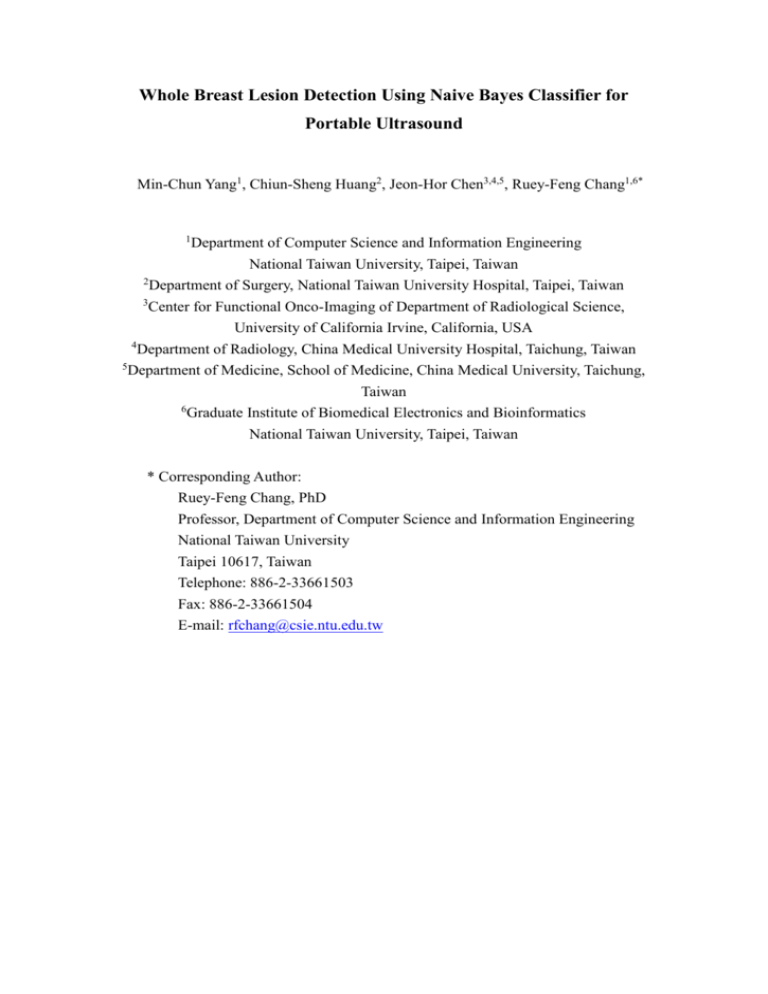
Whole Breast Lesion Detection Using Naive Bayes Classifier for
Portable Ultrasound
Min-Chun Yang1, Chiun-Sheng Huang2, Jeon-Hor Chen3,4,5, Ruey-Feng Chang1,6*
1
Department of Computer Science and Information Engineering
National Taiwan University, Taipei, Taiwan
2
Department of Surgery, National Taiwan University Hospital, Taipei, Taiwan
3
Center for Functional Onco-Imaging of Department of Radiological Science,
University of California Irvine, California, USA
Department of Radiology, China Medical University Hospital, Taichung, Taiwan
5
Department of Medicine, School of Medicine, China Medical University, Taichung,
4
Taiwan
6
Graduate Institute of Biomedical Electronics and Bioinformatics
National Taiwan University, Taipei, Taiwan
* Corresponding Author:
Ruey-Feng Chang, PhD
Professor, Department of Computer Science and Information Engineering
National Taiwan University
Taipei 10617, Taiwan
Telephone: 886-2-33661503
Fax: 886-2-33661504
E-mail: rfchang@csie.ntu.edu.tw
Abstract
In recent years, the portable PC-based ultrasound (US) imaging systems
developed by some companies can provide an integrated computer environment for
the computer-aided diagnosis and detection applications. In this paper, an automatic
whole breast lesion detection system based on the naive Bayes classifier using the
PC-based US system Terason t3000 (Terason Ultrasound, Burlington, MA, USA) with
hand-held probe is proposed. In order to easily retrieve the US images for any regions
of the breast, a clock-based storing system is proposed to record the scanned US
images. A computer-aided detection (CAD) system is also developed to save the
physicians’ time for a huge volume of scanned US images. The pixel classification of
the US is based on the naive Bayes classifier for the proposed lesion detection system.
The pixels of the US are classified into two types: lesions or normal tissues. Then, the
connected component labeling is applied to find the suspected lesions in the image.
Consequently, the labeled 2-D suspected regions are separated into two clusters and
further checked by two-phase lesion selection criteria for the determination of the real
lesion while reducing the false-positive rate. The free-response operative
characteristics (FROC) curve is used to evaluate the detection performance of the
proposed system. According to the experimental results of 31 cases with 33 lesions,
the proposed system yields a 93.4% (31/33) sensitivity at 4.22 false positives (FPs)
per hundred slices. Moreover, the speed for the proposed detection scheme achieves
12.3 frame per second (fps) with an Intel Dual-Core Quad 3 GHz processor and can
be also effectively and efficiently used for other screening systems.
Keywords: Portable ultrasound, naive Bayes classifier, lesion detection
1
Introduction
2
Ultrasound (US) is a good complementary imaging modality to the
3
mammography for diagnosing breast cancer. US could perform better than
4
mammography for a breast with dense fibroglandular tissue (Gordon and Goldenberg
5
1995; Buchberger et al. 2000; Kaplan 2001; Kolb et al. 2002; Crystal et al. 2003).
6
Supplemental screening US could depict small, node-negative breast cancers not seen
7
on mammography (Berg et al. 2008). Recently, the American College of Radiology
8
Imaging Network (ACRIN) has a large trial
9
In the trial report for 2809 women (Berg et al. 2008), adding screening US to
for the screening US (Berg et al. 2008).
10
mammography will
yield an additional 1.1 to 7.2 cancers per 1000 high-risk women
11
but it will also substantially increase the false positive number. The diagnostic
12
accuracy is increased from 78% to 91% for mammography plusUS.
