Advice_for_Healthy_Travel
advertisement

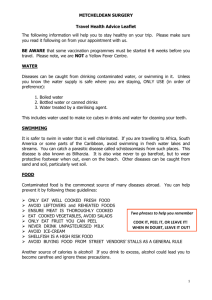
SWADLINCOTE SURGERY GUIDE TO HEALTHY TRAVEL Accident Prevention 5. 6. If a swimming pool smells of chlorine, the risk of infection is probably slight. Travellers to the tropics beware of water associated diseases eg. Schistosomiasis. Seek local advice on the presence of these diseases and water snakes. Jet Lag Road and swimming accidents are the most common cause of death and injury to travellers. Road Safety 1. Do not drink alcohol and drive. 2. Wear seat belts in cars. 3. Wear crash helmets when riding motor bikes and mopeds. Ensure your clothes help protect your arms and legs. 4. Check that rented vehicles are in good condition and are insured. 5. Find out about local traffic systems, regulations and road conditions. Usually only appreciable if crossing more than 5 time zones (five hours’ time difference). Worse if the flight is eastwards (ie. When the day of travel is shortened). 1. Do not book heavy commitments for the first 24 hours after travel. 2. Sleep on the plane. 3. Avoid or limit your alcohol intake. Drink plenty of soft drinks. 4. Keep regular medications on home time and meals during the flight, when practicable, and adjust on arrival. Diabetics need more detailed advice. Sun and Hot Climates Swimming Safety and Leisure Activities 1. Do not drink alcohol and swim. Wait at least an hour after eating before swimming. 2. Think before you jump. Make sure you know the depth of the water before diving. 3. Find out about local safe beaches and sea conditions. Beware of water currents and inflatable airbeds or dinghies. 4. Children need close supervision by water. 1. 2. Prevent damage to the skin in the first place by careful preparation. Initially limit exposure to the sun and increase gradually. Fair skins are most at risk. Use high factor sunscreens with frequent top ups especially after swimming. 3. 4. 5. Wear hats and T-shirts and other loosely fitting clothing. Encourage children and snorkellers to wear T-shirts over swim suits. Increased sweating means increased fluid loss, therefore increase fluid intake and add extra table salt to meals. Drink enough to keep your urine light coloured. If you get sunburnt: avoid the sun, have cool showers, drink plenty of fluids, and use calamine lotion. Painkillers such as paracetamol and anti-histamines may help. Do not burst any blisters as it encourages local infection. Blood Borne Diseases, Sexually Transmitted Diseases and AIDS Blood Borne Diseases Many countries do not have the standard of healthcare that you are used to in the UK. Medical and dental equipment may not be properly sterilised. Blood is not always screened for infections. 1. Make sure you are fit to travel. 2. If you have a medical problem, try to find out where you will receive a good standard of medical care at your destination. If you become ill abroad seek advice from the British Embassy or High Commission. 3. Any dental treatment should be completed before travel. 4. Ensure holiday insurance includes medical repatriation. 5. Reduce the risk of accidents abroad and attend a first aid course. 6. Know your blood group and find out if any fellow travellers have a compatible blood group. 7. If you do need a blood transfusion ensure it is absolutely necessary. Ask if alternatives such as plasma expanders can be used or the availability of screened blood. 8. The charity the Blood Care Foundation will provide screened blood for Emergencies worldwide. For information write to the Blood Care Foundation, PO Box 7, Sevenoaks, Kent TN13 2 SZ. Tel. 01732 742427. Sexually Transmitted Diseases and AIDS 1. Beware of casual sex. Do not take risks. 2. Always use a condom. Take adequate supplies of condoms, which have the British Standard Kitemark. 3. Alcohol encourages sexual risk taking. 4. If in doubt visit the local STD or genitourinary clinic on your return. Sterile Needles and Syringes 1. Medical kits are available containing sterile needles and syringes for emergency use. Carry it at all times and keep it in its original case so that it’s purpose is obvious. Travellers Diarrhoea 1. 2. Use only bottled water (preferably carbonated) or boiled water and ensure the seal is intact. This includes water used for brushing teeth, washing fruit and salads, and in ice cubes. Beware of locally produced drinks; ice cubes and ice cream. Water can also be purified by boiling for at least 10 minutes, or using water sterilising tablets, or using a water filter/purifier. Peel fruit, including tomatoes and avoid those that cannot be peeled. Eat only cooked vegetables and avoid salads. 