M&M General Guidelines
advertisement

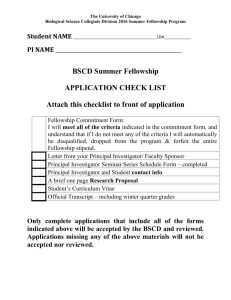
Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide Why: Morbidity and Mortality (M&M) Conferences are an Accreditation Council for Graduate Medical Education (ACGME) mandated educational series that occur regularly at all institutions that have residency training programs. The potential for learning from medical errors, complications, and unanticipated outcomes is immense—provided that the focus is on education, as opposed to culpability. (Morbidity and Mortality Conference, Grand Rounds, and the ACGME's Core Competencies. J Gen Intern Med. 2006 November; 21(11): 1192–1194.) Format: The allotted time for the M&M conference is 30 min per case/fellow /4 cases in 2 hours. Ideally the case presentation should last no more than 15 minutes, and should raise questions specific to either systemic or clinical errors pertinent to the case. After the case presentation, there should be time for questions and discussion. The Faculty Moderator will facilitate a discussion of the case. After this discussion, a concise review of the evidence based literature and teaching points should be presented for one or two of the salient clinical points in the case. Faculty Moderator Role: Assist the resident in identifying an appropriate case Review the residents presentation in advance and be prepared for the topic No “finger-pointing” – focus on systems of care rather than individual errors Open the Conference with an overview of the purpose of M&M and brief points about why the case selected Facilitate and engage the audience in the discussion using active adult learning methods(see faculty for tips) Close with Key Take Home Points Resident Presenter Role: Prepare the case presentation using the M&M Conference Preparation Worksheet Review the presentation with the assigned Faculty Moderator in advance Provide copies of any relevant articles cited Encourage to reflect on a monthly case per rotation that can help the fellow to focus in how to analyzed and learn from his/her practice. Keep cases in the portfolios. How to find a case: Talk the assigned Faculty Moderator, chief residents, Chief of Service(s) or Division Directors for case ideas. Cases (inpatient (ACE , consults), outpatient, long term care, ECTC , home care etc ), should involve: A. a poor or unintended outcome which might have been due to or worsened by error or system problems, or B. “near-misses,” where there was an error or misstep in care delivery that could have led to a poor patient outcome, or C. an interesting and unique case that may provide new learning and inquiry. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 1 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide D. Or any issue that relates with “Patient Safety Primers and clinical indicators”: Patient Safety Primers guide you through key concepts in patient safety. Each primer defines a topic, offers background information on its epidemiology and context, and highlights relevant content from both AHRQ PSNet and AHRQ WebM&M. http://www.webmm.ahrq.gov/perspectivesHome.aspx • Adverse Events after Hospital Discharge Being discharged from the hospital can be dangerous for patients. Nearly 20% of patients experience an adverse event in the first 3 weeks after discharge, including medication errors, health care–associated infections, and procedural complications. • Checklists Though a seemingly simple intervention, checklists have played a leading role in the most significant successes of the patient safety movement, including the near-elimination of central line–associated bloodstream infections in many intensive care units. • Computerized Provider Order Entry Computerized provider order entry systems ensure standardized, legible, and complete orders, and—especially when paired with decision support systems—have the potential to sharply reduce medication prescribing errors. • Diagnostic Errors Thousands of patients die every year due to diagnostic errors. While clinicians’ cognitive biases play a role in many diagnostic errors, underlying health care system problems also contribute to missed and delayed diagnoses. • Disruptive and Unprofessional Behavior Popular media often depicts physicians as brilliant, intimidating, and condescending in equal measures. This stereotype, though undoubtedly dramatic and even amusing, obscures the fact that disruptive and unprofessional behavior by clinicians poses a definite threat to patient safety. • Error Disclosure Many victims of medical errors never learn of the mistake, because the error is simply not disclosed. Physicians have traditionally shied away from discussing errors with patients, due to fear of precipitating a malpractice lawsuit and embarrassment and discomfort with the disclosure process. • Handoffs and Signouts Discontinuity is an unfortunate but necessary reality of hospital care. No provider can stay in the hospital around the clock, creating the potential for errors when clinical information is transmitted incompletely or incorrectly between clinicians. • Health Care-Associated Infections Although long accepted by clinicians as an inevitable hazard of hospitalization, recent efforts demonstrate that relatively simple measures can prevent the majority of health care–associated infections. As a result, hospitals are under intense pressure to reduce the burden of these infections. • Human Factors Engineering Human factors engineering is the discipline that attempts to identify and address safety problems that arise due to the interaction between people, technology, and work environments. • Medication Reconciliation Unintended inconsistencies in medication regimens occur with any transition in care. Medication reconciliation refers to the process of avoiding such inadvertent inconsistencies by reviewing the patient's current medication regimen and comparing it with the regimen being considered for the new setting of care. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 2 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide • Never Events The list of never events has expanded over time to include adverse events that are unambiguous, serious, and usually preventable. While most are rare, when never events occur, they are devastating to patients and indicate serious underlying organizational safety problems. • Patient Safety in Ambulatory Care The vast majority of health care takes place in the outpatient, or ambulatory, setting, and a growing body of research has identified and characterized factors that influence safety in office practice, the types of errors commonly encountered in ambulatory care, and potential strategies for improving ambulatory safety. • Physician Work Hours and Patient Safety Long and unpredictable work hours have been a staple of medical training for centuries. However, little attention was paid to the patient safety effects of fatigue among residents until March 1984, when Libby Zion died due to a medication-prescribing error while under the care of residents in the midst of a 36-hour shift. • Rapid Response Systems Rapid response teams represent an intuitively simple concept: when a patient demonstrates signs of imminent clinical deterioration, a team of providers is summoned to the