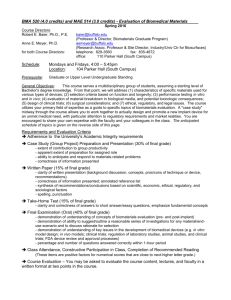
Biomaterials Science, 2nd edition
advertisement

Biomaterials Science, 2nd edition Part II: Biology, Biochemistry, and Medicine Questions Chapter 3: Some Background Concepts 3.1 Introduction Buddy D. Ratner 3.2 The Role of Adsorbed Proteins in Tissue Response to Biomaterials Thomas A. Horbett none 3.3 Cells and Cell Injury Richard N. Mitchell, Frederick J. Schoen none 3.4 Tissues: The Extracellular Matrix and Cell-Biomaterial Interactions Frederick J. Schoenm Richard N. Mitchell none 3.5 Mechanical Forces on Cells Larry V. McIntire, Suzanne G. Eskin, Andrew Yee none Chapter 4: Host Reactions to Biomaterials and Their Evaluation 4.1 Introduction Frederick J. Schoen 4.2 Inflammation, Wound Healing, and the Foreign Body Response James M. Anderson none 4.3 Innate and Adaptive Immunity: The Immune Response to Foreign Materials Richard N. Mitchell none 4.4 The Complement System Richard J. Johnson 1. A biomaterial is known to activate WBC and result in elevated levels of C5a when incubated with plasma. What markers or assays would you use to distinguish between classical and alternative pathway activation for this biomaterial. 2. In clinical hemodialysis the use of cellulosic membranes such as cellulose acetate are known to produce a more profound WBC activation (eg. neutoropenia) than synthetic membranes such as polysulfone. Explain why this so and how you modify the CA membrane to make it perform more like a synthetic. 3. Bacterial colonization of biomaterials is an important clinical complication, often necessitating removal of the biomaterial/device. Bacteria have evolved a number of mechanisms to protect them from complement attack, including the binding of complement regulatory proteins to their surface. Name two complement regulatory proteins that bacteria might use to inhibit complement. 4. Alexion Pharmaceuticals has developed a monoclonal antibody (eculizimab) that inhibits C5. They have shown in human clinical trials that treating patients with eculizimab results in lower IL6 levels in these patients. How does the antibody lower IL-6 levels. 4.5 Systemic Toxicity and Hypersensitivity Arne Hensten-Pettersen, Nils Jacobsen none 4.6 Blood Coagulation and Blood-Materials Interactions Stephen R. Hanson none 4.7 Tumorigenesis and Biomaterials Frederick J. Schoen none 4.8 Biofilms, Biomaterials, and Device-Related Infections Bill Costerton, Guy Cook, Mark Shirtliff, Paul Stoodley, Mark Pasmore none Chapter 5: Biological Testing of Biomaterials 5.1 Introduction to Testing Biomaterials Buddy D. Ratner 5.2 In Vitro Assessment of Tissue Compatibility Sharon J. Northup none 5.3 In Vivo Assessment of Tissue Compatibility James M. Anderson, Frederick J. Schoen none 5.4 Evaluation of Blood-Materials Interactions Stephen R. Hanson, Buddy D. Ratner none 5.5 Large Animal Models in Cardiac and Vascular Biomaterials Research and Testing Richard W. Bianco, John F. Grehan, Brian C. Grubbs, John P. Mrachek, Erik L. Schroeder, Clark W. Schumacher, Charles A. Svendsen, Matt Lahti 1. A large amount of progress in medical research leading to significant advances in health care has been made using mammalian models in biomedical research. In order to protect animal subjects the Animal Welfare Act was enacted which covers all of the following species except: A) B) C) D) E) Canine Feline Ovine Porcine Rattus 2. The comparative anatomy of dogs, swine, and sheep make them each advantageous for testing types biomaterials. Choose an animal model for testing 1) a synthetic coronary artery bypass graft, 2) a new pacemaker, and 3) a new tri-leaflet mechanical valve. Describe what features of the animal model make it desirable for testing the specific device. 3. The International Standards Organization mandates that in vivo testing of heart valves is completed to evaluate the performance of cardiac devices in a uniform manner. The rationale for in vivo pre-clincal testing is that valuable data on hemodynamic function, biological compatibility, and catastrophic failure can be obtained. After the testing is completed an official report is completed. Describe what should be documented in the report at the conclusion of the in vivo investigation. 