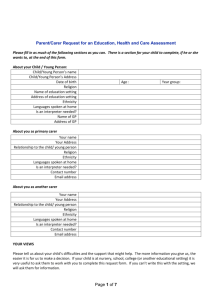
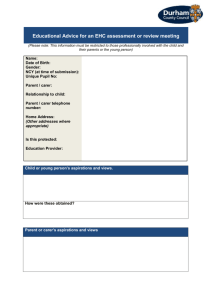
The Single Integrated Assessment and Plan Process
advertisement

DEVON ASSESSMENT FRAMEWORK (DAF) PRACTICAL GUIDANCE Incorporating the Family Health Needs Assessment, Common Assessment Framework (CAF) and links to the Special Educational Needs & Disabilities Pathway (0-25yrs) This document has been developed for managers and staff working with children and young people in Devon. It supports the implementation of the Devon Assessment Framework (DAF) and integrated working processes centred on the needs of children and young people. It will help practitioners to organise multi agency activity and service provision in a coordinated manner to ensure that children and young people achieve better outcomes. It will provide most of the information required for multi agency staff to complete the DAF forms The guidance covers Health Visitors undertaking a Universal Plan as part of the Family Health Needs Assessment Professionals undertaking a Common Assessment of need following the National Framework for Assessment Professionals supporting children and young people with Special Educational Needs and Disabilities (SEND) following guidance as set out in the SEN Code of Practice. DAF Guidance – DRAFT Version 0.5 – 30/10/2013 CONTENTS 1. GUIDING LEGISLATION AND REGULATIONS 1.1. Framework for the Assessment of Children in Need & their Families (2000) 1.2. Draft Special Educational Needs (SEN) Code of Practice: for 0 to 25 years (2013) 2. 3. PRINCIPLES INFORMATION SHARING AGREEMENT 4. PERSON CENTRED PLANNING 5. DAF 1 FAMILY INFORMATION 6. 7. DAF 1 ASSESSMENT DAF 2a ‘MY PLAN’ 8. DAF 2b ‘MY EDUCATION, HEALTH & CARE (EHC) PLAN’ 9. DAF 3 ‘REQUEST FOR ADDITIONAL RESOURCES’ 10. DAF 4 ‘TRANSITIONS ASSESSMENT’ DAF Guidance – DRAFT Version 6 – 13/02/2014 2|Page 1. GUIDING LEGISLATION AND REGULATIONS 1.1. Framework for the Assessment of Children in Need & their Families (2000) The Framework for the Assessment of Children in Need and their Families (Department of Health) covers the areas shown in the diagram below and is the model some other assessment tools follow or build on. The framework is based on three domains: - Child’s developmental needs; - Parenting capacity; - Family and environmental factors. The framework is intended to provide “a systematic way of analysing, understanding and recording what is happening to children and young people within their families and the wider context of the community in which they live” The Department of Health (DoH) Framework states that to assess the needs of a young person effectively requires a thorough understanding of: - The developmental needs of children - The capacities of parents or caregivers to respond appropriately to those needs; - The impact of wider family and environmental factors on parenting capacity and children. DAF Guidance – DRAFT Version 6 – 13/02/2014 3|Page 1.2.Draft Special Educational Needs (SEN) Code of Practice: for 0 to 25 years (2013) The draft SEN Code of Practice was published in October 2013. It details the responsibility of the Local Authority and its partners, in relation to children and young people with special educational needs. This means that whenever settings, schools and local authorities decide how to exercise their functions relating to children with special educational needs, they must consider what the Code of Practice says. The Code of Practice requires schools to identify and assess pupils’ needs and to arrange for increasing specialist expertise to be deployed within the school to help meet the difficulties pupils may be experiencing. The trigger for intervention is if a child requires provision that is additional to and different from that normally provided, based on teachers’ professional judgement. In the Devon SEND process that will link to the development of ‘My Plan’ and in some cases an Education, Health and Care (EHC) plan. It is for schools, colleges and early year’s providers, as part of their normal budget planning, to determine their approach to using their resources to support the progress of children and young people with SEN. In deciding whether to make a statutory assessment of a child’s SEN the local authority will seek to satisfy themselves that there is convincing evidence that despite the school or setting, with the help of external specialists, taking relevant and purposeful action to meet the child’s learning difficulties, those difficulties remain, have not been remedied sufficiently for the child to make adequate progress and may require the authority to determine what special educational provision should be made for them. Statutory assessment should not be the first step in the process; rather it should follow on from planning already undertaken with parents and young people in conjunction with an early year’s provider, school, post 16 institution or other provider. The local authority will conduct a statutory assessment when it considers the special educational provision required to meet the child or young person’s needs cannot reasonably be provided from the resources normally available to early years providers, schools and post 16 institutions. In considering whether a statutory assessment is necessary, the local authority will pay particular attention to: a. The views, wishes and feelings of the child and his or her parents or the young person. b. Evidence of the child or young person’s academic attainment and rate of progress c. Information about the nature, extent and cause of the child or young person’s SEN d. Evidence of the action already taken by the early years provider, school or post 16 institution to meet the SEN e. Evidence that where progress has been made, it has only been the result of much additional effort at a sustained level over and above that which is usually provided f. Evidence of the child or young person’s physical, emotional and social development and health needs g. Where a young person is over 18, their age and whether remaining in education would help them to progress. DAF Guidance – DRAFT Version 6 – 13/02/2014 4|Page 2. PRINCIPLES It has been recognised that there need to be a common set of principles for successfully delivering a family centred approach to a single assessment and planning framework. The key areas are; Children, families and young people are at the centre of the assessment and planning process and should be partners in making decisions throughout, including the decisions about the content of the plan. Assessment and planning should be an on-going process which builds on previous assessments and continues to identify and meet the needs of children, young people and families as they develop. Practitioners should be engaged and committed to the co-ordinated assessment and planning process. As far as possible, there should be a ‘tell us once’ approach to sharing information, so families and young people don’t have to repeat the same information to different agencies, or different practitioners/services within each agency. Effective co-ordination and joint working between education, health and social care services, to reach agreement on key outcomes with children, parents and young people and to secure the appropriate provision to deliver those outcomes. Plans should be focussed on outcomes (both short term outcomes and longer term aspirations for children and young people). Outcomes need to be specific, measurable, achievable, realistic and time-bound (SMART). Plans should build on the strengths of the child or young person as well as identify difficulties. Plans should explore how informal (family and community) support as well as formal support from statutory agencies can be used to achieve the agreed outcomes. The workforce should have the necessary skills. 3. INFORMATION SHARING AGREEMENT You will need to explain why it is important to share information and get the parent/carer (and child or young person where relevant) to sign the ‘DAF Information Sharing Consent Form’ before proceeding with the assessment. What is an Information Sharing Protocol or Agreement? An Information Sharing Protocol or Agreement provides a framework for the secure and confidential obtaining, holding, recording, storing and sharing of information between participating partner agencies or organisations. It is an agreed set of principles about sharing personal or confidential information and it enables each organisation signed up to the protocol to understand the circumstances in which it should share information and what its responsibilities are. Organisations involved in providing services to the public have a legal responsibility to ensure that their use of personal information is lawful, securely controlled and that an individual’s rights are respected. Why do we need to share information? DAF Guidance – DRAFT Version 6 – 13/02/2014 5|Page Sharing information about individuals between public authorities is often essential if we need to keep people safe, or ensure they get the best services. This sharing must only happen when it is legal and necessary to do so and adequate safeguards are in place to protect the security of the information. Parent carers and young people themselves should be informed about information sharing at the start of engagement, this could be in the form of a leaflet, which should include what information is shared with whom and by whom. The Government have recommended a set of golden rules to follow when sharing information: 1. Remember the Data Protection Act is not a barrier to sharing. It is a framework that ensures personal information about a living person is shared appropriately. 2. Be open and honest with the person (and/or their family where appropriate) from the outset about why, what, how and with whom information could be shared, and seek their agreement, unless it is unsafe or inappropriate to do so. 3. Seek advice if you are in any doubt whether you should or shouldn’t share 4. Share with consent where appropriate and where possible, respect the wishes of those who do not consent to share ‘confidential’ information. You may still share information without consent, if in your judgement that lack of consent can be overridden in the public interest. You will need to base your judgement on the facts of the case. 5. Consider safety and well-being: Base your information sharing decisions on considerations of the safety and well-being of the person and others who may be affected by their actions. 6. Necessary, proportionate, relevant, accurate, timely and secure: Ensure that the information you share is necessary for the purpose for which you are sharing it, is shared only with those people who need to have, is accurate and up-to-date, is shared in a timely fashion, and is shared securely. 7. Keep a record of your decision and the reasons for it-whether it is to share information or not. If you decide to share, then record what you have shared, with whom and for what purpose. If followed, these rules will ensure that any sharing you do will be appropriate and lawful. 4. PERSON CENTRED PLANNING At the start of our dialogue with families we want to have dynamic conversations where families and young people feel they have a voice which is heard and responded to. Some families may need support for this to occur but the main essence is to enable all families and young people to have the same approach at developing person centred/self-directed planning. GOLDEN RULES OF ADVOCACY Make time to develop a positive relationship with the young person. Understand how the young person likes to communicate and support this. Be independent and stay impartial. Listen to the young person’s opinions rather than your own. DAF Guidance – DRAFT Version 6 – 13/02/2014 6|Page Try not to take sides, or offer solutions. Confidentiality - Talk through this with the young person before you start working with them. Explain that you will keep what is said to yourself, unless it is likely to cause harm to anyone, including the young person. When writing a young person’s response for them, use the exact words the young person used. Evidence anything said on the young person’s behalf, through multiple examples, photos etc. The following sections provide specific guidance on how to complete the DAF forms. 