13
In conventional hand-held US, the breast lesions require immediate
14
characterization during the examination. But the demerit of such US screening is the
15
lack of the standardization of sonographic documentation for instant evaluation and
16
the second evaluation on hard copies is needed (Kotsianos-Hermle et al. 2008).
17
Moreover, it also takes time for hand-held US to operate the whole breast examination.
18
In the study of Berg et al. (Berg et al. 2008), a breast screening US takes about 19
19
minutes of physicians’ time. Hence, some automated US breast imaging systems
20
(Shipley et al. 2005; Kotsianos-Hermle et al. 2008) have been proposed to scan the
21
whole breast. Some commercial automated US machines (Ikedo et al. 2007; Chang et
22
al. 2010) are also available. In this study, a freehand whole breast US screening
23
system is proposed without any extra mechanisms to obtain and store the US images
24
for the whole breast.
25
In this study, the portable personal computer (PC) based US imaging system
1
1
(Kim et al. 1997) is used to implement the proposed freehand US screening system. In
2
the system, a Terason t3000 (Terason Ultrasound, Burlington, MA, USA) probe is
3
connected to a PC via a standard FireWire cable to obtain the US images. A
4
clock-based storing method is also proposed to record all the scanning images for
5
later analysis. After the US screening, the physician could diagnose any regions of the
6
breast and retrieve the images easily. If a lesion is found, then its location could be
7
approximately identified by its o’clock direction and the distance from the nipple.
8
Nonetheless, there are several thousand of scanned US images for a patient and
9
the physician still needs a lot of time to diagnose. Hence, the computer-aid detection
10
system (Ikedo et al. 2007; Chang et al. 2010) would be needed for assisting the
11
physician to instantly locate the suspected lesions. Because the scanned US is based
12
on the PC-based imaging system, the computer-aid detection function could be easily
13
installed with the proposed system. This study aims to develop a PC-based
14
computer-aid detection system and offers real-time or off-line lesion detection for
15
physicians. Furthermore, the proposed system with clock-based scanning mechanism
16
might provide multiple observations of the target lesion in different clock regions,
17
thus the lesion can be detected more than one time and diagnosis accuracy can be
18
improved as well.
19
20
Materials and Methods
21
Patients and Lesion Characteristics
22
From January to April 2008, this study collected 33 biopsy-proven lesions (22
23
benign and 11 malignant lesions; size range, 0.52-3.8 cm; mean size 1.48±0.99 cm)
24
from 31 women (age range, 21-79 years; mean age 46.30±11.80 years). All the 31
25
patients are scanned for their whole breast area and the acquired images of each case
2
1
are a series of two-dimensional (2-D) US images with a size of 440×340 pixels.
2
Moreover, the cases have been diagnosed by an experienced radiologist and the
3
locations of possible lesions are identified. The benign lesions include 14 fibrocystic
4
changes, 4 papillomas, and 4 fibroadenomas. The malignant lesions include 8 invasive
5
ductal carcinomas, 1 lobular carcinoma-in-situ (LCIS), 1 mucinous carcinoma, 1
6
infiltrating ductal carcinoma (IDC). Institutional review board approval is obtained
7
for this study and informed consent is obtained from each patient prior to performing
8
a biopsy.
9
Image Data Acquisition
10
In this study, a Terason t3000 (Terason Ultrasound, Burlington, MA, USA) with
11
12L5 small part probe is used to obtain the US images. The frequency of the
12
transducer is between 5MHz and 12MHz and the maximum scanning width and
13
depth are 38mm and 80mm respectively. In the proposed PC-based US screening
14
system,
15
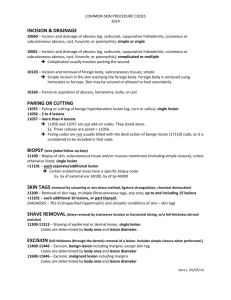
images as shown in Fig. 1. The storage system divides each breast into 12 clock
16
regions; furthermore, the operator selects a clock region to be scanned and then moves
17
the probe from the nipple to outside. In order to reduce the operator-dependent effect
18
of the hand-held probe, the operator is requested to start the scanning process when
19
the probe could move steadily on the skin surface. After the scanning process of the
20
clock region is finished, the operator would check the quality of the scanned image
21
video and decide whether the re-scan process is needed. Moreover, all the scanned
22
images for this region are saved into a file and the whole breast examination for a
23
patient is completed
24
Whole Breast Lesion Detection Based on Naive Bayes Classifier
25
a clock-based storing mechanism is adopted to organize all the scanned
after both breasts are scanned.
We proposed an automatic approach based on the naive Bayes Classifier
3
1
(Domingos and Pazzani 1997; Cevenini et al. 2011) for the whole breast lesion
2
detection. A novel pre-processing technique (i.e. spatio-temporal resolution
3
down-sampling) is proposed to decrease the processing data and improve the
4
detection robustness. After applying the pre-processing technique, each pixel of the
5
image diagnosed by the naive Bayes Classifier is classified into lesions or normal
6
tissues. Then, the connected component labeling (Rosenfeld and Pfaltz 1966) and
7
hole-filling (Mesev 2001) are applied to find the suspected lesions in the image.
8
Consequently, each labeled suspected region would be further separated into two
9
clusters and checked by two-phase lesion selection criteria to reduce the false positive
10
rate while improving the detection sensitivity.
11
Spatio-temporal Resolution Down-sampling
12
Due to the scanned US image slices for each patient are over three thousands and
13
it is hard to recognize the lesion objects in the US image with the noise effect (Giger
14
et al. 1999; Horsch et al. 2004), the spatio-temporal resolution down-sampling
15
(ST-ReD) is proposed to address these issues. The ST-ReD refers to firstly perform
16
the image spatial resolution reduction followed by synthesizing the compact image
17
from a series of degraded 2-D US images. Firstly, each high-resolution US image is
18
resized by the bicubic down-sampling (Keys 1981) to reduce the spatial resolution.