5.6 Microscopy for Biomaterials Science Kip D. Hauch none Chapter 6: Degradation of Materials in the Biological Environment 6.1 Introduction: Degradation of Materials in the Biological Environment Buddy D. Ratner 6.2 Chemical and Biochemical Degradation of Polymers Arthur J. Coury 1. The two major mechanisms of chemical degradation of polymers in vivo are hydrolysis and oxidation. Given the following polymers, indicate whether they are susceptible to hydrolysis, oxidation or both processes. If they would be highly resistant to both processes, so indicate. Poly (carbonate urethane) Poly (ether urethane) Poly (ester urethane) Aromatic polyester, poly (ethylene terephthalate) Polypropylene Polyethylene (linear) Polytetrafluoroethylene Polydimethylsiloxane 2. What are some common polymer functional groups susceptible to hydrolysis? 3. In the past, investigators have fabricated heart valves from “aromatic polyurethanes” which contain polyether, urethane, and urea functional groups. These devices were intended to last for several years in use, but have generally failed to perform for those periods. What physical and chemical forces are acting on the heart valves in vivo? What are the most likely mechanisms (physical and chemical) of degradation leading to failure of these devices? State at least three mechanisms. 4. As a materials scientist, you have experience with polyurethanes as biomaterials. Among the readily available commercial elastomers, they demonstrate the best combination of physical properties, but are susceptible to biodegradation, mostly through their polyether or polyester soft segments. You are charged with designing a biostable elastomer (polyurethane or otherwise). Choose an approach to produce a chemically stable elastomer that retains reasonable physical properties for at least 3 years. Describe 5 tests/analyses (in vitro /in vivo) which may be used to characterize this elastomer and confirm its potential stability. 6.3 Degradative Effects of the Biological Environment on Metals and Ceramics David F. Williams, Rachel L. Williams 1. (a) What are the three most common implant alloys used in structural applications? For each one, state which element in the alloy is chosen to enhance corrosion resistance, and how do they do it? (b) Describe the mechanisms of intergranular corrosion and fretting corrosion. (c) If you had an orthodontic appliance where Ni-Ti wire was placed in the groove of a stainless steel bracket, what corrosion problems might you encounter? 2. Consider a situation in which a 316L stainless steel fracture fixation plate has been used to treat a tibial fracture. Discuss the possible mechanisms of corrosion of the device with reference to the alloy composition, the geometry of the device and the mechanical environment. Include a discussion on the fate of any corrosion products and their possible effect on the patient. 3. Discuss the potential disadvantages of using two different alloys for the components of modular orthopedic prostheses. 6.4 Pathologic Calcification of Biomaterials Frederick J. Schoen, Robert J. Levy none Chapter 7: Application of Materials in Medicine, Biology, and Artificial Organs 7.1 Introduction Jack E. Lemons, Frederick J. Schoen 7.2 Nonthrombogenic Treatments and Strategies Michael V. Sefton, Cynthia H. Gemmell none 7.3 Cardiovascular Medical Devices Robert F. Padera, Jr., Frederick J. Schoen none 7.4 Implantable Cardiac Assist Devices William R. Wagner, Harvey S. Borovetz, Bartley P. Griffith none 7.5 Artificial Red Blood Cell Substitutes Thomas M.S. Chang none 7.6 Extracorporeal Artificial Organs Paul S. Malchesky none 7.7 Orthopedic Applications Nadim J. Hallab, Joshua J. Jacobs, J. Lawrence Katz 1. What are the general qualifications for orthopedic biomaterials and what are the two major types of orthopedic implants? ANS: Generally orthopedic implants must be capable of load bearing and are used in either in bone fixation or total joint arthroplasty. 2. (a) What is the primary problem associated with the longevity of current total joint replacement implants and why? (b) How could this be solved by improved biomaterials? ANS: (a) Particle and wear debris generation at the articulating surfaces of total joint replacements causes aseptic loosening of the implants through the induction of inflammation around the implant (macrophageparticle overload) which causes a decreased production of new bone and increased bone resorption. (b) More wear-resistant materials at the articulating surface while maintaining current available levels of other mechanical properties. 