5DAF 1 – FAMILY INFORMATION SECTION A – Children or young people in household This page should record all the children in the household. If a specific child is the reason for the start of the process the ‘Main Child or young person for this contact box’ should be crossed and ‘Reason for Contact’ box at the bottom of the page filled in. Ethnicity Codes White British (WB); White Irish (WI); Traveller of Irish Heritage (TIH); Gypsy/Roma (GP); Caribbean (C); African (A); Any other Black background (ANO); Indian (I); Pakistani (P); Bangladeshi (B); Any other Asian background (ANO*); White & Black Caribbean (WBC); White & Black African (WBA); White & Asian (WA); Any other Mixed background (ANO*); Chinese (CH); Any other Ethnic Group (ANO*), if ANO, please specify. Reason for contact – Give a brief explanation of what the concern is that has prompted you to complete this form. Young person’s contact details – You should only complete these details where the young person concerned is assessed under the Mental Capacity Act as capable of making decisions regarding their future. In such circumstances, they, and not their parents/carers, will be the first point of contact for any issues relating to their Plan. SECTION B & C – Parent carer/ Parents’ details if not main carers Use Section B to record the details of the child/young person’s parents and/or main carers and use Section C to record the details of the child/young person’s parents, where they are not the main carers. For example where a child lives with foster carers, the foster carers details will be recorded in Section B and the biological parents in Section C. Only record information that the parents/carers are happy to share with you. Use the same ethnicity and religion codes as in the guidance for Section A. Please ensure you record if the family are part of the Armed Forces as this links to additional education and social care support. SECTION D - Other Household members (including non-family members) Record the details of other known household members in this section. This may include children, adults, relatives, friends and lodgers, but only those who reside in the home. DAF Guidance – DRAFT Version 6 – 13/02/2014 7|Page The identification number in this section refers to when the household member is known to other services, for example, it could be an adult with physical or learning disabilities known to Adult Services and who have a ID number (CareFirst ID) SECTION E – Carers Record any specific caring duties carried out by members of the household. This should include children who care for siblings and/or adult relatives, adults who care for others including adult relatives. Include any other carers who may be involved with the family i.e. carers from agencies or personal assistants who support members of the household. SECTION F – Significant others/ Key contacts to the family Record people who the members of the family identify as providing significant support, advice and/or, guidance to the family, for example, other relatives, friends, advocates SECTION G – Services Working with the Family/Child/Young Person List all known services that are involved or who have been involved with the family, child or young person, this may include the following:Educational Psychologist Nursery/pre-school/school Portage Worker Special Educational Needs Coordinator Child & Adolescent Mental Health Service Sensory Impairment Service (VI/HI/PD) Communication and Interaction Team ASC Outreach Support SLCN Outreach Support Behaviour Support Service General Practitioner Health Visitor Hearing/Vision Professional Occupational Therapist Other Consultant Paediatrician Physiotherapist Psychiatrist Psychologist School Nurse Speech and Language Therapist Learning Disability Nurse Community Children’s Nurse Community Care Worker Family Support Worker Foster Carer Social Worker Specialist Child Assessment Centre SECTION H - FAMILY TREE Please identify, using the key, the current family structure. Please note the key is currently under review in the wider context of the local authority and may not represent all possibilities within the family structure at this time. SECTION I - Does the Child/Young person listed have a disability? The Local Authority has a statutory duty to collect information about of all children and young people who have a disability and for whom they are responsible. You should use the following tables to determine if their disability is moderate, severe or profound. Disability Living Allowance (DLA)/ Personal Independence Payment (PIP) If the child/young person receives Disability Living Allowance (DLA) or Personal Independence Payment (PIP) please record the rate of each component. Disability Register (Joint Agency Register) Using the following guidance, identify the level of observed functional difficulty and areas of Disability. Include Confirmed or Likely (C/L) Diagnosis with the name of the medical practitioner who has recommended these. DAF Guidance – DRAFT Version 6 – 13/02/2014 8|Page The Disability Discrimination Act (2005) defines the following categories as needing to be recorded:MOBILITY Getting about the house and beyond HAND FUNCTION Holding and touching. PERSONAL CARE Eating, washing, going to the toilet, dressing, etc. INCONTINENCE Controlling the passage of urine or faeces. COMMUNICATION Speaking and/or understanding others. LEARNING Having special educational needs, etc. HEARING Ability to hear VISION Ability to see A condition entailing behavioural difficulties including Attention Deficit Hyperactivity Disorder (ADHD). One or more of the child’s disabilities under the Disability Discrimination Act 2005 does not fall into any of the above categories e.g.Epilepsy BEHAVIOUR OTHER DDA In Devon we record the functional and diagnosed needs of a child and use the following guidance. AREA OF DIFFICULTY – MOBILITY These categories are based on the child’s ability to control his own body with and without the form of assistance, such as walking aids/wheelchair, and so on. Included within the grouping, especially at the younger age range are locomotor skills, such as crawling, running, hopping, skipping, and so on Level of Difficulty Indicators Moderate A child with a moderate ‘locomotion and mobility impairment’ may exhibit (Level 2) some of the following: Pre-school: Demonstrate a range of difficulties in locomotor and mobility skills and is definitely functioning at a stage significantly less than that expected at chronological age. School age: Able to walk but may require the assistance of equipment for activities such as family walks or outings – or perhaps to function in a large school campus. Can transfer from chair to chair independently – but due to problems with stamina and possible tiredness may require the use of equipment or helper. Over six years: May require mobility equipment for some activities. DAF Guidance – DRAFT Version 6 – 13/02/2014 9|Page Severe (Level 3) A child with a severe ‘locomotion and mobility impairment’ would demonstrate some of the following: Pre-school: Demonstrates no age appropriate locomotor and mobility skills, for example, at one year demonstrates little ability for the development of sitting and shows no desire to take weight through feet. School age: May be able to ‘walk’ short distances, or within a room, but is heavily dependant upon walking aid or wheelchair. Cannot functionally ‘walk’ outdoors requires a chair. Is unable to transfer from chair to chair without the aid of equipment or carer. Profound (Level 4) Has no functional locomotor mobility and is completely dependant upon carer for all mobility needs. Will require the provision of wheelchair mobility both indoors and outdoors. Will require other adaptations and equipment in the home and school to facilitate mobility (for example, ramps, hoists, and so on) and to enable transfers. AREA OF DIFFICULTY – HAND FUNCTION Classification is determined by the degree of independence, or the need for supervision or assistance. Age appropriate tasks must be considered here. Tasks will include the ability to play with toys, write, use scissors and involve the ability to reach, grasp, and so on. Restrictions may be due to; weakness, tremor, poor co-ordination, missing limb, hemiplegia, and so on Level of Difficulty Indicators Moderate A child with a ‘moderate’ upper limb difficulty may demonstrate: (Level 2) Significant difficulty with age appropriate tasks and may require adapted toys and equipment: Over three years: Cannot build with ‘Duplo’. Over five years: Cannot do buttons. May require adapted cutlery and only manage a spoon or fork. Over eight years: Cannot successfully use a pen/pencil, may require the support of IT keyboard, and so on. Cannot use implements such as scissors. Cannot build with ‘Mechano’. Severe (Level 3) A child with a ‘severe’ upper limb difficulty may demonstrate: Virtually no ability to use hands and arms to effectively achieve age related tasks. Is dependent on equipment to function, but has some ability to access and use the equipment. DAF Guidance – DRAFT Version 6 – 13/02/2014 10 | P a g e Profound (Level 4) May require helper or equipment in order to eat. Can only use keyboard/joystick or other access such as simple switches for computer access or communication. May require simple switch for wheelchair mobility. Has no functional ability with hands and is completely dependant upon carer or some other form of switch control (for example, head or foot) to control mobility, communication or environment. AREA OF DIFFICULTY – PERSONAL CARE Classification will be determined by the degree of independence, or the need for supervision or assistance. Age appropriate tasks must be considered here. Tasks will include: washing, dressing, toileting and personal hygiene (including menstruation). Personal Care difficulties may be as a result of other difficulties such as poor hand function or mobility difficulties, but should still be classified here. Level of Difficulty Indicators Moderate A child with ‘moderate’ difficulty with personal care may demonstrate: (Level 2) Over eight years: Struggles to dress and requires regular supervision and help (with or without the use of aids) to complete the task. Cannot put on socks or shoes. Cannot drink from a standard cup or glass, but may manage a straw. Can only use a spoon or fork for eating (may require adapted cutlery or utensils). Cannot clean teeth (but may manage an electric toothbrush). Over ten years: Requires supervision and/or assistance to bathe or shower, but can take some responsibility. Requires help to clean themselves after toileting and may require adapted toilet facilities. Menstruating child: Unable to care totally for self and requires prompting. Severe (Level 3) A child with a ‘severe’ difficulty with personal care may demonstrate: Over seven years: Requires a helper/carer to help to dress, eat, bathe or shower (with / without aids). Over ten years: Heavily dependant upon carer or aids to dress, eat, bathe or shower . Over 12 years: Cannot self catheterise. Over 14 years: Requires assistance to fit/remove menstruation protection. DAF Guidance – DRAFT Version 6 – 13/02/2014 11 | P a g e Profound (Level 4) Totally dependant upon carer for all personal needs. Cannot assist by any means whatsoever. Will need the appropriate provision of support, aids, adaptations and equipment both in school and the home. Child who has very little if not totally unable to care for themselves. Over ten years: Totally dependent upon carer for eating, drinking, toileting and bathing. AREA OF DIFFICULTY – INCONTINENCE Classification will be determined by the degree of control, or the need for supervision, prompting and assistance. Age appropriate ability must be considered here. Continence in this section is the ability to control bladder and bowel function and is not the ability to get to/from and on/off the toilet. These difficulties would be included in ‘self-care or mobility’ section. Unless there is a clear diagnosis of a relevant medical condition, continence difficulties cannot be accurately classified prior to four years. Level of Difficulty Indicators Moderate A child with a ‘moderate’ incontinence problem may demonstrate: (Level 2) Marked difficulty influencing bladder or bowel control. Over five years: Regularly wets the bed at night and also wets during the day. Soils on a fairly