19
Second, the edge-preserved minimum intensity projection scheme is proposed to
20
preserve the edges of the suspected lesion objects when synthesizes the compact
21
images. The procedure of this step would be depicted as follows. For each spatial
22
resolution degraded 2-D image, the Sobel edge detector (Cherri and Karim 1989) is
23
applied to detect the edges in the image. Therefore, the edge map of each degraded
24
image can be obtained and each pixel of the edge map can be defined as edge or
25
non-edge pixel. Finally, the intensity value of a specific pixel of the compact image
4
1
can be decided by using the following projection scheme. The maximum intensity
2
projection (MIP) (Lagerwaard et al. 2005) of the consecutive degraded images is
3
applied if one or more than one pixel is defined as the edge pixel in the edge maps;
4
otherwise, the minimum intensity projection (mIP) (Beigelman-Aubry et al. 2005) is
5
applied if no edge pixels are defined in this position. More specifically, this step can
6
be formulated as
n
arg
max
U
(
x
,
y
)
,
if
Edgei(x,y) 1
i
G ( x, y ) i 1,..., n
i 1
arg min U i ( x, y ) , otherwise
i 1,..., n
7
(1)
8
where the G(x,y) is the projected intensity value of the compact image in pixel (x,y),
9
Ui(x,y) is the intensity value of the slice number i in pixel (x,y) out of n series of
10
degraded images and Edgei(x,y) equals to 1 if the pixel is an edge pixel or 0 represents
11
the non-edge pixel in the edge map.
12
Based on the approach, the detection time of the screening system can be
13
significantly reduced and the suspected lesion objects can be easily identified.
14
Moreover, the compact images with different projection schemes are shown in Fig. 2.
15
Obviously, the lesion and fat region might be misclassified as the same group by most
16
of the clustering algorithms while applying the mIP scheme (Beigelman-Aubry et al.
17
2005).
18
Tissue Feature Extraction
19
In the study, the pixels of the compact US image are defined as lesions or normal
20
tissues. Moreover, two feasible feature parameters are adopted for characterizing the
21
pixels. These feature parameters are, intensity local mean u and intensity local stick s,
22
which are calculated with a 5×5 region mask. Generally speaking, the gray level of
23
the lesion tissues tends to be smaller than that of the surrounding normal tissues. On
24
the other hand, the US images with speckle noise (Rakotomamonjy et al. 2000) might
5
1
affect the pixel classification results. Therefore, the mean feature parameter u
2
calculated from the local average of the mask can be used to characterize the lesion
3
tissue and suppress the speckle noise in the US image (Gonzalez et al. 2008).
4
Furthermore, the stick method (Czerwinski et al. 1999) is applied to enhance the
5
contrast of the edges to differentiate the lesion regions easily from other tissue regions.
6
The stick feature is an optimal line detector that is superior to some traditional
7
edge-detection methods (Haralick 1984; Wagner et al. 1988). More explicitly, if a
8
local square mask with N×N in an image is clipped, there are (2N-2) short lines with N
9
pixels and each short line passes through the center pixel of the mask. The sticks with
10
length five are adopted in our study and the stick feature s can be obtained by
11
searching the maximum value among the line templates (Czerwinski et al. 1999). The
12
stick feature parameter can be used to improve the classification accuracy while the
13
edge pixels between the lesion and fat region are smoothed by the mean feature
14
parameter (i.e. the edge pixels might be misclassified as the lesion tissues).
15
Distribution Model Estimation for Feature Parameters and Pixels Reasoning by
16
Naive Bayes Classification
17
The procedures of constructing the distribution models of the feature parameters
18
for both tissues and pixels reasoning based on naive Bayes Classifier (Domingos and
19
Pazzani 1997) would be drawn in this stage. Moreover, the leave-one-patient-out
20
cross validation (LOPO-CV) (Dundar et al. 2004; Andre et al. 2010) is adopted for the
21
patients’ dataset for objective performance evaluation. In each performance validation,
22
US images from one patient are kept for validation and the others would be used as
23
the training set (including the candidate images with or without the lesions) for
24
constructing the feature distribution models. The level set segmentation (Sethian
25
1996) is applied to segment the candidate images to obtain the lesion regions.
6
1
Afterward, we extract the observed samples with lesions or normal tissues from these
2
training images. Consequently, the feature values u and s can be calculated for the
3
observed samples to obtain the statistical histograms respectively. The statistical
4
histogram for feature parameter stick s of both tissues is depicted in Fig. 3 (a).
5
The Rayleigh distribution is a common distribution for describing the average
6
wind speed (Morgan et al. 2011) and can be used to characterize the Rayleigh-like
7
distribution of the feature parameters in this study. The probability density function
8
(PDF) of Rayleigh distribution for feature variable X with tissue class W can be
9
modeled as follows:
X 2
F ( X | w ,W )
10
X
w
exp 2 w , X {u , s}, W {L, N }.
2
2
(2)
11
where the feature variable X corresponds to feature parameter u or s, class W
12
corresponds to the tissue type L (Lesion) or N (Normal), and σw is the model
13
parameter to be estimated.
14
The maximum likelihood Rayleigh estimator is adopted to estimate the model
15
parameter σw that can be approximated by the calculation of the σ̂ w (Sijbers et al.
16
1998;Sijbers et al. 1999):
n
ˆ w
17
X i2
i 1
2n
, X {u, s}, W {L, N }.
(3)
18
where n is the number of the training samples. The estimated Rayleigh distribution
19
models for stick feature parameter with normal and lesion tissue are depicted in Fig. 3
20
(a).
21
After the Rayleigh-distributed models of feature parameters are constructed for
22
both tissues, the naive Bayes Classifier (Domingos and Pazzani 1997; Cevenini et al.