bedside to immediately assess and treat the patient with the goal of preventing adverse clinical outcomes. • The Role of the Patient in Safety Efforts to engage patients in safety efforts have focused on three areas: enlisting patients in detecting adverse events, empowering patients to ensure safe care, and emphasizing patient involvement as a means of improving the culture of safety. • Root Cause Analysis Initially developed to analyze industrial accidents, root cause analysis is now widely deployed as an error analysis tool in health care. A central tenet of RCA is to identify underlying problems that increase the likelihood of errors while avoiding the trap of focusing on mistakes by individuals. • Safety Culture High-reliability organizations consistently minimize adverse events despite carrying out intrinsically hazardous work. Such organizations establish a culture of safety by maintaining a commitment to safety at all levels, from frontline providers to managers and executives. • Systems Approach Medicine has traditionally treated errors as failings on the part of individual providers, reflecting inadequate knowledge or skill. The systems approach, by contrast, takes the view that most errors reflect predictable human failings in the context of poorly designed systems. • Teamwork Training Providing safe health care depends on highly trained individuals with disparate roles and responsibilities acting together in the best interests of the patient. The need for improved teamwork has led to the application of teamwork training principles, originally developed in aviation, to a variety of health care settings. • Voluntary Patient Safety Event Reporting (Incident Reporting) Patient safety event reporting systems are ubiquitous in hospitals and are a mainstay of efforts to detect safety and quality problems. However, while event reports may highlight specific safety concerns, they do not provide insights into the epidemiology of safety problems. • Wrong-Site, Wrong-Procedure, and Wrong-Patient Surgery Few medical errors are as terrifying as those that involve patients who have undergone surgery on the wrong body part, undergone the incorrect procedure, or had a procedure intended for another patient. These "wrong-site, wrong-procedure, wrong-patient errors" (WSPEs) are rightly termed never events. When to start: At least 1 month prior to your scheduled presentation date. How to organize your presentation: Use the M&M Conference Preparation Worksheet to develop your PowerPoint presentation from. Use the M&M Conference standard PowerPoint template. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 3 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide What to include: Include the history, vital signs, physical exam, labs, x-rays, CT scans, EKGs, and consultant opinions as they were obtained during in the patient’s course. You should obtain the relevant images for xrays, EKGs, and CTs for display in your presentation or relevant imaging if applicable. Ask colleagues or a team member ( including pharmacy, nursing, chaplain, social work etc) for help in obtaining all the information. Remember that to construct the case for the audience, it is crucial to chart a time course, so that the case can be followed as it evolves over minutes to hours. How to research your discussion: Each M&M presents one or two opportunities for an evidence-based discussion of in the field of geriatrics. Do not approach this as a core lecture. If the chosen topic is unfamiliar to you, of course you should read up on it in a review article. But quickly move on to more specialized and upto-date resources, which will make up the foundation of your discussion. The completion of a root cause analysis should aide in your ability to determine all the factors impacting the case. Use update, MDConsult or other more advance search like Cochrane database, systematic reviews, Quality improvement tools etc. Resources: http://www.webmm.ahrq.gov/primerHome.aspx Root Cause Analysis: Root Cause Analysis is a technique that helps answer the question of why the problem occurred in the first place and seeks to identify the origin of a problem. It uses a specific set of steps, to find the primary cause of the problem, so that you can: 1. Determine what happened. 2. Determine why it happened. 3. Figure out what to do to reduce the likelihood that it will happen again. You'll usually find three basic types of causes: Physical causes - Tangible, material items failed in some way (for example, the fetal monitor stopped working). Human causes - People did something wrong or did not doing something that was needed. Human causes typically lead to physical causes (for example, no one checked to be sure the maintenance was performed on the fetal monitor, who led to it failing). Organizational causes - A system, process, or policy that people use to make decisions or do their work is faulty (for example, no one person was responsible for maintenance, and everyone assumed someone else had checked the fetal monitor). You may also want to use a Fishbone Diagram to assist with your analysis of the root cause. ( tools to do this include QI macros, exel) Draw the diagram with a process arrow to the effect and draw a box around it. Decide what the major categories of the causes are (i.e., people, machines, measurement, materials, methods, environment, policies, etc.). Label categories important to your situation. Make it work for you. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 4 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide Brainstorm all possible causes and label each cause under the appropriate category. Analyze causes and eliminate trivial and/or frivolous ideas. Rank causes and circle the most likely ones for further consideration and study. Investigate the circled causes. Resources: http://www.ihi.org/knowledge/Pages/Tools/default.aspx Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 5 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide Example of a Fishbone Diagram Tips: • Know the case well, especially the timeline. • Chart documentation only takes you so far -- speak with the involved residents and attendings and other nursing and ancillary staff so that you know their thought process. • Ask for help early if you need guidance. • Practice your presentation early and often. • Tactfully point out errors or near misses, but do it without blaming or being smug. • Control the room while you are presenting. Try to limit early, frequent interruptions as these questions are often answered later in the course of the case. It’s your room! • Leave time for discussion and questions at the end. This is when people can fire away with their comments, clarifications, questions, and pontifications. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 6 Geriatrics Fellowship UTHSCSA M&M Conference Preparation Guide When to finish: Review your entire presentation (slides, images, videos, etc…) to the Faculty Moderator at least 1 week prior to your talk. This allows a second pair of eyes to review your slides, ensures that there are no computer mishaps, and gives you enough time to practice delivery. Version 8-8-11 All cases are confidential and names have been removed. For Educational purposes only. 7