regular basis (two to three times per week). Over eight years: Has occasional day time wetting (once/twice a week). Has occasional night time wetting. Severe (Level 3) A child with a ‘severe’ incontinence problem may demonstrate, little or no control: Over four/five years: No control over bladder and bowel function. Requiring continence protection of nappies pads, and so on. Over five/six years: Soils numerous times per week. Requiring continence protection of nappies. Over eight years: Wets numerous times per week (even with prompting). Uses device or manual stimulation, to manage bladder and bowel. Profound (Level 4) Demonstrates no awareness and/or ability to control bladder and bowel function. Requires constant “changing” or supervision AREA OF DIFFICULTY - COMMUNICATION DAF Guidance – DRAFT Version 6 – 13/02/2014 12 | P a g e Level of Difficulty Moderate (Level 2) Indicators A child with moderate communications difficulties may: Pre School Have difficulty understanding some spoken instructions especially those out of routine. Use language typical of much younger child, for example a delay of one to two years. Have speech sound development which is not following a normal pattern. Many sounds are substituted or omitted. Unintelligible to unfamiliar listener. Use signing or gesture to support speech. Severe (Level 3) School Age Misinterpret spoken instructions or only remember part of the instruction. Use language typical of a much younger child, for example, significantly reduced vocabulary, incomplete or simplified sentences. Have speech which is unintelligible to unfamiliar listener. Have identified stammering behaviour, for example, a high number of words affected and/or associated facial and body tension. A child with severe communication difficulties may: Pre-school Have difficulty following most everyday instructions. Heavily reliant on routine and visual clues for understanding. Use very little spoken language. Use only restricted vocabulary and have a marked delay in combining words to make sentences. Day of two years plus. Have a restricted range of speech sounds. Be unintelligible to family members. Use a sign or gesture system for most communication. School Age Have difficulty following instructions even when explained on an individual basis. Be heavily reliant on routine, context and visual clues to follow spoken instructions. Use a range and type of grammatical structures which are very limited for the child’s age. Have a restricted range of speech sounds. Be unintelligible most of the time. Have difficulties with social language which impinge on interacting and establishing relationships with others. Rely on a sign system or communication aid for most communication. Profound (Level 4) A child with profound communication difficulties may: Be able to indicate only basic needs through body language but have no functional speech or alternative communication. AREA OF DIFFICULTY - LEARNING DAF Guidance – DRAFT Version 6 – 13/02/2014 13 | P a g e Learning difficulties include problems with the rate of acquisition of skills and/or weaknesses in particular aspects of skill acquisition. This may include problems with processing information, either verbal or through other senses/media, and/or with retrieval (memory). The gap between chronological age and attainments usually widens with age. Level of Difficulty Indicators Moderate A child with moderate difficulties may be functioning some three years behind (Level 2) their peers by the age of five. They may: Have limited/disrupted attention skills. Have limited awareness of danger (for example, road safety). Be socially naïve and at risk of exploitation by others. Pre-school Engage in little pretend/constructive play. Show limited interest and competence in simple shape, colour and quantity matching activities. Prefer physical activities to drawing, books and so on. By age seven – school performance of a typical four year old: Recognise and attempt to write own first name. Attempt representational drawing. Be able to count but make mistakes applying skill to real objects/pictures. By age 11 – school performance of a typical seven year old: Be able to read simple text with picture cues. Be able to copy words. Be able to draw recognisable pictures. Be able to complete written sum involving numbers to ten. By age 14 – school performance of a typical eight year old: Be able to read simple text but struggles with unfamiliar words (fluency and comprehension may remain weak). Be able to write legibly about everyday occurrences (spelling may be incorrect). Be able to carry out simple number operations but dependent on taught procedures and unable to self-correct. DAF Guidance – DRAFT Version 6 – 13/02/2014 14 | P a g e Severe (Level 3) A child with severe difficulties may be functioning some four years behind their peers by the age of five. In addition to indicators given for moderate difficulties they may: Show frustration through challenging behaviour. Have particular difficulty developing understanding of concepts involved in reading, writing, time and money. Pre-school Mouth or throw toys/games/books. Show minimal interest and competence in simple shape, colour and quantity matching activities given adult assistance. Colour and quantity matching activities given adult assistance. By age seven – school performance of a typical three year old: Show some interest in making marks on paper. Enjoy number rhymes but dependent on adult to show correct number of fingers, objects, and so on. By age 11 – school performance of a typical five year old: Attempt to write own first name and undercopy words. Usually recognises own name, those of some classmates and a few familiar words. Be able to complete simple size, shape and quantity matching activities. By age 14 – school performance of a typical six year old: Be able to read familiar words in school/community environment (may require prompting and be dependent on additional cues, for example, symbols). Be able to use a computer to record activities (may be in symbol format rather than words). Can apply skill practised at school to community experience with supervision, for example, shopping, and travel. Profound (Level 4) A child with profound difficulties will remain developmentally young and is likely to be functioning below the level typical of a one year old as a preschooler, below the level typical of a two year old at seven years, below the level of a typical three year old at 11 years and below the level of a typical four year old at 14 years. They are likely to: Be dependent on others for stimulation. Be dependent on others interpreting their needs. Be dependent on others for personal safety. DAF Guidance – DRAFT Version 6 – 13/02/2014 15 | P a g e AREA OF DIFFICULTY - HEARING Level of Difficulty Moderate (Level 2) Indicators A child with moderate hearing loss may: Use hearing aids or other equipment to access speech. Have difficulty producing some speech sounds. Need visual clues to aid speech reception - therefore need to be at the front of the class close to speaker. Manage well with one-to-one conversation but lose the thread with group discussion. Respond to environmental sounds without hearing aids. Be able to make use of the telephone. Have TV on extra-loud to follow speech. Experience some behaviour difficulties (rejecting help - hearing aids, attention-seeking) Severe (Level 3) A child with a severe hearing loss may: Only be able to detect environmental sound with hearing aids. Only acquire limited speech. Will be unlikely to be able to use a telephone. Use subtitles for TV watching. Be a Cochlear Implant user. Profound (Level 4) A child who is profoundly deaf may: Not respond to sound even with the use of hearing aids. Detect limited environmental sound. Not acquire speech. Experience difficulties in abstract thought and therefore behave inappropriately – traffic safety, stranger danger. Belong to a clearly defined group of signing peers. AREA OF DIFFICULTY - VISION Level of Difficulty Moderate (Level 2) Indicators A child with a moderate impairment may have reduced distance vision and/or near vision and/or field defects and therefore may: Have difficulty reading the board. Have difficulty in reading smaller print sizes without magnification. Have difficulty reading own handwriting and writing on lines. Have difficulty in participating in ball games. Have difficulty following events at a distance such as football matches. Have difficulty watching Television programmes. Have difficulty completing tasks on time. DAF Guidance – DRAFT Version 6 – 13/02/2014 16 | P a g e Severe (Level 3) A child with a severe impairment may have reduced distance vision and/or near vision and/or field defects and therefore may: Have difficulty in recognising faces. Have difficulty in making eye contact and interpreting facial expressions and body language, which may affect social and interpersonal skills. Have difficulty in reading standard print sizes without magnification. Have perception of colour limited to shades of grey. Have severe photophobia, with or without extreme skin sensitivity, on exposure to sunlight. Have difficulty in scanning for and fixating stationary distant objects and tracking moving ones. Have difficulty in scanning and fixating near objects. Have difficulty in carrying out tasks, which require hand eye coordination, such as pouring liquids. Have difficulty in carrying out daily living activities, such as using a selfservice school canteen. Have mobility and orientation difficulties in unfamiliar areas or in areas with poor illumination. Have difficulty travelling independently without mobility and orientation training and mobility aids. Have developmental delays in fine and gross motor skills. Have difficulty completing tasks on time. Profound (Level 4) A child with a profound visual loss may: Have no perception of light. Have perception of light only. Have perception of hand movements only. Have extensive loss of near and distance acuity, for example, no functional central vision. Have field losses causing extensive loss of peripheral near and distance vision, such as, Tunnel vision. Have poorly developed social, inter-personal, spatial and environmental concepts arising from impaired visual perception. Have to use tactile methods of communication such as Braille, although some may access large print under optimal conditions with the appropriate technology. Have difficulty performing everyday living activities independently without specialist training and equipment. Have difficulty travelling independently without mobility and orientation training and mobility aids. Have difficulty completing tasks without extra time and assistance. AREA OF DIFFICULTY: BEHAVIOURAL This section is organised slightly differently from the preceding sections as factors such as context, longitudinal history and complexity are better determinants of severity of problem than the actual indicators themselves. In order to assign a severity weighting to a child/young persons difficulties the following procedure should be followed: DAF Guidance – DRAFT Version 6 – 13/02/2014 17 | P a g e 1. Write a narrative account of the situation to include what the child/young person does which is of concern, what they and other people feel about the behaviours and what has been done to try and resolve problems. Include information about settings which appear to exacerbate problems (with whom, where, when) and those where the worrying behaviours do not occur. Detail the frequency and duration of problem behaviours and compare and contrast with earlier periods in time. 2. Use the following notes to check whether you have covered all relevant areas, expanding your narrative if any aspects have been missed. 3. Assign a moderate coding to situations where problems are clearly long-term (for example, have been a constant feature,, or for at least three months). 4. Assign a severe coding if, in addition to the above, there is clear evidence that appropriate interventions have been implemented without reducing (not necessarily removing) the behaviours of concern. In situations where the child/young person has been resistant to the intervention, or the family unable to support and implement advice, use a moderate coding. 