Guide to meningococcal infection - meningitis and the need for
advertisement
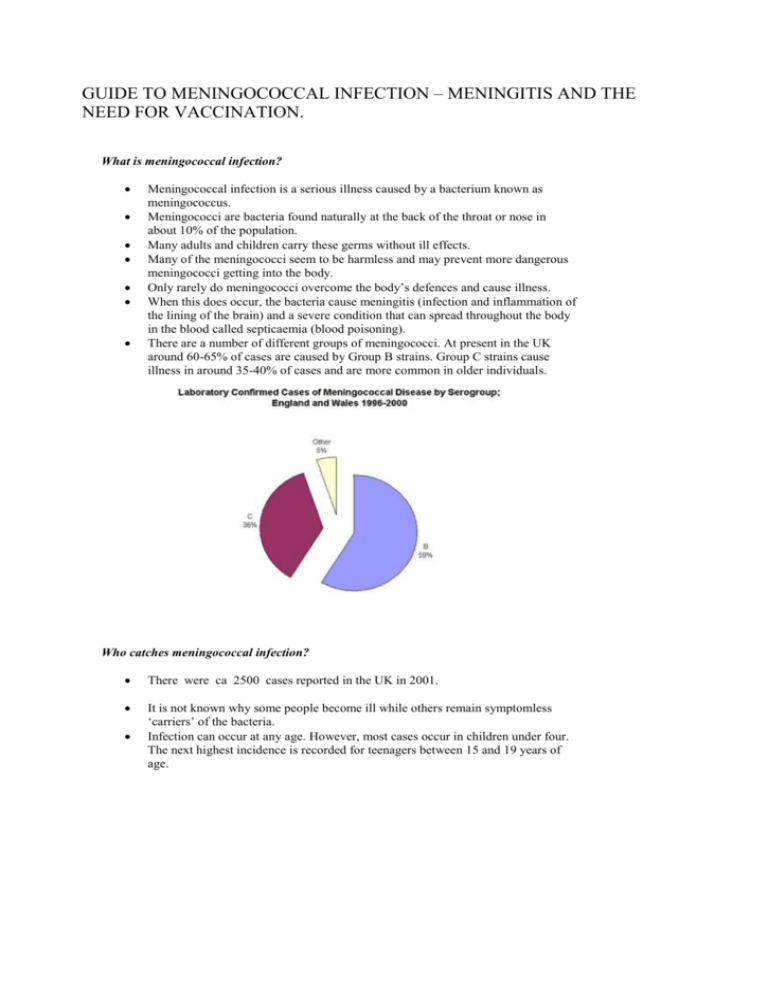
GUIDE TO MENINGOCOCCAL INFECTION – MENINGITIS AND THE NEED FOR VACCINATION. What is meningococcal infection? Meningococcal infection is a serious illness caused by a bacterium known as meningococcus. Meningococci are bacteria found naturally at the back of the throat or nose in about 10% of the population. Many adults and children carry these germs without ill effects. Many of the meningococci seem to be harmless and may prevent more dangerous meningococci getting into the body. Only rarely do meningococci overcome the body’s defences and cause illness. When this does occur, the bacteria cause meningitis (infection and inflammation of the lining of the brain) and a severe condition that can spread throughout the body in the blood called septicaemia (blood poisoning). There are a number of different groups of meningococci. At present in the UK around 60-65% of cases are caused by Group B strains. Group C strains cause illness in around 35-40% of cases and are more common in older individuals. Who catches meningococcal infection? There were ca 2500 cases reported in the UK in 2001. It is not known why some people become ill while others remain symptomless ‘carriers’ of the bacteria. Infection can occur at any age. However, most cases occur in children under four. The next highest incidence is recorded for teenagers between 15 and 19 years of age. Confirmed cases of meningococcal disease in England and Wales, Weeks 1 39 (PHLS data) 1400 1293 1241 1200 1085 Confirmed cases 1000 758 800 Group B 608 Group C 600 400 266 200 0 1999 2000 2001 Year (Meningitis C vaccination Introduced to under 18s in11999) Most cases occur without any connection to other cases (sporadic cases), sometimes two or more cases are connected by those affected having close contact (outbreaks). How can you suspect someone has meningococcal infection? Someone with the infection will become very ill, though not all the symptoms will occur at once. In children and young adults symptoms can include: sudden onset of a high fever a severe headache dislike of bright lights (photophobia) vomiting drowsiness that can deteriorate into a coma Septicaemia occurs if the bacteria enter the bloodstream. A characteristic rash develops and may start as a cluster of pinprick blood spots under the skin, spreading to form bruises under the skin. The rash can appear anywhere on the body. It can be distinguished from other rashes by the fact that it does not fade when pressed under the bottom of a glass (the tumbler test). Symptoms can develop within hours. How do you catch meningococcal infection? Meningococcal infection is not highly infectious. The bacteria are passed by close contact, so family members of a case and others who have close contacts with a case may be spreading the same germs. This usually means household or kissing contacts. Close contact in residential accommodation, such as student halls of residence can also give the opportunity for the spread of infection. As the bacteria cannot survive for long outside the human body, infection cannot be caught from water supplies, swimming pools, or buildings. How serious is meningococcal infection? The bacteria only rarely give rise to meningococcal disease. But when they do infection spreads rapidly and is fatal in about 10% of cases (up to 50% with septicaemia). If infection is diagnosed early and treated promptly most people make a full recovery. However, about 1 in 8 people who recover experience some long term effects. These can include headaches, stiffness in the joints, epileptic fits, deafness and learning difficulties. Can you prevent meningococcal infection? A vaccine against meningococci group C was introduced to under 18 year-olds in the UJ in 1999/2000. It gives good protection and has reduced