3. Cook meat, seafood and fish thoroughly. Ensure food is served piping hot and avoid left overs and reheated food. 4. Boil unpasteurised milk. 5. Be wary of soft cheeses and other dairy products particularly if made with unpasteurised milk and when there is no refrigeration. 6. Wash your hands thoroughly with soap and clean water before eating and always after going to the toilet. Use paper towels or hot air for drying hands and whenever possible avoid touching food with your hands. What to do when diarrhoea strikes Most episodes of diarrhoea will pass in three to four days without treatment. 1. Assess the diarrhoea. Is it watery? Is there any blood or mucous present? 2. Check your fluid balance. Make a rough guess about whether you are losing more fluid through diarrhoea than you are drinking. 3. Drink plenty of fluids – enough to keep your tongue moist and your urine a pale yellow colour. Small amounts of dark urine suggest you are at risk of dehydration. (See “Travellers First Aid Kit” for oral rehydration mixture). 4. Seek medical attention if you develop a temperature above 38C, find blood in your stools, become dehydrated, or if the diarrhoea persists for one week. 5. Introduce food gradually. Avoid solid food for the first day or two. 6. Antidiarrhoeal tablets are recommended when the diarrhoea will be an inconvenience. They are not recommended for children. 7. Antibiotics are not routinely recommended. Remember: boil it, cook it, peel it. When in doubt, miss it out! Animal Bites, Scratches and Licks If you are going to a country where rabies is present, then all bites, scratches and even licks should be considered as suspect. Rabies is a virus infection carried by infected dogs, cats, foxes, bats and other animals. 1. Always consider the possibility of rabies if you are bitten, scratched or licked by an animal. 2. Clean the wound immediately and thoroughly with soap and running water for at least 5 minutes. Apply tincture of iodine or alcohol. 3. If the owner of the animal is present, find out if it has been vaccinated against rabies and ask to see the last certificate. Exchange each other’s details. 4. Make sure you seek local medical advice about rabies vaccination as soon as possible, even if the animal has been vaccinated or you have had the rabies vaccine. 5. Inform the local police in the country and then your GP on returning home. Prevention of Malaria Malaria is the most serious disease that a traveller faces in tropical climates and it can be fatal. It is transmitted by the bite of a mosquito; these are most active between dusk and dawn. Personal Protection 1. Avoid exposing areas of skin after sunset. Wear long sleeved tops and trousers. Light colours are less attractive to mosquitoes. 2. Use insect repellents. Skin preparations should contain DEET. Eucalyptus preparations are an alternative and more user friendly. Apply to all exposed areas, especially the wrists, ankles and feet. Wrist and ankle bands soaked in DEET are available and last for several weeks. Physical Protection 1. Always use a mosquito net treated with permethrin in malarial areas in rooms that do not have air-conditioning. Check the net for holes and tuck it firmly under the mattress. 2. Use accommodation that has screens on windows and doors and air conditioning that runs all night. Keep doors and windows tightly shut. 3. Mosquitoes that have entered a room can be killed with insecticide spray. 4. Mosquito coils that burn smouldering pyrethrum can be useful in preventing mosquito bites at night or use synthetic pyrethroid containing electric mats. Antimalarial Tablets Start your antimalarial tablets two to three weeks before you travel, so that any reactions can be reported to your doctor. Take them with a meal and regularly. It is important that you continue taking the tablets for four weeks after you have returned, to cover the incubation period. When To Suspect Malaria Some of the main signs and symptoms of malaria are a flu-like illness with fever, chills, sweating, and headache. Seek medical attention for any fever 1-week after arriving in malaria zone. On your return home, remember to suspect malaria if feverish symptoms begin, especially in the first three months following your return. The possibility of malaria persist for up to one year. Always inform your doctor that you have visited a malaria zone. Taking Children to Malarial Areas The advice for babies and children is the same as for adults. 