5. Assign a profound coding if, in addition to all of the above, the behaviours cover several areas of difficulty. In all cases it is important to focus on behaviours which are quantitatively and qualitatively different from normal developmental behaviours, taking into account degree and persistence over time as well as age and duration of onset. Indicators Relating to Emotions Regular repeated nightmares. Inability to concentrate. Neglecting own needs. Refusal to co-operate/comply. Constantly challenging authority. Bullying/ being bullied. Sleeping difficulties. Bedwetting. Soiling and/or smearing faeces. Poor school attendance. Anxieties that inhibit every day activities. Withdrawal from family interaction. Exhibiting seriously risky/dangerous behaviour (to self or others). Fire setting. Continually interfering with others activities. Indicators Relating to Thoughts and Perceptions Expressing negative / pessimistic ideas. Pre-occupation with a specific interest. Unrealistically high or low expectations of own ability to achieve. Unpredictable / inconsistent / impulsive behaviour. A very different description events to others who were present Undue concern with appearance/body shape. Unclear boundaries between what they believe is reality or fantasy. Seeing all events as having personal impact. Controlling behaviour over food intake. Hearing/seeing things that are not there. Rigid thinking, not being distractible. Significant amounts of verbal communication that does not make sense. Total withdrawal, no communication, bodily rigidity. DAF Guidance – DRAFT Version 6 – 13/02/2014 18 | P a g e Distorted sense of personal identity. Indicators Relating to Social Skills Withdrawal from social situations. Lack of awareness of the needs of others. Unable to judge social context accurately. Exhibiting promiscuous/provocative behaviour. Excessive fear of adults. Being verbally/physically aggressive to others. AREA OF DIFFICULTY: OTHER DDA (Eating, Drinking and Ingestion) The assumption is that the food and/or drink has already been placed in the mouth by the child and/or carer (see personal care and upper limb function) this deals with oral control, swallowing, and so on. Psychological components in eating difficulties are covered in the emotional/behavioural section Level of Difficulty Indicators Moderate A child with moderate eating, drinking and ingestion difficulties may at each (Level 2) meal time have one of the following difficulties: Difficulty in the ability to produce controlled jaw movements and/or could not take food off a spoon with lips. (Usually able at six to seven months.) Has an abnormal amount of food or liquid spillage from the mouth, or the child’s helper has to frequently scrape food off the chin. (Usually by 18 months.) Gagging, choking or coughing once or twice at each meal/drink. Have long meal times which are longer than 30 minutes for a meal consisting of two courses and of age appropriate quantity. Not eat age appropriate consistencies/textures. Normal development: Stage 1 (around 3-4 months) – pureed foods, for example, pureed peas. Stage 2 (5-6 months) – thicker consistencies and lumpy textures Stage 3 (7-8 months) – mashed, minced or finely chopped foods, finger foods and chunks of fruit. Stage 4 (9-12 months) – chopped food and a varied diet. Severe (Level 3) A child with severe eating, drinking and ingestion difficulties may show two or more of the symptoms listed below: Difficulty in the ability to produce controlled jaw movements and/or could not take food off a spoon with lips. (Usually able at six to seven months). Has abnormal amount of food or liquid spillage from the mouth, or the child’s helper has to frequently scrape food off the chin. (18 months). Gagging, choking or coughing frequently during each meal/drink. Long meal times, longer than 30 minutes. For a meal consisting of two courses and of age appropriate quantity. Does not have age appropriate consistencies/textures. Normal development: Stage 1 (around 3-4 months) – pureed foods, for example, pureed peas. Stage 2 (5-6 months) – thicker consistencies and lumpy textures DAF Guidance – DRAFT Version 6 – 13/02/2014 19 | P a g e Profound (Level 4) Stage 3 (7-8 months) – mashed, minced or finely chopped foods, finger foods and chunks of fruit. Stage 4 (9-12 months) – chopped food and a varied diet. A child with profound eating, drinking and ingestion difficulties will have no oral intake of food. Fed through nasogastric tube or gastrostomy. 6. DAF 1 – ASSESSMENT / REVIEW List the individuals, who are being considered as part of the assessment, this may be the whole family, or an individual within the family. Record the name and contact details of the person leading this part of the process, they will be the initial person coordinating the assessment and could be the SENCO in a school setting or a support worker identified to lead this part of the process. Once the initial assessment is completed it may be agreed that the role of ‘Lead Professional’ is taken on by someone else. Record the date the assessment was started. This may be the date on which the first analysis of a child/young person’s emerging needs was initiated or the date on which the child/young person’s needs are reviewed. Also record the date of the first Team Around the Child (TAC) meeting. This may be the first meeting in the setting with parents to discuss any emerging issues. Any meeting or assessment gathering with the parent child or young person should be considered as a TAC. For subsequent meetings and reviews update the version number as part of the assessment record. SECTION A – Reason for doing Devon Assessment Framework (DAF) Outline what has led to the DAF being undertaken and the key areas to be looked into. This may be emerging issues relating to SEN, social care, health or other related needs. For Health Visitors you will record the status of the assessment in (i) as part of the Universal assessment process for the Healthy Child Programme Depending on your role, sections B – H will be completed at differing levels, for example, a Social Worker will utilise their training and professional practice to include a full analysis of strengths and needs whereas a worker within a school/setting at the initial stage of the process may want to note down any issues they are aware of at that point. SECTION B – Child / Young Person’s Health, Learning and Development Needs On pages 25-28 you will find age and stage guidance (0-4, 5-11, 11-16, 16-25) which includes reference to health visiting outcomes, early years and foundation stage developmental guidance, SEN Code of Practice and general development milestones. Depending on your role you will use this section to record any developmental information against those headings. If this is part of emerging SEN needs you will use the Code of Practice guidance as outlined in the age and stage guidance below. Your school or setting may have a clear framework for this and it should be incorporated into this document. You should only record judgements that relate to your area of knowledge and expertise or where there is supporting evidence from relevant DAF Guidance – DRAFT Version 6 – 13/02/2014 20 | P a g e professionals. If information is reported to you then you should make this clear e.g. mother reports that xxx has mental heath difficulties. For a child being identified as having SEND the Devon SEND toolkit supports schools in identifying the type and level of need. The SEN Categories of need are:SEN Category (Area of Need) Cognition and Learning Difficulties Social, Mental and Emotional health Communication and Interaction Needs Sensory and/or Physical Needs Other Description of Need SpLD Specific Learning Difficulties (Dyslexia) Moderate Learning Difficulties; which includes children MLD who have difficulty with some of the work in school, and with keeping up with other children their age. Severe Learning Difficulties; includes children who have SLD difficulty developing basic skills. PMLD Profound & Multiple Learning Difficulties BESD Behavioural, Emotional & Social Difficulty ADHD Attention Deficit Hyperactivity Disorder Speech, Language and Communication Needs; including SLCN expressing themselves or understanding what others are saying. Autistic Spectrum Condition, difficulties with social ASC communication, making friends or relating to adults. VI Visual Impairment HI Hearing Impairment MSI Multi-Sensory Impairment PD Physical Disability MED Complex Medical You should not record the child or young person as having conditions such as ASC, ADHD etc. unless you have a formal diagnosis. SECTION C – Parenting Capacity / Parents and Carers This section focuses on the strengths and needs of those parenting the child/young person and included in the guidance on page 29 are some specific areas to support your analysis. Only record judgements that you have discussed and agreed with the parent/carer. SECTION D – Child / Young Persons Home and Community This section is to record any family or environmental factors outlined in the guidance on page 30, which may have an impact on the child/young person and/or family. According to your role this will be recorded at the appropriate level of your analysis. Only record judgements that you have discussed and agreed with the parent/carer. The above areas are the key parts of the National Framework for Assessment. The following pages contain the specific guidance set out to capture all relevant age and stage information. These areas relate directly to the Assessment part of the Devon Assessment Framework. Professionals must have regard to these areas to ensure that all information currently available is captured and that any additional information is requested through the most appropriate channels, for example Early Help Co-ordinators, Single Point of Access or area based support from Babcock LDP. DAF Guidance – DRAFT Version 6 – 13/02/2014 21 | P a g e Guidance is relevant for health visitors undertaking Family Health Needs Assessments, Early Years Professionals, School Based professionals, Special Educational Needs Coordinators, All community based health and social care staff, and other staff including the Police, Housing Officers , Employment officers, Youth Workers and others engaged in supporting children young people and their families. DAF Guidance – DRAFT Version 6 – 13/02/2014 22 | P a g e CHILDS HEALTH, LEARNING AND DEVELOPMENT (EARLY YEARS, 0 – 4 YRS) General Health Conditions /Specific Diagnosis / TB Risk Known or Family History i.e. Asthma, eczema, hay fever, allergies. Childhood deafness, fits, eye problems, reading and spelling difficulties, speech and language difficulties, physical development Consider Parental Mental health and Wellbeing Health Visitors Use Contact Codes Physical Development / Physical, Sensory & Medical Learning and Play Does your child continue to play when you leave? Share toys? What does your child choose to play with? Does your child have a favourite book, toy, song, TV/DVD? Do they pretend? Do they like to pretend to do the things you do? Do they use one object to pretend it is another, e.g. plastic banana for a telephone? Can your child watch or listen to other people? Do they prefer to choose what they want to do? Do they identify any letters and sounds? Recognise their name when it is written? Recognise any numbers? Count objects? Does the child attend nursery? Does the child respond to adult instruction? Can the child concentrate for short periods? Does the child show an interest in stories & play materials? Communication and Language / Interaction EYFS Listening and Attention Understanding Speaking Listening / Understanding Does your child turn their head towards sound? Look towards the caregiver when hearing their voice? Respond to their name being called? Does your child understand ‘no’ and ‘yes’? Do they understand you when you speak to them? Does your child look at you? Smile at you? Look at toys/people and objects with you? Do they show you things they are interested in? Do they understand routine / simple instructions? Speech and Language Does your child make noises or sounds of pleasure, gurgle and babble, say the name of familiar people/objects? Make sounds to get attention from others? String 2-3 words together? Speak in sentences? Use 50-100 words? Can they be understood by people who know them? Can they be