3. What are the primary cytokines associated with particleinduced osteolysis, and what is the primary cell type involved in this process? ANS: The primary cytokines associated with osteolysis are TNF-alpha, IL-6 IL-1, prostaglandin E2, etc., produced by macrophage interaction with particulate debris from implants. 4. What are the seven primary orthopedic implant biomaterials? ANS: (a) Co-base alloys, Ti-base alloys, stainless steel, PMMA, UHMWPE, alumina, and zirconia. 5. Name one new orthopedic biomaterial and why it was introduced (i.e., what specific problem/deficit it is attempting to solve). ANS: Zirconium alloy was introduced to decrease the amount of metallic wear debris being generated at the bearing surface and as an alternative metal less likely to induce hypersensitivity reactions. 6. What is one way in which current designs of orthopedic implants are creating more challenging conditions for biomaterials to overcome and why? ANS: Increasing popularity and degree of orthopedic implant component modularity is creating more interfacial surfaces from which implant debris can be generated through fretting corrosion and interact both locally and systemically. 7.8 Dental Implantation A. Norman Cranin, Jack E. Lemons 1. What are the most popular metals in use today in dental implantology? 2. How well does bone tolerate invasive procedures? Is heat generated? Are there safe limits to induced temperatures? How can the health of host bone be assured? 3. What are some of the presurgical diagnostic techniques used to assist in planning? 4. Name some of the less frequently used dental implant modalities. 7.9 Adhesives and Sealants Dennis C. Smith none 7.10 Ophthalmological Applications Miguel F. Refojo none 7.11 Intraocular Lens Implant: A Scientific Perspective Anil S. Patel 1. What are the advantages of IOL implantation over spectacles for correction of vision after removal of cataract? What other improvements have been achieved in cataract surgery over the past 30 years? 2. Which was the first biomaterial selected for IOL implant? What was the basis for this selection? 3. What is the rationale for foldable IOLs? Which foldable soft hydrophobic materials are preferred over soft hydrophilic materials and why? 7.12 Burn Dressings and Skin Substitutes Jeffrey R. Morgan, Robert L. Sheridan, Ronald G. Tompkins, Martin L. Yarmush, John F. Burke none 7.13 Sutures Mark S. Roby, Jack Kennedy none 7.14 Drug Delivery Systems Jorge Heller, Allan Hoffman 1. You are working at AntiKoag, Inc., a company that has developed a new transdermal reservoir patch containing a rate-controlling membrane. The patch is to deliver an anti-coagulant drug whose plasma concentration needs to be carefully monitored due to its narrow therapeutic index. The FDA is coming next week to check on your quality control (e.g.,reproducibility of release rate profiles of the drug from the patch, both in vitro and in animals), and your boss has asked you to spend the weekend randomly sampling patches from batches that have been fabricated, packaged and stored over the past two months, and then measuring their in vitro release rates. You find there are two types of behavior, shown as A and B in the figure below. Release Rate A (%/hr) B Time (hrs) You know that all patches are supposed to have the same composition and structure, so how do you explain these two different behaviors to your boss? Can you suggest a way to produce a product with one consistent behavior, and if so, which behavior would you select, A or B? 2. A degradable copolymer of lactide and glycolide is being tested as a disc-shaped drug depot that has been implanted in sub-cutaneous sites in rats. Some implants have been retrieved after about two weeks, and are found to have a hollow core inside of a strong shell of polymer. Your colleague thinks the reason for this is simply that the drug has leaked out and left the empty core, but the drug only makes up 1% by weight