by 90 % the cases of meningitis due to the Meningitis C strain in 15 – 17 year olds..It is now being offered to everyone under the age of 25. (see graph below) There is as yet no vaccination for the other common group of meningococci in the UK (group B). Antibiotics are recommended for close contacts of a case to prevent further spread of infection. If group C is involved, the vaccine may be given as well as antibiotics. Group C Meningococcal Disease: January to September by Age Group, England and Wales 180 155 1999 2000 2001 Confirmed Cases 160 140 120 96 100 80 86 73 73 83 68 76 68 61 57 60 40 20 46 37 26 17 41 22 21 7 4 8 0 Under 1 1-2 yrs 3-4 yrs 5-9 yrs 10-14 yrs 15-19 yrs 20-24 yrs Age Group Covered by Men vaccination since 1999. C How can you treat someone with meningococcal disease? Antibiotics are used to treat meningococcal disease The earlier the treatment, the better the prospect of recovery. Often GPs will give treatment even before the person is admitted to hospital. If you suspect someone may have meningococcal disease, contact the doctor immediately. If the doctor is unavailable they should be taken to the nearest casualty department. Prompt action is vital The Meningitis C Immunisation Programme The UK was the first country in the world to introduce meningococcal serogroup C PHLS conjugate (MenC) vaccination. Immunisation with (MenC) vaccine started in November 1999 for everybody up to the age of 18 years, and to all first year university students within two weeks of arriving at college. This has since been extended to include everybody under 25 years of age. For further information about Meningitis C vaccine see Department of Health http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuid ance/DH_082989 and Health Promotion England http://www.dh.gov.uk/en/Publichealth/Information/index.htm The MenC vaccine does not protect against other meningococcal disease caused by other serogroups (A, B, W135, Y). Three other European countries (Ireland, Spain and Luxembourg) have followed the UK in implementing conjugate meningococcal C vaccination programmes. Various other European Union countries or regions are currently considering the introduction of routine conjugate meningococcal C vaccination programmes. These include Belgium, Greece, Madeira, and the Netherlands. As the vaccine does not protect against serogroup B meningococcal disease (currently responsible for the majority of meningococcal infections), it is of the upmost importance that health professionals and the general public remain alert to the signs and symptoms of meningococcal disease. Work is currently being undertaken to develop a group B meningococcal vaccine. However, the variability of the group B meningococcus means that a group B vaccine for meningococcal disease will not be available for sometime. Meningococcal vaccines and travel: Polysaccharide vaccines for serogroups A and C have been available for some time and are used for travellers to parts of Africa and the Middle East. These vaccines are not effective in children under 2 years old and offer short term protection (3-5 years). If the person remains at risk of serogroup A meningococcal disease (e.g. travel to sub-Saharan Africa) a polysaccharide vaccine containing serogroup A will be recommended. An individual who has had the polysaccharide A and C vaccination can have the MenC vaccine after a specified period of time. A quadrivalent vaccine (ACWY Vax) protecting against disease caused by serogroups A, C, W135 and Y from GSK is available for travel to the religious festivals of Hajj and Umra. Travellers to these festivals must ensure their vaccination covers these four meningitis variants. Saudi authorities are requesting a certifcate of vaccination from visiting pilgrims. For more information see Department of Health http://www.nhs.uk/Livewell/travelhealth/Pages/Travelhealthhome.aspx .