understood by people who do not know them? Do they point or gesture? Social, Mental & Emotional Health EYFS Self Confidence/Self Awareness Managing Feelings and Behaviour Making Relationships Behaviour Is your child generally happy & calm? Do you think your child’s behaviour is appropriate for his/her age? Does your child understand rules and routine? What happens when they are refused something that they want? Do they do what you ask them to do? Can you take your child to unfamiliar places without worrying about how they might behave? Does your child behave the same or differently in new places? How do they react if asked to do something they do not want to do? Do they hurt others? Social Does your baby smile at you/others? Does your child have a favourite toy? Does your child maintain eye contact? Do they show interest in others? Do they track objects as they move? Do they smile/make sounds in the company of others? Do they recognise familiar people? Show preference for certain people? Do they show affection towards others? Who do they get on best with? Do they play near other children? Join in simple shared songs and games? Emotional Health How do you know what your child is feeling? What makes your child happy? What makes them upset? Do they get upset DAF Guidance – DRAFT Version 6 – 13/02/2014 23 | P a g e Cognition & Learning (please consider the 3 other sections first as these are the Prime areas of learning) Engagement Does your child enjoy playing with you Does your child enjoy exploring and finding out about things around them Are they curious about new things, people and experiences and show interest and fascination Do they use their senses to explore the world around them – touch things, put things in their mouth, listen if they hear new sounds etc. Do they play with things in a range of ways including pretending objects are something else and enjoy exploring how to make things happen Are they developing favourite things – toys, food, visits, people Are they prepared to try new things and have a go Motivation Are they developing the ability to focus on activities, people, for longer periods of time Does your child persist at an activity even when it is hard, do they keep on trying. Do they show a sense of achievement when they have done something for the first time Are they starting to have their own ideas and solving problems for themselves i.e. finding a way to get a toy they want that is out of reach Are they beginning to make links with their experiences, grouping things, sequencing and exploring cause and effect Are they beginning to choose ways to do things, exploring possibilities and changing things if it is not working the way they want it to. Literacy (Communication and Language Development is the basis for all literacy and easily? When they are upset who do they go to? Who do they get on best with? Does he /she enjoy affection/physical contact in an ordinary way? therefore should be considered first) Does your child enjoy looking at books and printed materials with a familiar adult (from birth) Does your child join in with favourite rhymes or stories which are repetitive (up to 3 years) Does your child hold books, enjoy turning the pages and anticipate what will happen next (up to 2 years) Does your child tell you what they have drawn, painted or written (pretend writing) (from 2 years) Does your child recognise familiar signs, symbols or words (from 2 and half years) Mathematics Can your child recognise changes in number of objects/ images in a group of 3 (up to 1 year) Is your child starting to understand that things exist even when out of sight (12 – 18 months) Does your child organise and categorise things e.g. putting all the teddies together, separating teddies and cars into separate piles (up to 2 years) Can your child select a small number of (from 2 – 3 years) Can you child recite a few number names in sequence (2 – 3 years) Does your child understand things like more and a lot (2-3 years) Does your child recognise big and small things (up to 2 years) Does your child understand routines of the day (up to 2 years) Does your child play with inset puzzles and shape sorters (up to 2 years) Does your child use blocks to build and arrange (up to 2 years) Does your child enjoy filling and emptying containers (up to 2 years) Does your child use the language of size (up to 3 years) Does your child anticipate certain times of the day – bedtime, meal times, etc (up to 3 years) DAF Guidance – DRAFT Version 6 – 13/02/2014 24 | P a g e CHILDS HEALTH, LEARNING AND DEVELOPMENT (MIDDLE CHILDHOOD, 5 - 11 YRS) General Health Conditions /Specific Diagnosis / TB Risk Known or Family History i.e. Asthma, eczema, hay fever, allergies. Childhood deafness, fits, eye problems, reading and spelling difficulties, speech and language difficulties, physical development Consider Parental Mental health and Wellbeing Consider – Worries regarding health, hearing problems, dental problems, orthodontist. Sight problems, optician. Sleep problems/habits. Smoking, alcohol, illegal substances. Identity; self esteem. Does the child feel good about who they are, do they know how to get advice about how they feel. What type of education provision does the child attend – mainstream, special, alternative Do they attend full time, part time Home education Have there been any exclusions Physical, Sensory & Medical Physical Have you any concerns about the health of the child? Do they seem physically well? Eating? Drinking? Sleeping? Independence skills? Toileting – is the child wearing nappies day or night? Are they able to clean themselves? Dress themselves? Feed themselves? Communication & Interaction Communication Is your child able to listen and understand what others say? Instructions? Understands jokes? Is your child able to express themselves (feelings, wants, events) in sentences? Ask questions and respond to others answers? Pronounce words clearly? Eating & Drinking Is the child able to feed themselves? Can they use a knife/ fork/ spoon? Toileting Is the child wearing nappies, day/night? Do they wet/soil their clothing? Can they toilet independently? Fine motor skills Can your child make marks; write their name, form letters? Is their writing easy to read? Can the child thread beads, clip pegs? Gross Motor Skills What activities do they like, in school or home? Do they enjoy running, skipping, swimming and cycling? Have you noticed any movements which seem unusual? DAF Guidance – DRAFT Version 6 – 13/02/2014 Social, Mental & Emotional Health Behaviour Do they comply with rules and routines? Does your child get upset in school? Can you identify triggers/antecedents? Can they calm themselves down? Have they ever hurt others? Eating? Drinking? Sleeping? Does the child display any worrying or sexualised behaviour? Can the child share & take turns with others? Does the child have a realistic sense of personal danger? Has the child ever run away? Social Does your child have friends? Do they have several good friends or nobody particularly close? Is your child particularly close to one adult? Do they seek out adults to help them? Emotional Does your child enjoy school? What do they like about it? What don’t they like about it? What makes you think this? 25 | P a g e Cognition & Learning What national curriculum levels is your child currently achieving? Is your child learning? Is there an area of learning in which they are particularly weak, or do not enjoy? What interventions have been put in place? What was the outcome? Are their interventions you would like to try? Why have you not tried them? How do they respond to challenging work? Can they complete work independently? Is their concentration span similar to their peers? Does your child enjoy school? What do they like about it? What don’t they like about it? What makes you think this? Is there something they are good at in or out of school? How to they respond to challenging activities? Can they complete school / homework independently? YOUNG PERSON’S HEALTH, LEARNING AND DEVELOPMENT (ADOLESCENCE, 11 - 16 YRS) General Health Conditions /Specific Diagnosis / TB Risk Known or Family History i.e. Asthma, eczema, hay fever, allergies. Childhood deafness, fits, eye problems, reading and spelling difficulties, speech and language difficulties, physical development Consider Parental Mental health and Wellbeing Consider – Worries regarding health, hearing problems, dental problems, orthodontist. Sight problems, optician. Sleep problems/habits. Smoking, alcohol, illegal substances. Identity; self esteem. Does the child feel good about who they are, do they know how to get advice about how they feel. Do they know how to get advice about Sexual health issues, anger management, anxiety, bullying. Physical, Sensory & Medical Communication & Interaction Physical Is your young person generally well? What activities do they like doing best? Do they do any physical activities, e.g. walking, swimming, running, sport? Do you think they are a similar weight and height to others of their age? Do they need to wear glasses/hearing aids? Are they able to wash, brush teeth, dress eat and drink without help? Do they have a disability? Does your young person have a physical illness (temporary or long-term)? Do they suffer from mental health problems (temporary or long-term)? Does your young persont have an eating disorder? Do you think they have ever felt suicidal? Do you think your young person is misusing drugs or alcohol? Is or have they ever been pregnant? Has your son ever fathered a child? Is hospital attendance at the expected level? Do they have an accurate knowledge of puberty, sex and contraception? Are your young persont’s medical and dental appointments generally kept? Do they smoke? Have they had up to date immunisations? Communication Is your young person able to explain thoughts, feelings & events to others? Are they able to easily move from one topic to another? Can they hold conversations with peers and adults? Do they respond appropriately to adult instructions? What is their first language? Are they fluent in their first language? Do they have any help with their speech and language? DAF Guidance – DRAFT Version 6 – 13/02/2014 Social, Mental & Emotional Health Behaviour Do they bully other children? Is their behaviour/language age appropriate at home, school or in the wider community? Have they ever self-harmed? Have they ever been involved in criminal behaviour? Do you always know their whereabouts? Have they ever run away? Do they have a realistic sense of personal danger? Social Do you think they are bullied, isolated or alone at school? Does your young person have friends at school or work? Do you think your young person is liked by teachers and other pupils? Emotional Is your young person generally happy and calm? Do they enjoy affection/physical contact in an ordinary way? How would you describe their relationships with their peers and other adults? Does their sexual behaviour seem reasonable for someone of their age 26 | P a g e Cognition & Learning Does your young person attend mainstream school, a specialist setting or receive home tuition? Do they like school and want to learn? Do you feel they are reaching their potential? Do they receive any special support in school because of a specific learning difficulty or because they are above average intelligence? Is there an individual learning plan in place? Have they been excluded from school permanently / temporarily, or in an out of school education scheme? Do they attend school regularly and on time? Do you think they experience racism at school? Is your young person encouraged to find work if no longer at school? Have they achieved the relevant SATS tests or GCSE’s? Do they have difficulties concentrating? Is homework generally done and handed in on time? HEALTH, LEARNING AND DEVELOPMENT (YOUNG ADULT, 16 - 25 YRS) General Health Conditions /Specific Diagnosis / TB Risk Known or Family History i.e. Asthma, eczema, hay fever, allergies. Childhood deafness, fits, eye problems, reading and spelling difficulties, speech and language difficulties, physical development Consider Parental Mental health and Wellbeing Consider – Worries regarding health, hearing problems, dental problems, orthodontist. Sight problems , optician. Sleep problems/habits. Smoking, alcohol, illegal