7
1
2011) is applied to reason the tissue class of each pixel of the test US images. The
2
naive Bayes classifier (Domingos and Pazzani 1997) is the probabilistic model which
3
is based on conditional independence assumption among the features (attributes) of
4
Bayes’ theorem. The equal priori probability of the features (Cevenini et al. 2011) is
5
assumed in this study. Thepixel is classified as the lesion tissue if the corresponding
6
likelihood probability (i.e. the product of the Rayleigh PDF of feature parameters) is
7
higher than that of the normal tissue:
P(X| , L) =
F(X | L , L) F(u | L , L)F (s | L , L)
X {u , s}
8
F(u | N , N)F ( s | N , N )
F(X| N , N )
(4)
X {u , s}
P(X| , N)
9
where P(X|σ,L) and P(X|σ,N) denote the likelihood probability of the pixel to be
10
classified as a lesion tissue and a normal tissue respectively. The decision boundary
11
exists in the condition when P(X|σ,L) equals to P(X|σ,N). The classification result
12
based on naive Bayes classifier of a compact US image and corresponding decision
13
regions are shown in Fig. 3 (b)-(d).
14
Suspected Lesions Extraction
15
After classifying each pixel of the US images by the naive Bayes classifier, the
16
gray-scale US image is transferred into a binary image. The 2-D connected
17
components labeling (Rosenfeld and Pfaltz 1966) is applied to label the lesion pixels
18
and group the connected labels to obtain the isolated regions in an image. The
19
hole-filling (Mesev 2001) is adopted for filling the holes and gaps inside the regions.
20
Afterward, each suspected region would be evaluated by two-phase selection criteria
21
to determine whether the labeled region is a lesion or not. The two-phase lesion
22
selection criteria referring to each suspected 2-D lesion region would be firstly filtered
8
1
by the 2-D shape feature criteria. Afterward, the candidate 2-D lesions (those satisfy
2
the 2-D shape feature criteria) would be further checked by the region continuity
3
criteria for the final determination of a real lesion. The two-phase lesion selection
4
criteria are adopted for the reduction of false-positive rate of the redundant suspected
5
2-D lesions detected by the neighboring image slices. The detection sensitivity can be
6
improved if part of the real lesion object can satisfy the region continuity criteria. In
7
the experimental results, we would demonstrate the effectiveness of the 2-D whole
8
breast lesion detection mechanism especially for the malignant cases with shadowing.
9
False Positive Rate Reduction via Two-phase Lesion Selection Criteria
10
In the first lesion selection phase, the 2-D shape feature criteria include area size,
11
width-height ratio, region ratio and the compactness (Bribiesca 2008) are applied for
12
filtering the unwanted 2-D regions. The lesion area size Rsize is used to filter out these
13
regions with smaller or larger size caused by speckle noise or shadows. On the other
14
hand, the width-height ratio RW_H used to eliminate the non-lesion regions with
15
lengthy or flat shapes can be defined as
16
RW_H
Wb ,
b
H
Hb
Wb ,
if H b Wb
(5)
otherwise
17
where Wb and Hb are the width and height of the minimum-bounding box (the
18
minimum rectangle covers the lesion region) respectively.
19
The region ratio RS_R which describes the cover ratio of the suspected region
20
relatives to the minimum-bounding box can be calculated as
21
RS_R
22
23
Rsize
Wb H b
(6)
Compactness is a shape descriptor which measures the degree of the compact
around the margin within an object.
Moreover, the 2-D image compactness Rc
9
1
2
introduced by Bribiesca et al. (Bribiesca 2008) can be defined as
Rc
N pel P / 4
N pel
N pel
(7)
3
where Npel is the number of pixels in the lesion and the perimeter P is the number of
4
pixels of the sides of a 2-D closed shape object.
5
The 2-D shape features criteria used to characterize the suspected lesions are
6
evaluated by the LOPO-CV with classification trees (Praagman 1985). In the
7
classification tree implementation, the information gain (Quinlan 1987) is adopted as
8
the feature (numeric attribute) selection criteria. The pre-pruning and post-pruning
9
(Bramer 2002; Fournier and Cremilleux 2002) are used to prevent the overfitting of
10
the training data while building the tree. After the tree is constructed, the class label of
11
each leaf is assigned as the lesion or non-lesion candidate.
12
In the second lesion selection phase, the region continuity criteria consider the
13
consecutive connected 2-D lesions in the depth (scan) direction and volume size are
14
adopted for deciding the final lesions. The depth ratio Rd which describes the lesion
15
continuity relatives to its maximum length can be calculated as
16
Rd
arg max Lcon les
L
Ns
(8)
lices
17
where Nslices represents the number of slices of the connected 2-D lesions and Lcon-les is
18
the longest length between Wb and Hb among all the connected 2-D lesions. Moreover,
19
the volume size Rvol of the lesion can be calculated by summing the total region size
20
of n connected 2-D lesions slices as follows:
n
21
Rvol Rsize _ i
(9)
i 1
22
where Rsize_i is the area size of the slice number i out of n connected candidate 2-D
10
1
lesions.
2
Consequently, the two region continuity criteria for determining the real lesion of
3
a series of candidate 2-D lesions would be also evaluated by the LOPO-CV with
4
classification trees (Praagman 1985). The experimental results would demonstrate the
5
effectiveness of the proposed two-phase lesion selection criteria.
6
Separate Classification of Whole and Partial Lesions for Improving Detection
7
Sensitivity
8
Due to the limited scan width of the probe (only 38mm), the flat-shaped fat or
9
shadow in the sides of the scanned US images might be cut as the partial regions and
10
misclassified as the lesion candidates. Therefore, in order to improve the detection
11
sensitivity, the suspected lesions are split into two clusters: the suspected lesions
12
connected to one side or both sides of the US image would be categorized as the
13
outside cluster; otherwise, the suspected regions would be categorized as the inside
14
cluster. The suspected regions of each cluster are classified by their respective
15
classification trees and the detection sensitivity can be merged by both clusters. The
16
advantage of splitting the detected regions into two clusters is the lesion-like regions
17
(i.e. the shape similar to the real lesions due to the shadow noise or cut flat-shaped fat)
18
of the outside cluster can be recognized as the non-lesion regions without the
19
classification intervention of the real lesions in the inside cluster. Therefore, better
20
detection sensitivity and lower false-positives rate can be achieved. More details
21
would be drawn in the experimental results.
