOT helpful/necessary where patients are: Confused Poorly motivated Have frequent changes to their medication regimen Take medicine ‘as required’ Formal Carers are administering medicines. (an MDS is not essential to the process of “prompting” the client to take their medication.) Unable to use the device The following groups of patients may benefit from a MDS Blind or partially sighted patients Patients on more than 4 medicines Patients who have difficulty handling original containers e.g. bottles or foil packs Some compliance problems Some learning disabilities When a pharmacist fills an MDS it is dispensed and labelled according to professional standards. The pharmacist will advise on the stability of medication in the device as certain medications should not be placed in monitored dosage systems. There is limited capacity for safe provision of MDS for patients and a pharmacist assessment must take place to ensure the most effective provision of the service. Patients who do not benefit from an MDS but receive their medicines dispensed this way deprive those patients who would benefit from this service from receiving it. The pharmacist may be unable to accept additional patients for MDS supply and there may be a waiting list. Regular review of patients receiving MDS should be carried out to ensure this is still an appropriate presentation for their dispensed medicines. The following information summarises some problems and offers some solutions for those most frequently encountered, it is not intended to be an exhaustive list. Some of the solutions may not be available to you. COMMON PROBLEMS and SOLUTIONS 1. Patient is running out of medication due to poor ordering system, lack of synchronisation in repeat cycle or inability to leave house Carer requests and/or delivers prescriptions all medication should be on a 28-day cycle and only 28 days supplied at a time. 2. Patient has poor understanding of the need for a medicine Offer verbal and/or written advice. A medication chart may be useful 3.Frequency or timing of dose, the patient may be unaware of the dose or it may not fit in with their life style. Ensure full directions are on prescription/ label Review medication for rationalisation and simplification of regimen The mid-day dose is the most difficult to remember. Changing to a single or twice daily dose frequency can significantly reduce the complexity of the regime. There is little difference in compliance between once a day and twice a day dosing. 4. Forgetfulness Set up a routine linked to daily activity eg mealtimes Use of 28-day calendar packs Use of reminder charts to help the patient to remember to take their medication. Compliance aids if the person is committed to taking their medication Weekly dispensing into ordinary containers. Involve the informal carer if possible. How able are they to help? You may need to discuss the issue of arranging formal carer input. ( see policy for home carer administration of medicines ) 5. Intentional non-compliance Discuss non-compliance with patient, it may be a result of side-effects, interactions or as a because of their beliefs about their illness or medication. Clarify the issues where possible and refer to prescriber if necessary. 6. Cannot read the label/information leaflet due to poor eye sight Make the best use of clear, easily understandable information. Large print instructions Braille labels 7. English is not the patients’ first language and they cannot understand oral or written instructions Different language patient information leaflets (PILS) are available from Drug Manufacturers and some Health Promotion Departments Enlist the help of a family member or friend who can help with translation 8. Dexterity problems Patients with arthritic or rheumatoid conditions can be offered oversized bottles that they can grasp, with plain tops that they can open Patients can be shown homemade options such as putting rubber bands around the caps, to aid grip. The use of plain caps The use of different sized bottles can help the blind or partially sighted to differentiate between medicines. Arrange for transfer of medication from blister packs to bottles. Compliance aids/monitored dosage systems may help some patients 9. Cannot measure liquids Patients with handling difficulties may prefer two small light liquid bottles. They may not be able to hold or accurately measure from a heavy 500ml bottle. 10. Dexterity problems affecting ability to use inhaler/eye drops Advise GP/nurse for an alternative Aids to help administration of eye drops or aerosol inhalers are available for sale. Refer to local formularies and guidelines 11. Cannot swallow medication Check if available in liquid/soluble form and refer to prescriber Tablet crushers and splitters are available for sale. Check the medication is suitable for crushing or splitting before recommending If you require further information, contact your local community pharmacist or Alison MacRobbie, Palliative/Community Care Pharmacist tel. 01463 706829 or Alison.macrobbie@hpct.scot.nhs.uk AMacR obbie October 2006