substances. Identity ; self esteem. Does the child feel good about who they are, do they know how to get advice about how they feel. Do they know how to get advice about Sexual health issues, anger management, anxiety, bullying. Physical, Sensory & Medical Physical Who do you live with? Are you physically well? Eating? Drinking (alcohol)? Sleeping? Do you feel you are the right weight for your height? Are you or someone you depend on presently receiving or waiting for specialist medical services like a hospital consultant or operation? Have you got access to a dentist and a doctor? When did you last see them? Are you taking medication regularly? What is it for? Do you see any doctors/therapists/nurses regularly? Are you getting all of the health services you think you need? If not, what are you missing and why do you think you are not getting them? Would you describe yourself as having a disability or special need? How do you spend your time? Is there an activity or sport that you don’t do but would like to? What is stopping you? Has the young person established entitlement for Continuing Health care funding from NHS Devon ? Is the young person eligible for CHC in adult services? Communication & Interaction Can the young person communicate independently Do they use Augmentative Communication equipment, BSL support or other strategies DAF Guidance – DRAFT Version 6 – 13/02/2014 Social, Mental & Emotional Health Under the Mental Capacity Act 2005 would the young person be deemed capable of making their own decisions Did they need support to make those decisions Has a Best Interest meeting been held Accommodation requirements – independent/supported living Managing personal care Financial and Benefits advice and support Cognition & Learning 27 | P a g e Are you able to prepare food? Use simple appliances? Wash clothes? Are you able to recognise all coins and notes? Count change? Use a current/saving account? Credit Card? Can you tell the time? Make telephone calls? Can you travel alone to familiar/unfamiliar destinations? Can you keep a job? Budget? What are your strengths and skills in you education setting? What additional support do you require to access learning? What work experience, voluntary work do you do? What are your current goals for education, employment, independence? What skills do you require to take up a career? What transport plans are in place to enable you to access your educational placement? What are your mobility training needs – wheelchair user, Hearing Impaired, Visually Impaired, Multi Sensory Impaired What are your aspirations skills and achievement PARENTING CAPACITY/PARENT CARERS How did you feel about your pregnancy/ parenthood? Have you had experience of babies/young children? What was your childhood experience like? Would you make any changes when parenting your own children? Are you/your partner still in close contact with your parents/extended family? If appropriate and safe to do so make enquiries about parental/domestic issues – routine question regarding domestic abuse/violence School Age child / Young person- Is there someone at home or anywhere else who you can talk to if you are worried or if something good has happened? Would you know where to go for help and support? Basic Care, ensuring safety and protection Provision of Food, drink Warmth shelter Appropriate clothing Emotional Warmth and Stability Sable affectionate and stimulating family / home environment Guidance, Boundaries and Stimulation Family History / Current Roles Encouraging self-control Parental/Carer relationship Modelling positive behaviour Relationship with their own parents and siblings Effective and appropriate discipline Illness, bereavement, other significant life events that may have impacted on family life Praise and encouragement Personal and dental hygiene Secure attachments Engagement with Services and others Avoiding over protection Frequency of house moves Safe and Healthy environments and home Support for Positive Activities Frequency of school moves Can the parent keep the child safe from exploitation including sexual ? Job / employment moves and security Family engagement outside the home – community involvement sporting activities, days out , holidays etc Is there a culture of risk taking, violence, substance misuse, anti social behaviour which may impact on the care for children DAF Guidance – DRAFT Version 6 – 13/02/2014 Important people to the family – grandparents, absent parents / grandparents, other relatives , siblings impact and support to family Positive role models within the family Is life stimulating within the environment. 28 | P a g e CHILD/YOUNG PERSON’S HOME AND COMMUNITY – FAMILY AND ENVIRONMENTAL Family History of Health Problems Depression Mental Ill Health Recent major issues – bereavement, separation, moving house, accident, burglary, domestic violence Employment issues , return to work, additional education/learning / housing Diet exercise, healthy lifestyle, daily routine, socialisation, social networking Living environment – do you like where you live, good neighbours, who else lives there? Childcare support, benefits, advice re safety ( Smoke detector), Healthy Start leaflet Access to transport Regular contact with others and professionals, children’s centre, school college, social worker CPN Support regarding bullying ( mobile phone internet and personal), attendance at school / college, good food access school lunch packed lunch Has anything big happened recently to impact on the home and community History Functioning and Wellbeing Has there been illness, bereavement, Wider Family Formal and Informal networks from extended family and others Housing Employment and Financial Considerations Social and Community elements and resources including education Water, Heating, Sanitation facilities Day Care Sleeping arrangements Places of Worship Reason for homelessness, housing problems Transport Criminality, anti social behaviour Work and shift patterns Shops / Leisure Facilities Cultural issues Employment income – impact on the family Crime / anti social behaviour in the area Size and composition of household Benefits access Peer groups Absent family members Effects of hardship Social Networks / Community centres of social networking pubs/clubs Issues of violence, abusive behaviours Wider caring roles for others Parental substance misuse Employment roles and responsibilities Breakdowns of relationships Relationships Physical Disability Religion and wider faith communities Mental Illness DAF Guidance – DRAFT Version 6 – 13/02/2014 29 | P a g e SECTION E & F - Child and Young Person’s View / Parent Carers View Record the views of the child/young person and their parent/carers, and try to enable them to feel confident about areas where they have concerns and what they are looking for through this process as personal outcomes. This section should summarise the views noted in the person centred planning tool e.g. ‘Listen to Me and My Family’. Ensure that the main issues from both the child/young person and the parent/carer are summarised so that the plan can both reflect and respond to these views and the outcomes can be agreed with the child/young person and parent/carer. It is often when these views are not used or are ignored that further issues arise and a confrontational relationship may develop. SECTION G – Describe what you think the child’s life is like from their perspective To be added SECTION H – Analysis In this section you need to write what the conclusions of this initial process are; areas of risk, strengths, needs that can be met universally, additional needs that require specific support. This is a specialist model and should only be completed if you feel confident to do so. Using the grid outline; Family Strengths – Positive resources within the family Resiliency factors - support networks and family skills Dangers/Risks – What those undertaking the assessment process may be worried about Safety – things that keep the child and family safe SECTION I – What Needs to Change? Summarise the outcomes, solutions and goals that all are agreed to want to achieve. If there is a difference of opinion about what needs to change, make it clear who is seeking what. This information should inform the DAF 2 ‘My Plan’ at the Team Around the Child (TAC) meeting. It is an aim of this process that outcomes which can be agreed at this point give some immediate support to the child, young person and family and should be actioned without waiting for the outcome of a TAC meeting. NEXT STEPS MASH Enquiry The Multi-Agency Safeguarding Hub (MASH) is the central resource for receiving all safeguarding and child protection enquiries. The MASH is staffed with professionals from a range of agencies including police, probation, health, education and social care. These professionals share information to ensure early identification of potential significant harm, and trigger interventions to prevent further harm. MASH staff decide the most appropriate intervention to respond to the child’s identified needs. Where appropriate, the MASH team is able to immediately trigger a response. You do not need the consent or agreement of the parent/carer in order to make a MASH enquiry. DAF Guidance – DRAFT Version 6 – 13/02/2014 30 | P a g e MASH Enquiries: Tel: 0345 155 1071 E-mail: mashsecure@devon.gcsx.gov.uk Fax: 01392 448951 Proceed to DAF 2a ‘My Plan’ Following the DAF 1 assessment, a Team Around the Child (TAC) meeting should be arranged with the parent carers, child/young person and all relevant professionals. Use the DAF 2a to create a plan for the child/young person which is outcome focused. If you have any difficulty in getting an agency to engage in the TAC meeting, contact the Single Point of Access (SPA) for advice. If a child/young person has complex needs and there is sufficient evidence that the actions or interventions to date have not been successful in helping the child/young person achieve agreed outcomes, a request for additional resources can be submitted to the Single Point of Access (SPA). For more information on completing the DAF 3 ‘Request for Additional Resources’, please see page 34. No further action at this time If no further action is required at this time, please finalise the DAF paperwork with the agreement of the parent/carer or child/young person and ensure it is logged/kept in a place where it can be recovered in the future. Referral for Family Group Conferencing A Family Group Conference (FGC) is strengths based, family led, decision making process. The main difference with this way of working is that the family are the primary decision making group. The role of the ‘professionals’ is to share information about their role in supporting the family and potential resources that could be available; this might include extended family, neighbours and friends. The family have an agenda, set by the referrer, and after hearing information from the service providers, are left alone to make their plan. This process is set up and facilitated by a fully trained Independent Co-ordinator; children can be involved with support from advocates when required. This service is available free to all, wherever a plan needs to be made for a child. If you would like to know more please email fgcmailbox@devon.gov.uk Other Please note down any other action not present in the list above and explain the reason for this. Please ensure you note the name of the person completing the assessment and the date. If applicable complete the name and role of the agreed Lead Professional and the next review date (this may not be completed until the TAC meeting) DAF Guidance – DRAFT Version 6 – 13/02/2014 31 | P a g e 7. DAF 2a – ‘MY PLAN’ Once the DAF 1 has been completed and additional needs have been identified, the DAF 2a ‘My Plan’ should be used to identify the provision needed to achieve the agreed outcomes to meet the needs of the child/young person. In most cases the resources already available in the community, including the school setting will be able to support the plan. Health support at this level would include those health services identified as part of the community provision including initial Speech and Language support, uni-professional Occupational Therapy, Physiotherapy, Primary Mental Health Worker Support, School