22
23
Results
24
The proposed system of lesion detection for portable US images is implemented
25
by the C++ language under the Visual Studio .NET 2008 (Microsoft, Seattle, WA)
11
1
with Microsoft Windows XP operating system (Microsoft, Seattle, WA). The program
2
is running on an Intel Dual-Core Quad 3 GHz CPU with 4G RAM.
3
Performance Quantitative Evaluation
4
In this experiment, the proposed detection method is evaluated for 29 patients
5
with one lesion and 2 patients with two lesions. In the two-phase lesion selection
6
stages for false-positive reduction, the classification trees (Praagman 1985) are
7
adopted with LOPO-CV. Moreover, the predicted class probabilities of the regions
8
from the classification trees lie between 0 and 1. If the predicting probability of the
9
suspected region is larger than the chosen threshold, the region would be classified as
10
the lesion candidate; otherwise, the region would be regarded as a non-lesion and
11
ignored.
12
(Chakraborty 1989; Yu and Guan 2000) curves can be generated by changing the
13
threshold level of the predicted probability to demonstrate the detection performance
14
of the automatic screening system.
Furthermore,
the
free-response
operating
characteristics
(FROC)
15
In this study, the physicians would examine the whole scanned videos and
16
manually delineate the lesion boundaries. The detected lesion is regarded as a “true
17
positive” if the center of gravity is located inside the delineated lesion region (Ikedo et
18
al. 2007). Otherwise, a “false positive” is considered. Besides, the patient case would
19
be regarded as a TP case if the lesion is detected in one or more than one clock
20
regions. On the other hand, the scanned image slices for different patients are varied
21
in our database; therefore, the false positives (FPs) are counted and evaluated for all
22
the scanned image slices in per patient case, per clock section and per hundred image
23
slices. In the experiment, we would firstly validate the detection performance of the
24
suspected regions with and without the split method and corresponding false-positive
25
rate is shown in per hundred image slices respectively. In the first-phase lesion
12
1
selection stage, the FROC curves of all suspected lesions filtered by the 2-D shape
2
feature criteria are shown in Fig. 4 (a). The sensitivity rate of lesion detection after the
3
first-phase FPs reduction for the non-split method is 96.97% (32/33) at 58.77 FPs per
4
hundred slices and is 96.97% (32/33) at 39.67 FPs per hundred slices for the split
5
method. Moreover, the threshold levels of the classifier with maximum detection
6
sensitivity are chosen; therefore, the 2-D suspected lesions satisfy the threshold would
7
be kept for evaluation of the second-phase lesion selection stage. The FROC curves of
8
the connected 2-D candidate lesions filtered by the region continuity criteria are
9
shown in Fig. 4 (b). The sensitivity rate of lesion detection after the second-phase FPs
10
reduction for the non-split method is 93.94% (31/33) at 10.15 FPs per hundred slices
11
compared to 93.94% (31/33) at 4.22 FPs per hundred slices for the split method (or
12
87.88% (29/33) with 5.65 FPs per hundred slices for the non-split method compared
13
to 84.85% (28/33) with 2.23 FPs per hundred slices for split method). As shown in
14
Fig. 4, the method using two split clusters achieves a better detection sensitivity and
15
lower false-positive rate than the method using one non-split cluster. Therefore, the
16
experimental result shows the efficacy of the split method.
17
To conclude the detection performance of the proposed split method, the
18
sensitivity rates of different sizes for benign, malignant lesions and whole dataset are
19
listed in Table 1. Moreover, we list three FPs measurements (i.e. count in per patient
20
case, per clock section and per hundred image slices) for two detection sensitivity
21
rates in Table 2 to clarify the detection performance. Though the false-positive rate of
22
malignant lesions is higher than that of benign lesions (the malignant lesions may
23
introduce more lesion-like shadowing and regions), the difference is not significant.
24
Moreover, each scanned clock region is partially overlapped with the neighboring
25
clock regions in the proposed clock-based method. Thus, the lesion might exist in
13
1
several clock regions and can be detected multiple times as shown in Fig. 5. This
2
clock-based scanning mechanism presents high detection sensitivity because of
3
offering multiple observations of the target lesion. On the other hand, we can observe
4
that two malignant lesions with shadowing as shown in Fig. 6 can be detected based
5
on the proposed method. The main reason is that if part of the malignant lesion (i.e.
6
several consecutive compact frames) can satisfy the region continuity criteria, and
7
then the real lesion would be considered as well. In our database, there are 5 out of 11
8
malignant lesions and 2 out of 22 benign lesions with shadowing that can be detected
9
based on the proposed mechanism. Moreover, the lesion size of the two false negative
10
cases is below 0.6 cm. Therefore, the real lesions would be classified as the
11
non-lesion regions by the lesion size criterion or region continuity criteria. As shown
12
in Fig. 7, a false negative case with fewer scanned image slices is classified as the
13
non-lesion regions by the region continuity criteria. Furthermore, the detection
14
performance with estimated detection difficulty of the lesions by the physician is
15
reported in Table 3. The estimated items described in the BI-RADS-US (Liberman et
16
al. 1998) including internal echo pattern, margin, calcification and shadowing
17
(including posterior shadows) are listed in our study. In order to simplify and clarify
18
the assessment of the difficulty of the lesions, the physician would examine the scan
19
video and choose the representative frame (i.e. the most easily recognized frame for
20
the real lesion) for each patient case. A positivity is defined if the lesion is difficult to
21
recognize under the specific estimated item (e.g. the margin of the lesion is unclear to
22
be detected); otherwise, a negativity is defined. As observed in Table 3, the benign
23
cases with internal echo pattern (e.g. the echo pattern inside the lesion is bright and
24
inhomogeneous) or unclear margin might lead the detected lesions to be grouped as
25
smaller regions and be eliminated. Besides, the calcification and shadowing would not
14
1
significantly influence the detection results according to the test database.