of the sample, so you know he cannot be right. What other reason(s) could explain this phenomenon, and how might you avoid it? 3. You are working for a drug delivery company that has discovered a new anti-inflammatory bowel disease (IBC) drug to be delivered orally. You are fabricating an elementary osmotic pump capsule by encapsulating lyophilized particles of the drug in a cellulose acetate (CA) coating and drilling a tiny hole in the CA with a laser. Water permeates through the CA and creates a saturated drug solution inside the capsule, which is delivered out of the hole. Excess drug particles remain in suspension inside the capsule. Your boss wants the company to market a range of capsules with high, medium and low delivery rates for the new drug, since the severity of IBC varies from patient to patient. The transit time through the GI tract and the influence of food intake on it are assumed to be fixed, average values for all patients. Also assume that only one capsule having the desired dosage is to be taken by each patient, and that the laser drilled hole has a fixed diameter, which is designed to permit liquid flow out but to prevent drug particles from escaping from the tablet during its transit through the gut. How could you (a) increase or (b) decrease the amount of drug delivered during transit through the gut? 7.15 Bioelectrodes Ramakrishna Venugopalan, Ray Ideker 1. What material would you choose for a deep brain stimulating electrode and why? Develop a simplistic equivalent circuit model for such an electrode–electrolyte interface. You do not have to model the tissue. Model only the interface. 2. Calculate the increase in charge injected by decreasing the frequency of a symmetric sinusoidal waveform by an order of magnitude assuming all other parameters remain constant. 3. Compare and contrast the region of oxide stability (potential range) for titanium alloy and 316L stainless steel electrodes. Assume that the oxides on titanium electrode and stainless steel electrodes are predominantly TiO2 and Cr2O3, respectively. (Hint: Refer to the Pourbaix diagrams for titanium and chromium.) 4. Would a material used for a radio-frequency ablation electrode also be ideal for a cryoablation electrode (ablation due to freezing)? 5. Develop an equivalent circuit model for a capacitively coupled device used for healing nonunion fractures. You do not have to model the tissue. Model only the interface. 7.16 Cochlear Prostheses Francis A. Spelman 1. Sound at the level of the tympanic membrane demonstrates a pressure peak at a frequency of 2.5 kHz in the human. Consider the boundary conditions of the ear canal and explain why that resonance occurs. 2. Considering the areas of the stapes and the tympanic membrane, as well as the properties of the ossicular chain, compute the approximate ratio of pressures that is found when the tympanic membrane is driven at low frequency. Note that this is an approximate calculation that does not consider the dynamics of the system. 3. Focusing stimuli has been proposed by several people (Suesserman and Spelman, 1993; Jolly et al., 1996) as a solution to the problem of field interference between monopole sources. Consider using dipole and quadrupole sources. Assume that the sources are 50-µm hemispheres located on the surface of an insulating boundary. Let the hemispheres be separated by 200 µm in both cases. Plot the potential fields along two lines: one that is 100 µm above and parallel to the sources, another that is 200 µm above and parallel to the sources. Describe the properties of the fields that are produced. Look particularly at the peak potentials and the half-amplitude widths of the fields. Hints: A dipole consists of two sources, one carrying current I and the other carrying current –I. A quadrupole is a special case of a tripole. Three sources are used. The central source carries current I, while the two flanking sources carry current –I/2. For ease of calculation, place one of the sources at the origin, and let the other sources lie on, e.g., the x-axis. 4. Wiley and Webster (1982) give an equation that describes the potential field produced by an electrode of radius a located at the origin of a cylindrical coordinate system. The electrode is placed on the surface of an insulating boundary. V (r , z ) sin 1 r a 2 z 2 2V0 2a r a 0.5 2 0. 