Nursing and ongoing Health Visitor support. My interests, views and aspirations (Pg. 1) If the child/young person has used a person centred planning tool e.g. Listen to Me and My Family, please ensure this is summarised in this section. If a child/young person is not able to complete this themselves, ensure you write this section using the exact words of the child/young person. My parent/carer’s views and aspirations for me (Pg. 1) If the parent carer(s) have used a person centred planning tool e.g. Listen to Me and My Family, please ensure this is summarised in this section or ask them to state there views at the TAC meeting. Page 2 This page summarises the details of the lead professional and should give enough information in order for the family to be able to contact them when necessary. The child/young person, parent/carer and lead professional should sign this page to show they agree with what is written in the plan. If the child/young person is unable to sign, please indicate how the Plan has been explained to them. SECTION 1 – Child/Young Person’s Health, Learning and Development Needs (Pg. 3) Area of Need Indicate whether this falls within a particular area e.g. Education, Health or Social Care. This will be the agency that is responsible for addressing that particular need and for funding any resources required to do this – usually Education, Health or Social Care. Only that agency can determine the needs and outcome that they are responsible for. DAF Guidance – DRAFT Version 6 – 13/02/2014 32 | P a g e Summary of Need The ‘need’ of the child or young person is the difficulty they experience that you are seeking to address. It is not what they need to be provided in order to address that difficulty. Desired Outcome Consider this by asking the question: ‘What do I want this child or young person to be able to do following this particular intervention?’ The outcome must be SMART (specific, measurable, achievable, realistic and time-bound) e.g. ‘access playtime three times out of a possible five every week by the end of Spring Term 2014’. This gives an easily measurable target that can feed into the overall outcome that you are working towards. The ‘outcome’ can be described as the end purpose for what you are working towards. Ask yourself the question, ‘what difference will this make for the child or young person?’ The answer to this will depend on what you have identified in the ‘summary of need’ column and they should link up, e.g. Area of need Summary of Need Desired Outcome Education P has little confidence and struggles to work independently Complete short tasks independently 2x per day (to develop confidence in independent work tasks). What will be done to achieve this? Following Teacher input, structure P’s class based learning into small, structured tasks that are within his capability and can be completed within his attention span. Who will do this and how often TA for6 weeks until 15th Oct Resources Needed / Cost Differentiated materials that are visually organised. Initial adult input to direct P to task and prompt a start. Progress towards achieving this outcome (Review) P has been successful at this and is now able to complete some class based tasks. This has resulted in P becoming more confident and attempting to do more than was expected. As a result of the work done on the ‘desired outcome’ the outcome for the child is that he can actually do something he couldn’t do previously and this has resulted in his confidence building to enable him to progress further. What will be done to achieve this outcome? (Provision) Describe the interventions that will be put in place to achieve the desired outcome Who will do this and how often? Indicate who is responsible for ensuring the outcome is achieved and how often they will need to provide the interventions described. Resources needed / Cost Resources should relate to anything provided and not purely related to staff time or money. DAF Guidance – DRAFT Version 6 – 13/02/2014 33 | P a g e When costing provision only things that are ‘additional to’ and ‘different from’ what would normally be provided should be included. To decide what is ‘additional to’ and ‘different from’ ask the questions; Would this resource be available whether or not this child or young person was here? Is this resource available for others at the same time as for this child or young person (e.g. group delivery by one TA to a number of pupils)? If the answer is ‘yes’ to these questions, then consider whether it is ‘additional to’ and ‘different from’ what is available anyway. SENCO time should not be costed, as this will be included in the SEN notional budget that is already within the school. Progress towards achieving this outcome At review, use this column to note down the progress made by the child/young person against each desired outcome. See ‘Desired Outcome’ guidance above. SECTION 2 - Parenting Of The Child/Young Person (Including Carers’ Needs (Pg. 4) The development table on Page 29 can be used to help describe the areas of need for this section. This could be completed at whatever level you are working at or the decision to seek additional input from appropriate professionals may be agreed at the TAC. If a social worker is undertaking a social work assessment, more focussed analysis will be undertaken in certain family circumstances and the columns on the left can be used to identify sub headings from the national framework for assessment. SECTION 3 - Family Environmental Factors (Child/Young Person’s Home And Community) (Pg. 5) The development table on Page 30 can be used to help describe the areas of need for this section. This could be completed at whatever level you are working at or the decision to seek additional input from appropriate professionals may be agreed at the TAC. If you are a social worker or housing officer undertaking a social work assessment or housing assessment a more focussed analysis will be undertaken in certain family/ individual circumstances and the columns on the left can be used to identify sub headings from the national framework for assessment. My Resources You should only cost the resources that your service has agreed to fund and is responsible for providing. Each service is responsible for completing their own section. You cannot cost provision made by another service without their agreement. If you are seeking additional resources from your service your request may be turned down if this section has not been completed. 8. DAF 2b – MY EDUCATION, HEALTH AND CARE (EHC) PLAN If a child or young person fails to make sufficient progress in their mainstream school, even with additional support, the local authority will then consider if an EHC assessment is necessary. Any DAF Guidance – DRAFT Version 6 – 13/02/2014 34 | P a g e professional working with a child, young person or family can make a referral for an EHC assessment as part of the Devon Assessment Framework (DAF) process. This is the process by which early help, support and intervention can be agreed from all of the relevant services. However, the range of support that has been provided over time, previous to requesting an EHC assessment will need to be demonstrated. A parent can also request an EHC assessment themselves but, if a child or young person is at school, we recommend that they speak to a teacher or the Special Educational Needs Co-ordinator (SENCo) first. This might lead to the start of a ‘My Plan’, which will set out the areas of need a child or young person has and will target support towards meeting the agreed outcomes. Once a ‘My Plan’ has been agreed and is in place it will be monitored to ensure progress is being made. At this stage, if the child or young person is making progress the ‘My Plan’ will be updated regularly. If the child or young person continues to have significant difficulties, the school's Special Educational Needs Co-ordinator (SENCO) will be able to make a request for additional ‘top-up’ funding or resource using the DAF 3 ‘Request for Additional Resources’. Other professional may also use the DAF 3 to request additional resources from their service. The Local Authority is unlikely to agree to an EHCP assessment at this stage as these only apply to those children with the most complex needs in a mainstream school or those who require a specialist school or setting. My interests, views and aspirations (Pg. 1) If the child/young person has used a person centred planning tool e.g. Listen to Me and My Family, please ensure this is summarised in this section. If a child/young person is not able to complete this themselves, ensure you write this section using the exact words of the child/young person. My parent/carer’s views and aspirations for me (Pg. 1) If the parent carer(s) have used a person centred planning tool e.g. Listen to Me and My Family, please ensure this is summarised in this section. My Current Needs (Pg. 2) Please note down all of the child/young persons’ special educational needs and any health and social care needs that have been identified through the assessment and planning process. Child/Young Person’s Health, Learning and Development (Pg. 3) For this section please see guidance for completing DAF 2a on pages 33-35. My Resources You should only cost the resources that your service has agreed to fund and is responsible for providing. Each service is responsible for completing their own section. You cannot cost provision made by another service without their agreement. If you are seeking additional resources from your service your request may be turned down if this section has not been completed. DAF Guidance – DRAFT Version 6 – 13/02/2014 35 | P a g e Placement This is the name of the school or setting that the child or young person is expected to attend. Where it has not been possible to name a school or setting, the type of setting they might attend is described instead. Advice and information use to inform this plan This is a list of all the advice and information that was used in completing this plan. 9.DAF 3 – ‘REQUEST FOR ADDITIONAL RESOURCES’ A request for additional support will only be considered when it can be clearly shown that all the resources available to a child or young person have been exhausted and they are still failing to make adequate progress. There will need to be evidence that a range of interventions over time have been explored. The request should be submitted to the Single Point of Access (SPA) along with all the relevant supporting documents and reports detailing the needs of the child or young person. Each service seeking additional resources will need to describe and cost the provision they are currently putting in place and clearly explain how any additional resource is expected to meet the outcomes identified on the current Plan. The request may be turned down if a fully costed Plan is not submitted. 