2
On the other hand, the spatial down-sampling scale factor is 2 and five
3
connective degraded US images are used to synthesize one compact image in the
4
spatio-temporal resolution down-sampling stage. In order to improve the detection
5
robustness, the neighboring compact images have two connective degraded US
6
images in common. The detection frame rate of the proposed screening system is
7
about 12.3 fps (frame rate of the portable machine is set to 10 fps). Thus, the proposed
8
automatic lesion detection system can offer effective and efficient whole breast
9
examination for the operators.
10
11
Discussion
12
Drukker et al. (Drukker et al. 2002; Drukker et al. 2003; Drukker et al. 2005)
13
advocates to the breast US lesion detection for the still images acquired by the initial
14
localization of the physicians. In order to ensure the detection robustness, normal
15
images without lesions were constructed and the lesion detection performance is
16
evaluated with the collected lesions database. Their studies present 94% detection
17
sensitivity at 0.48 false-positives per image (Drukker et al. 2002) and 80% detection
18
sensitivity at 0.25 false-positives per image for malignant lesions that exhibit posterior
19
acoustic shadowing (Drukker et al. 2003). The main limitation of the approach is the
20
lesion detection algorithm only applied and constrained to lesion candidate images
21
localized by the physicians rather than the streaming video acquired from the whole
22
breast US scanners. Moreover, each image analyzed in 1 min (Drukker et al. 2002) is
23
not practical for the whole breast lesion detection with thousands of scanned images.
24
In recent years, the automatic lesion detection mechanism for whole breast US has
25
been investigated (Ikedo et al. 2007; Chang et al. 2010). Ikedo et al. (Ikedo et al. 2007)
15
1
proposed a 2-D detection scheme system with detection rate 80.6% (29/36) at 4.52
2
FPs per hundred slices (84 image slices per case) with the re-substitution method
3
(Theodoridis and Koutroumbas 2009) (i.e. using the same training and test sets) or
4
80.6% (29/36) at 7.85 FPs per hundred slices with the leave-one-out method. In the
5
edge detection stage for the suspected lesions, the vertical edges of the Cooper’s
6
ligaments in the fat tissue and ribs regions would be falsely detected as the lesion
7
candidates. On the other hand, the proposed 2-D detection scheme without
8
considering the 3-D characteristics of the lesions leads to enormous false positive
9
lesions. Chang et al. (Chang et al. 2010) proposed an automatic detection system
10
considers 3-D characteristics (e.g. coronal-view feature) and region continuity criteria
11
for false positive reduction. The detection rate is 92.3% (24/26) at 2.10 FPs per
12
hundred slices (84 image slices per case). The proposed automatic detection system
13
presents high detection sensitivity and very promising false positive rates.
14
Nonetheless, because there are no standards for selecting the threshold of the feature
15
parameters for the suspected lesions, the manual selection of the thresholds by
16
observing all the patient cases might be subjective to the physicians’ experience.
17
Moreover, the exhaustive search for adjusting the threshold level of the feature
18
parameters might not be convenient for the practical use.
19
In this study, an automatic detection is proposed for the whole breast lesion
20
detection. The two-phase false positive reduction offers an objective scheme by the
21
classification trees with LOPO-CV. Besides, the proposed system achieves a real-time
22
detection application due to the aid of the spatio-temporal resolution down-sampling
23
and fast pixel classification using naive Bayes classifier (Domingos and Pazzani
24
1997). Therefore, the proposed detection mechanism can be possibly used for the
25
real-time guidance for the operators during the whole breast examination (e.g.
16
1
real-time alarm for the operator while the lesions are detected or immediate second
2
breast examination is required). The advantage of the clock-based storing method can
3
assist the physicians to easily locate the detected lesions. This mechanism can
4
improve the detection sensitivity and robustness if the target lesion appears in more
5
than one clock regions.
6
There are several limitations in this study. First, the scan speed with the
7
hand-held probe of the operator might not be fixed and the spacing of the whole
8
breast US is unknown, thus the quality of the compact image with the proposed
9
edge-preserved mIP would be influenced. Therefore, the 3-D characteristics such as
10
coronal-view feature (Chang et al. 2010) could not be used for filtering out most of
11
the ribs and shape-flapped fats. Second, the same false positive lesion might be
12
repetitively counted due to that the shape-flapped fats or ribs might appear in several
13
clock regions. Lastly, the test database is relatively small in our experiments.
14
Therefore, a superior mechanism of larger dataset for obtaining the fixed spacing to
15
reduce the redundant false positives should be investigated in our future study.
16
Pending future verification, the proposed detection algorithm can be used for the
17
automated whole breast ultrasound (ABUS) (Chang et al. 2011) and then the robust
18
shape feature of the detected lesions can be extracted (Moon et al. 2011) for diagnosis
19
purpose. Thus, the system could provide a more reliable and robust detection and
20
diagnosis mechanism for clinical applications.
21
22
Acknowledgments
23
The authors would like to thank the National Science Council
24
99-2221-E-002-136-MY3), Ministry of Economic Affairs (100-EC-17-A-19-S1-164)
25
of the Republic of China, and National Taiwan University (10R80919-6) for the
17
(NSC
1
funding support.
2
18
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
References
Andre B, Vercauteren T, Buchner AM, Shahid MW, Wallace MB, Ayache N. An
image retrieval approach to setup difficulty levels in training systems for
endomicroscopy diagnosis. Med Image Comput Comput Assist Interv
2010;13:480-7.
Beigelman-Aubry C, Hill C, Guibal A, Savatovsky J, Grenier PA. Multi-detector row
CT and postprocessing techniques in the assessment of diffuse lung disease.
Radiographics 2005;25:1639-52.
Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Bohm-Velez M, Pisano
ED, Jong RA, Evans WP, Morton MJ, Mahoney MC, Larsen LH, Barr RG, Farria
DM, Marques HS, Boparai K. Combined screening with ultrasound and
mammography vs mammography alone in women at elevated risk of breast
cancer. JAMA 2008;299:2151-63.
Bramer M. Pre-pruning classification trees to reduce overfitting in noisy domains.
Intelligent Data Engineering and Automated Learning - Ideal 2002
2002;2412:7-12.