1. Antimalarials should be started in babies from birth. Breast-feeding does not provide protection. Some antimalarials are available in syrup. 2. Insect repellents containing DEET should be used sparingly avoiding the mouth and eyes. 3. The onset of malaria can be very rapid in babies and children, therefore seek medical attention promptly if the signs or symptoms of malaria appear. The Travellers First Aid Kit Remember to take enough of your usual medication. These are some suggestions about what you should consider taking with you on holiday and can be used as a checklist. First aid dressings Gauze squares, non-adherent dressings, bandage, fabric plasters, adhesive tape, scissors, tweezers and safety pins. Antiseptic Wipes, dry powder or spray: Savlon, betadine, and tincture of iodine. Use for cuts and grazes. Calamine lotion Use for sunburn and/or skin irritation. Painkillers Use for temperatures, pain and inflammation. Painkillers continued Paracetamol or aspirin (aspirin should not be given to children under 12 yrs). Calpol or other infant formula for children or babies. Thermometer Oral rehydration therapy in sachets and different flavours. Use for fluid replacement in diarrhoea. Dioralyte and Rehidrat. See below for homemade mixture. Antifungal cream Miconazole cream/powder, clotrimazole cream/powder. Antihistamines Chlorpheniramine, astemizole. Promethazine (Phenergan) for children. Oil of cloves For toothache. Ephedrine nasal drops For children with blocked noses or catarrhal ears. Insect repellent Travel sickness remedy Promethazine, cinnarizine. Indigestion remedy Protective sun cream, sunblock and lip cream Personal medication A doctor’s letter should accompany a larger amount of personal medication, or syringes and needles. For Travel to less developed countries Antidiarrhoeals Not recommended for children. Arret, Diocalm Ultra, Imodium or Lomotil. Codeine phosphate needs a doctor’s letter explaining why it is necessary. Water sterilisation Sterile injection kit Antibiotics Water filter or sterilising tablets. Iodine is better than chlorine based tablets at killing amoebic cysts. Needles and syringes; may include cannula. The need for antibiotics should be discussed with your doctor. Possibly required Contraceptives or condoms Acetazolamide For altitude sickness. For travel to malarial areas Antimalarial tablets Insect repellent Containing DEET; This can be bought in various strengths: Autan, Jungle Juice, Expedition. Eucalyptus preparations such as Mosi-guard. Wrist and ankle bands Soaked in insect repellent. Mosquito net Soaked in insecticide: permethrin or icon. For those travelling rough. Stand-by malarial If travelling to remote areas more treatment than 24 hours from medical help. Home-made oral rehydration mixture for diarrhoea 1 litre of water 1 level teaspoonful of salt 4 heaped teaspoonfuls of sugar ) ) all mixed together ) Further Reading Health Advice for Travellers. Department of Health. T5 1995 Leaflet. Available free from post offices. It also contains an application form for the certificate E111. Stay Healthy Abroad: The essential guide for all travellers. Ryan R. Health Education Authority 1995. The Traveller’s Handbook. Gorman S. and Brandenburger C. (eds) Wexas 1994 Very comprehensive. The Tropical Traveller. Hatt J. Penguin 1993 (3rd edition). Tropical travel tips. First Aid Manual. St John Ambulance. St Andrew’s Association, British Red Cross Society. Dorling Kindersley 1987. National Suppliers of Medical Goods Homeway Medical Ltd The White House Littleton Winchester HantsSO22 6QS Tel: 01962 881526 Lifesystems 4 Mercury House Calleva Park Aldermaston Berks RG7 4QW Tel: 01734 811433 Industrial Pharmaceutical Service Ltd Bridgewater Road Broadheath Altrincham Cheshire WA14 1NA Tel: 0161 928 3672 Medical Advisory Service for Travellers Abroad (MASTA) Keppel Street London WC1E 7HT Tel: 0171 631 4408 Nomad (Pharmacy) Ltd 3-4 Turnpike Lane London N8 0PX Tel: 0181 889 7014 SAFA Limited 59 Hill Street Liverpool L8 5SA Tel: 0151 708 0397 Philip Harris Medical Ltd Hazelwell Lane Stirchley Birmingham B30 2 PS Tel: 0121 433 3030 Williams Medical Supplies Unit 6 Springhead Enterprise Park Springhead Road Northfleet Kent DA11 8HD Tel: 01474 535330