10.DAF 4 TRANSITION ASSESSMENT 10.1.Overview In accordance with the Education Act 1996, amended in the Learning and Skills Act 2000 and amended by the Apprenticeships, Children and Learning Act 2009, Learning Difficulty Assessments are undertaken by the Local Authority for all young people who have had a Statement of Educational Needs for their pre-16 education. In 2013/14 all young people who have a Statement will have an DAF4/LDA in Year 11 to ensure that appropriate support can be put in place for them when they come to access their post-16 education. This will apply to young people who transition into provision whether in a school sixth form (post-16 in a special school), a Further Education College or independent specialist college. In Devon, Careers South West (CSW) is the organisation commissioned to undertake the DAF4/LDAs on behalf of Devon County Council. The information gathered in the DAF4/LDA will explain the learning difficulties and/or physical difficulties that the individual young person has and how they impact on their learning. They will also describe what support the young person will need to access their education. It could include information from any of the following documents: - Transition Plans - Individual Education Plan - Careers South West Plan - DAF1, 2a or 2b - Assessment from a local education provider - Statement / EHC Plan - Last Annual Review DAF Guidance – DRAFT Version 6 – 13/02/2014 36 | P a g e - Person Centred Plan - Educational Psychologist Report - CAMHS Report - Other professionals involved with the young person The DAF4/LDA is used by education providers, together with their own assessments to determine the level of support and funding needed for that young person to access their education and whether they are able to provide such support. The DAF4/LDA will result in a written report and may be supported by other documents. Devon County Council follow national guidance from the Education Funding Agency in placing young people with learning difficulties and/or disabilities. The following criteria need to be taken into account: - whether local provision by a mainstream provider (such as the local FE College) can adequately meet the learner’s needs - the learner has medical/care needs that mainstream provision cannot address which would otherwise prevent them from accessing education and support cannot be put in place to enable access - independent specialist provision meets the young person’s educational and medical/care needs and is essential to allowing them to participate in education or training to achieve their target outcomes - if applicable; a residential placement is necessary to meet an essential element of their education Where local providers cannot meet the educational needs for a young person with learning difficulties and/or disabilities, alternate provision will be sort. In order to agree the funding for such placements a Post-16 Placement Panel will make a decision based on the information contained in the DAF4/LDA together with other supporting documentation and an assessment from the local mainstream provider, where the young person’s needs can be met. In some instances such placements will require joint funding between Education and Adult Social Care/Health. We have the power to undertake DAF4/LDAs for young people who are not statemented but this will only be undertaken if a recommendation from a Careers SW advisor is agreed by the SEN 0-25 Team or is specifically requested by the SEN 0-25 Team. This is intended to be used in exceptional circumstances. 10.2.Completing The DAF 4 Parent Partnership Service can be signposted to give parents the opportunity to talk through this process independently. Parents/Carers must be involved with the process if the young person is under 16 and can be as involved with the assessment process post 16; again the Adviser needs to use professional judgement. In the case of applying for specialist/independent provision it is highly recommended that the parent/carer is kept fully informed. Personal Details and Agreement to Share Information (Pg. 1) This first page should capture the basic information of the young person and their consent to share the assessment with the appropriate education providers/trainers. DAF Guidance – DRAFT Version 6 – 13/02/2014 37 | P a g e Date of Birth / Age Please ensure that both of these fields are completed Child in Care (CiC) and Child in Need(CiN) Please ensure both of these questions are answered. This also applies to those who have left care as the local authority retains a duty until age 25 Agreement to Share Transition Information The signature of the young person (and parent/carer if appropriate) should be obtained when explaining the purpose of the DAF4/LDA. A parent/carer signature is required for any young person under the age of 16. An advisor should use their professional judgement when considering whether a parent/carer’s signature is required for those aged over 16, if in doubt get both signatures. If DAF4/LDA is being updated post 16 then the young person’s signature should be obtained at that time Consent is essential to share the information. A hard copy of this signed page must be sent to the LA and electronic copies of the DAF4/LDA are required to be attached to Insight. SECTION 1- Options Appraisal (Pg. 2) Options considered Local provision needs to be considered for all assessments whether it is the preferred choice or otherwise. It is recommended that local provision is applied for even it is not the preferred option and advice should be given to the young person and their family as such. In order to secure a place at a further education institution, a young person or their carer must apply for a place. Decisions on whether or not to offer a place are made by providers in response to an application. Post 16 education is not compulsory and it is for the young person and/or to make such an application Learner Preference Learner preference can be stated but there is no guarantee that specialist/independent provision will be funded. The LA will assess these through a Placement Panel Process. Please stress the need to apply for a local College as well Team leader must be entered – DAF4/LDA will be regarded as incomplete without this SECTION 2 – Terms of the Mental Capacity Act 2005 (Pg. 2) Additional information on Mental Capacity Act (pending). This question only applies to those aged 16 or over at the time of the assessment and only relates to the decisions being made in the DAF4/LDA process and not other decisions. A young person has the right to make the wrong decision; this does not mean they’re not capable of making any decisions If NO is ticked then a best interest meeting needs to follow. (See Mental Capacity Act information) DAF Guidance – DRAFT Version 6 – 13/02/2014 38 | P a g e If in doubt then please discuss with LA SECTION 3 – Other related documents required (Pg. 2) If the DAF4 is sent as a hard copy to the LA, please ensure any documents referenced here are sent as well. SECTION 4 – Learning Needs (Pg. 3) Describe Cognitive and Learning Needs Please ensure that the primary need is highlighted if there are multiple learning needs. Do not repeat the EHC plan or existing Statement of Special Educational Needs, this may be out of date from present needs and abilities. Is mainstream FE or School Sixth form the preference of the learner? If the young person is intending to enter a mainstream post 16 provider then the DAF4/LDA sections to be completed are sections 5, 9 and 12 as a minimum; Advisor may complete other sections if they feel the information is relevant. Are there transport needs that mean the local FE/SSF is not a preferred option? If a young person is looking to attend a SSF or FE College that is not their designated provider (see DCC Post 16 Transport Policy for details) then Section 10 needs to be completed to detail transport requirements SECTION 5 – Context of Learning (Pg. 4) Describe the educational needs and support requirements identified. This should not refer to a particular provider and should not show disproportionate influence of any one provider assessment. 24hour curriculum is not a support need Refer to resources, environments, support staff, levels of support (time, 1-2-1 and so on) Any equipment can be detailed in Section 8 SECTION 6 – Health and Social Care Needs (Pg. 5) Continuing Health Care in Adult Services is only applicable to those beyond or approaching their 18 th birthday SECTION 7 – Other Agencies and Services (Pg. 5) DfE guidance states that assessments must, where appropriate, consider the wider needs of young people and requires LAs to embed multi agency working in the assessment. This means that assessments from other professionals in health and social care can be referenced. If these documents support a named provider, this will be challenged by the LA; a recommendation could only be considered within the placement process if that professional had seen all possible options for provision. DAF Guidance – DRAFT Version 6 – 13/02/2014 39 | P a g e Contact the LA for an overview of Young Person in Transition meetings to determine if the young person has been discussed – relevant to those approaching 18th birthday. Any supporting documents from DCC staff that make an assessment should be independent of any provider locally or nationally unless there is a budget commitment included. SECTION 8 – Equipment (Pg. 6) Be as detailed as possible in terms of equipment and state if there is anything transferring with the young person. Do not assume that all equipment used in the past is a necessary requirement for further placements. SECTION 9 – Plans / Aspirations for the Future (Pg. 7) DfE guidance states that assessments must take account of the young person’s views and wishes and have a person centred approach focusing on progression. Expectations need to be managed if this is articulated in terms of a particular provider. The LA have to make a decision on specialist placements based on criteria not on preference and aspiration. While young people may have a preference to study on a particular course that does not mean that educational needs can only be met on this course. While young people have a right to express a preference, and preference must be taken into account, the LA must also take into account the fact that it has limited resources and must use those resources it has efficiently and fairly to meet the needs of all young people within its area. Advisors need to make young person and family aware of all post 16 provision and future employment and that they should have a contingency plan should funding not be approved for a particular preference Advisors should encourage plans and aspirations to consider future employment options and what is required to enable a young person to reach that goal SECTION 10 – Mobility, Travel and Transport (Pg. 8) DfE guidance requires that consideration of travel and transport needs including any recommendation for independent travel training as an aid to independence There is no automatic entitlement to post 16 transport and Advisors should signpost to the LA transport policy If applying for Further Education or School Sixth Form that is not the designated provider, the DAF4/LDA must be sent to the LA before the end of February if there are additional transport needs that outline why is more appropriate and a requirement to attend the non designated provider. Personal choice is not a need that requires transport to another provider SECTION 11 – Personal Skills, Social Skills and Aspirations The assessment needs to consider the wider context within which decisions are being made. Consideration should be given here to those needs beyond education and training; this section can inform other agencies when looking at packages of support that could complement local provision SECTION 12 – Future Placement This allows a summary to be made – no particular provider should be recommended by CSW; the LA will make the final decision if a specialist provider is applied for DAF Guidance – DRAFT Version 6 – 13/02/2014 40 | P a g e Final Checks - Assessment should be signed by Personal Advisor and Senior Manager (hard copy). DAF4/LDAs are not accepted without this. - A copy should be sent to the young person and their family if requested. If a copy has not been sent please record on page 10 of the DAF4/LDA. - Senior Manager should confirm that consent has been given and what date the hard copy was sent - Advice should be given to apply for local provision even if not the first preference - Electronic copy of the completed form should be attached to CCIS - If applying for independent specialist provision hard copies of DAF4/LDA and supporting documents should be sent to LA by agreed deadlines DAF Guidance – DRAFT Version 6 – 13/02/2014 41 | P a g e Deadlines 2013/14 Learner destination Independent Specialist Providers 16-25 Devon Special Schools 16-19 Devon Mainstream Post 16 16-19 SSF 16-25 FE Deadlines List of Names 5th Nov for list of names DAF4/LDA 31st Dec before Sep start List of Names 31st Jan for list of names DAF4/LDA 30th Mar before Sep start DAF4/LDA 31st May before Sep start (at latest) 28th Feb (exceptional cases) DAF Guidance – DRAFT Version 6 – 13/02/2014 Documents required DAF4/LDA (hard copy - SIGNED) (including assessment of options) Application to ISP Provider Assessments Supporting documentation as required DAF4/LDA (hard copy - SIGNED) (including assessment of options) Special School Assessments and proposed post 16 Programme of Study Learner details and nominated provider to DCC DAF4/LDA to nominated provider SIGNED DAF4/LDA must be sent to the LA if there are transport needs and the learner is applying for a non designated SSF/FE 42 | P a g e