Bribiesca E. An easy measure of compactness for 2D and 3D shapes. Pattern
Recognition 2008;41:543-54.
Buchberger W, Niehoff A, Obrist P, DeKoekkoek-Doll P, Dunser M. Clinically and
mammographically occult breast lesions: detection and classification with
high-resolution sonography. Seminars in ultrasound, CT, and MR
2000;21:325-36.
Cevenini G, Barbini E, Massai MR, Barbini P. A naive Bayes classifier for planning
transfusion requirements in heart surgery. J Eval Clin Pract 2011;
Chakraborty DP. Maximum likelihood analysis of free-response receiver operating
characteristic (FROC) data. Med Phys 1989;16:561-8.
Chang JM, Moon WK, Cho N, Park JS, Kim SJ. Radiologists' performance in the
detection of benign and malignant masses with 3D automated breast ultrasound
(ABUS). Eur J Radiol 2011;78:99-103.
Chang RF, Chang-Chien KC, Takada E, Huang CS, Chou YH, Kuo CM, Chen JH.
Rapid image stitching and computer-aided detection for multipass automated
breast ultrasound. Med Phys 2010;37:2063-73.
Cherri AK, Karim MA. Optical symbolic substitution: edge detection using Prewitt,
Sobel, and Roberts operators. Appl Opt 1989;28:4644-8.
Crystal P, Strano SD, Shcharynski S, Koretz MJ. Using sonography to screen women
with mammographically dense breasts. AJR Am J Roentgenol 2003;181:177-82.
Czerwinski RN, Jones DL, O'Brien WD, Jr. Detection of lines and boundaries in
speckle images--application to medical ultrasound. IEEE Trans Med Imaging
1999;18:126-36.
Domingos P, Pazzani M. On the optimality of the simple Bayesian classifier under
zero-one loss. Machine Learning 1997;29:103-30.
Drukker K, Giger ML, Horsch K, Kupinski MA, Vyborny CJ, Mendelson EB.
Computerized lesion detection on breast ultrasound. Med Phys 2002;29:1438-46.
Drukker K, Giger ML, Mendelson EB. Computerized analysis of shadowing on breast
ultrasound for improved lesion detection. Med Phys 2003;30:1833-42.
Drukker K, Giger ML, Metz CE. Robustness of computerized lesion detection and
classification scheme across different breast US platforms. Radiology
2005;237:834-40.
Dundar M, Fung G, Bogoni L, Macari M, Megibow A, Rao B. A methodology for
19
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
training and validating a CAD system and potential pitfalls. International
Congress Series 2004;1268:1010-4.
Fournier D, Cremilleux B. A quality index for decision tree pruning.
Knowledge-Based Systems 2002;15:37-43.
Giger ML, Al-Hallaq H, Huo ZM, Moran C, Wolverton DE, Chan CW, Zhong WM.
Computerized analysis of lesions in US images of the breast. Academic
Radiology 1999;6:665-74.
Gonzalez RC, Woods RE, Masters BR. Digital image processing. Upper Saddle River,
New Jersey: Pearson Prentice Hall, 2008.
Gordon PB, Goldenberg SL. Malignant breast masses detected only by ultrasound. A
retrospective review. Cancer 1995;76:626-30.
Haralick RM. Digital Step Edges from Zero Crossing of 2nd Directional-Derivatives.
Ieee Transactions on Pattern Analysis and Machine Intelligence 1984;6:58-68.
Horsch K, Giger ML, Vyborny CJ, Venta LA. Performance of computer-aided
diagnosis in the interpretation of lesions on breast sonography. Academic
Radiology 2004;11:272-80.
Ikedo Y, Fukuoka D, Hara T, Fujita H, Takada E, Endo T, Morita T. Development of a
fully automatic scheme for detection of masses in whole breast ultrasound
images. Med Phys 2007;34:4378-88.
Kaplan SS. Clinical utility of bilateral whole-breast US in the evaluation of women
with dense breast tissue. Radiology 2001;221:641-9.
Keys RG. Cubic Convolution Interpolation for Digital Image-Processing. Ieee
Transactions on Acoustics Speech and Signal Processing 1981;29:1153-60.
Kim Y, Kim JH, Basoglu C, Winter TC. Programmable ultrasound imaging using
multimedia technologies: a next-generation ultrasound machine. 1997.
Kolb TM, Lichy J, Newhouse JH. Comparison of the performance of screening
mammography, physical examination, and breast US and evaluation of factors
that influence them: An analysis of 27,825 patient evaluations. Radiology
2002;225:165-75.
Kotsianos-Hermle D, Hiltawsky KM, Wirth S, Fischer T, Friese K, Reiser M.
Analysis of 107 breast lesions with automated 3D ultrasound and comparison
with mammography and manual ultrasound. Eur J Radiol 2008;
Lagerwaard FJ, Underberg RWM, Slotman BJ, Cuijpers JP, Senan S. Use of
maximum intensity projections (MIP) for target volume generation in 4DCT
scans for lung cancer. International Journal of Radiation Oncology Biology
Physics 2005;63:253-60.
Liberman L, Abramson AF, Squires FB, Glassman JR, Morris EA, Dershaw DD. The
Breast Imaging Reporting and Data System: Positive predictive value of
mammographic features and final assessment categories. American Journal of
Roentgenology 1998;171:35-40.
Mesev V. Morphological image analysis: principles and applications. Environment
and Planning B-Planning & Design 2001;28:800-1.
Moon WK, Shen YW, Huang CS, Chiang LR, Chang RF. Computer-aided diagnosis
for the classification of breast masses in automated whole breast ultrasound
images. Ultrasound Med Biol 2011;37:539-48.
Morgan EC, Lackner M, Vogel RM, Baise LG. Probability distributions for offshore
wind speeds. Energy Conversion and Management 2011;52:15-26.
Praagman J. Classification and Regression Trees - Breiman,L, Friedman,Jh,
Olshen,Ra, Stone,Cj. European Journal of Operational Research 1985;19:144-.