5 z 2 and J z (r ,0) 2V0 J0 1 2 0.5 2 (a r ) 2 1 r a 2 0. 5 where J0 I0 a 2 I0 is the total current flowing into the electrode, J0 is a current density (defined earlier), ρ is the resistivity of the medium, and r is the radial distance [x2 + y2]0.5. Place a point source at the origin and compare it to a circular, planar electrode with its center at the origin. Let the radius of the circular electrode be 100 µm. Compute the potential field for −1 mm≤ x ≤ 1 mm at altitudes of 50 and 750 µm. What can you say about the shapes and the peak potentials? 5. A cochlear electrode array employs contacts that are hemispheres 100 µmin diameter. As the designer of the array, you compare Pt–Ir contacts with IrOx contacts. In one stimulus mode, you will use sinusoids of 100 and 1000 Hz. What is the maximum current that you can tolerate for each material at each frequency? Hint: compute charge per phase of the sinusoid. 6. A measurement of the IrOx electrode produces an impedance magnitude of 5 kilohms at 1000 Hz. If you drive a dipole pair with a 1-kHz sinusoid, what voltage range must the current source have if you drive the maximum allowable current that the electrode can tolerate? Assume that the tissue impedance of the cochlea is small compared to the impedance of the electrodes. 7. Two electrode array designs are considered. One uses a silicone substrate and the other a liquid crystal polymer substrate. If a circular cross section is used, with an outside diameter of 200 µm, find the force that would be exerted on a free end whose length is 1 mm and whose deflection is 20 µm. The modulus of elasticity of silicone is 2.76 MPa and that of liquid crystal polymer is 158 MPa. The polar moment of inertia is Ip d 4 32 8. A simple model of electrode impedance is the Warburg model (Macdonald, 1987). This diffusion model can take the form of a parallel resistance/capacitance circuit in which the resistance and capacitance are both inversely proportional to the square root of frequency, i.e., R( f ) R0 C( f ) C0 f f Compute the magnitude and phase of the electrode’s impedance if its impedance is 1 megohm at 10 Hz. Compute for frequencies from 10 Hz to 10 kHz. Assume that the electrode is circular in shape, and that its diameter is 100 µm. If it is covered with a membrane whose specific capacitance is that given in the text, how does the character of the impedance change? Plot the magnitudes and phases for both situations. 9. If the time constant of the membrane that covers the electrode is 125 msec, recompute the impedance for problem 8, accounting for the membrane resistance that parallels the membrane capacitance. 10. Consider the uncoated electrode of problem 8. If a controlled sinusoidal current were applied to the electrode, what would be the peak-to-peak voltage necessary to drive the current, undistorted, over the full frequency range? Assume that the electrode is driven as a monopole and that its counterelectrode has negligible impedance. 7.17 Biomedical Sensors and Biosensors Paul Yager none 7.18 Diagnostics and Biomaterials Peter J. Tarcha, Thomas E. Rohr none 7.19 Medical Applications of Silicones Jim Curtis, André Colas 1. Which material property was the basis for Charles Holter's selection of silicone rubber for the hydrocephalic shunt valve? a. biostability b. hemocompatibility c. thermal stability d. viscoelasticity e. all of the above 2. Epidemiology has shown silicone breast implants cause which of the following complications? a. breast cancer b. connective tissue disease c. autoimmune disease d. all of the above e. none of the above 3. Among the following applications where silicones are still in use today, which was the first reported human implantation of a silicone elastomer medical device? a. breast augmentation b. bile duct repair c. hydrocephalus shunt d. urethra repair Chapter 8: Tissue Engineering 8.1 Introduction Frederick J. Schoen 8.2 Overview of Tissue Engineering Simon P. Hoerstrup, Joseph P. Vacanti none 8.3 Immunoisolation Michael J.Lysaght, David Rein none 8.4 Synthetic Bioresorbable Polymer Scaffolds Antonios G. Mikos, Lichun Lu, Johnna S. Temenoff, Joerg K. Tessmar none