Quinlan JR. Simplifying Decision Trees. International Journal of Man-Machine
20
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
Studies 1987;27:221-34.
Rakotomamonjy A, Deforge P, Marche P. Wavelet-based speckle noise reduction in
ultrasound B-scan images. Ultrason Imaging 2000;22:73-94.
Rosenfeld A, Pfaltz JL. Sequential Operations in Digital Picture Processing. J ACM
1966;13:471-94.
Sethian JA. A fast marching level set method for monotonically advancing fronts.
Proc Natl Acad Sci U S A 1996;93:1591-5.
Shipley JA, Duck FA, Goddard DA, Hillman MR, Halliwell M, Jones MG, Thomas
BT. Automated quantitative volumetric breast ultrasound data-acquisition system.
Ultrasound in Medicine and Biology 2005;31:905-17.
Theodoridis S, Koutroumbas K. Pattern Recognition. San Diego, CA: Academic Press,
2009.
Wagner RF, Insana MF, Smith SW. Fundamental Correlation Lengths of Coherent
Speckle in Medical Ultrasonic Images. Ieee Transactions on Ultrasonics
Ferroelectrics and Frequency Control 1988;35:34-44.
Yu S, Guan L. A CAD system for the automatic detection of clustered
microcalcifications in digitized mammogram films. IEEE Trans Med Imaging
2000;19:115-26.
21
1
2
3
Figure Captions
Fig. 1
The proposed clock-based storing method.
4
Fig. 2
The compact image obtained from different projection algorithms. (a) The
5
compact image with the highlighted lesion. (b) The compact image with the
6
edge-preserved minimum-intensity projection. (c) The compact image with
7
the minimum intensity projection (mIP).
8
Fig. 3
(a) The calculated statistical histograms and estimated Rayleigh distribution
9
of the stick feature parameter of both tissues. (b) An example compact US
10
image. (c) The classification result based on naive Bayes classification. (d)
11
The decision regions of the proposed feature parameters. The feature
12
parameters of the inference pixels lay in the black decision region would be
13
classified as the lesion tissue.
14
Fig. 4
The FROC curve of the two-phase lesion selection criteria. (a) First-phase:
15
the sensitivity rate for non-split method is 96.97% (32/33) at 58.77 FPs per
16
hundred slices (THnon-split = 0.93) and is 96.97% (32/33) at 39.67 FPs per
17
hundred slices for split method (THsplit_inside = THsplit_outside = 0.94). (b)
18
Second-phase: the sensitivity rate for non-split method is 93.94% (31/33) at
19
10.15 FPs per hundred slices (THnon-split = 0.1) and is 93.94% (31/33) at 4.22
20
FPs per hundred slices (THsplit_inside = 0.11, THsplit_outside = 0.08) for split
21
method.
22
Fig. 5
A series of 2-D compact image slices and corresponding determined lesions.
23
Note that the real lesion is highlighted with solid circle, and the false
24
positive lesion is indicated by the dotted circle. (a) A true-positive case of a
25
1.0 cm invasive ductal carcinoma in the right breast. (i) 10 o’clock region.
26
(ii) 11 o’clock region. (b) A true-positive case of a 0.67 cm fibrocystic
22
1
2
disease in the left breast. (i) 1 o’clock region. (ii) 2 o’clock region.
Fig. 6
Two true-positive malignant cases with shadowing. Note that the detected
3
real lesion is highlighted with solid circle and the shadow is indicated by the
4
dotted circle. (a) A true-positive case of a 2.8 cm invasive ductal carcinoma.
5
(b) A true-positive case of a 2.2 cm invasive ductal carcinoma.
6
Fig. 7
7
8
9
10
A false-negative case of a 0.52 cm fibroadenoma in the right breast and the
real lesion is indicated by the dotted circle. (a) 10 o’clock. (b) 11 o’clock.
Table 1 The sensitivity rates of different sizes of benign, malignant lesions and whole
dataset.
Benign
< 1.0 cm
1.0 - 2.0 cm
2.0 - 3.0 cm
≧3.0 cm
Malignant
86.67% (13/15)
100% (2/2)
88.23% (15/17)
100% (5/5)
100% (3/3)
100% (8/8)
100% (3/3)
100% (3/3)
100% (2/2)
100% (3/3)
100% (5/5)
90.09% (20/22)
100% (11/11)
93.94% (31/33)
N/A
All
Whole database
11
12
13
14
Table 2 Three different FPs measurements under two detection sensitivity rates of the
proposed split method.
84.85% detection sensitivity:
false positive rate (FPs)
per
case
15
per
clock
per
hundred
section
slices
93.94% detection sensitivity:
false positive rate (FPs)
per
case
per
clock
per
hundred
section
slices
Benign
80.45
3.35
2.21
151.35
6.31
4.16
Malignant
82.64
3.44
2.27
157.36
6.56
4.33
Whole
database
81.23
3.38
2.23
153.48
6.40
4.22
Note,
23
1
2
1 patient case = 24 clock sections
1 patient case≒3000 image slices
3
24
1
2
3
4
Table 3 The detection performance with estimated detection difficulty of the lesions
by the physician of the proposed split method.
Internal echo
pattern
Margin
Calcification
Shadowing
Positive
84.62%(11/13)
90.00% (9/10)
100% (2/2)
100% (7/7)
Negative
100% (20/20)
95.65% (22/23)
93.55% (29/31)
92.31% (24/26)
5
25
1
11
12
1
10
2
9
3
8
4
7
2
3
6
5
Fig. 1
4
26
1
2
3
(a)
(b)
Fig. 2
4
27
(c)
1
2
3
(a)
4
5
6
(b)
(c)
(d)
Fig. 3
7
28
1
2
3
(a)
4
5
(b)
6
Fig. 4
7
29
1
(i)
2
(ii)
3
4
(a)
5
(i)
6
(ii)
7
8
9
10
(b)
Fig. 5
30
1
2
3
(a)
4
5
6
(b)
Fig. 6
7
31
1
2
3
4
(a)
(b)
Fig. 7
32