Biomedical waste other than sharps and bulk liquids must be

E1739
V2
Proposal of Medical Waste Management Plan (MWMP)
For Rural Health Facilities in Four States
( Blue Nile , South Kordufan , Kasala and Red Sea )
Prepared For
Federal Ministry of Health (FMOH)
Decentralized Health System Development Project (DHSDP)
BY
Dr.Abd Alrahman Elamin
AUGUST 12, 2008
1
Proposed Medical Waste Management Plan
Table of Content Page number
Introduction .………………………………………………………………...………………..1
1.0 Medical waste management plan For Sudanese Rural Health facilities………….2
1.1 Current situation of water supply in the rural health facilities……………... ……2
1.2 Best practice of water sources…………………………………………….………2
1.3 Best Practice for sewerage (toilet) system ……………………………………….2
2.0 Medical waste minimization options …………………………………..……………………3
2.1 Source Reduction………………………………………………………………….. 3
3-0 Regulation and control system……………………………………………………………….3
4.0 Medical Waste collection………………………………………….…………………………..4
5.0
Handling and disposal facilities…………………………………………..…………………5
6.0 Medical waste Storage and packaging………………………………………………..7
7.0 Proposal of Appropriate Treatment/disposal methods of Medical waste
Applicable for Rural Health facilities in Sudan………………………….………………………..9
7.1 Disposal of Contaminated Waste…………………………………………………… 9
7.2 Best Practice for disposal of liquid contaminated .……………..…………….... 9
7.3 Best Practice for the disposal of solid contaminated wastes……………… .....10
7.4 INCINERATION………………………………………………….……………….………..11
7.4.1 Types of Incinerators ………………………………………………………………...11
7.4.2 Types of Waste That Should Not Be Incinerated……………………………..….11
2
7.4.3 How to Build and Use a Simple Drum Incinerator for Waste
Disposal……………………………………………..………………………12
7.5 Open burning ………………………… ………………………….…………….….. 14
7.6 Burying waste……………………………………………………….………….……..14
7.6.1 How to Make and Use a Small Burial Site for Waste Disposal……....14
7.7.0 Best Practice for disposal of Hazardous wastes…………………………..……...16
7.7.1 Chemical Waste ………………………………………………..………. 16
7.7.2 How to Dispose of Used Chemical Containers……………...………..16
7.7.3 Disposal of Large amounts of pharmaceutical waste ……….……..17
8.0 Mercury spill handling and management…………………………………..……..17
9.0 Personnel training procedures……………………………………………..…...…….19
3
Proposed Medical Waste Management Plan
Introduction
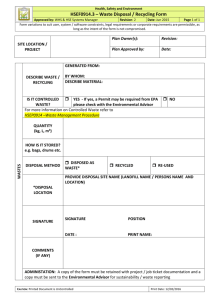
Medical waste management practices that should be employed include strictly segregating, packaging, labeling, and tracking the waste according to state requirements or WHO regulations; the most essential part of hospital waste management is the segregation of medical waste. The segregation of the waste should be performed within the premises of the hospital/nursing homes, according to the color coding as indicated in Annex I, the type of container to be used for different waste category and suggested treatment options are listed in Annex II.
Unfortunately all the above mentioned practices can not be applied for the biomedical waste management in the Sudanese rural health facilities due to the followings:
There is no reliable healthy source of potable water and water for cleaning or for sanitation.
There is no electricity for autoclave , incinerators or steam sterilization
Rural health facilities are remote areas some times there is no regular transport especially
during the rainy seasons.
Lack of awareness amongst the hospital staff including doctors, nurses..Etc. towards the management of Biomedical waste in the hospital
Therefore the proposed biomedical waste plan and waste treatment technique will be according to the international standards such as WHO, UN regulations by applying simple types of technologies or treatment that suit the rural areas in Sudan this policy should be in the short term, but for long terms they should apply the modern safe technique according to the international standards.
4
1.0 Medical waste management plan For Sudanese Rural Health facilities
This part of the study present the best practice that can be applied in Sudanese Rural health facilities with the local resources , appropriate technology with minimum cost, the proposed biomedical waste management plan consists of the followings:
1Water resource and sewerage system
2 Medical waste minimization options
3Regulation and control system
4Medical Waste collection
5Handling and disposal facilities
6Medical waste storage and packaging
7Proposal of Appropriate Treatment/disposal methods of biomedical waste
Applicable for Rural Health facilities in Sudan
8Mercury spill handling and management
9Personnel training procedures
1.1 Current situation of water supply in the rural health facilities:-
There is no adequate sources of water supply in most of the health facilities in rural areas the main source is harvesting rain water and some of them are connected to the town net but there is no regular supply.
In these situations it is difficult to program for waste management, since the lack of water will affect sanitation problem, (toilets) and the general environmental health in the rural health facilities.
1.2 Best practice of water sources:
It is imperatively important for each health facility to have adequate supply of water either by having bore- hole with reservoir or storage tank to secure enough water for minimum three days and to be refill by truck from the nearest source of supply
1.3 Best Practice for sewerage (toilet) system
5
In most of the health facilities toilets are primitive pit latrine, the best alternative for short term will be to have a septic tank big enough or biological fermentation tank which will make primary treatment of the sewage with a suitable size that can hold the sewerage for many months depends on the average number of patients visit the health facility and the permanent staff, for long term proper waste water treatment plant should think of it.
2.0 Medical waste minimization options
The waste management hierarchy is:
Source reduction of waste
Reuse the waste
Recycling the waste
Treatment
Finally disposal( least preferred)
Therefore the best practice for waste management that rural health care faculties can start with is the source reduction
2.1 Source Reduction
Source reduction can be achieved by the implementation of policies and procedures that would reduce waste. The key operating practices that can be utilized to affect waste minimization are as follows:
2.1
Waste segregation
2.2
Centralize purchasing and dispensing of drugs and other hazardous chemicals
2.3
Use first-in, first-out policy in dispensing drugs and chemicals to minimize the wastes generated because of exceeded shelf life
2.4
Require inventory checks before ordering/using new stock
2.5
Minimize acceptance of free samples that are likely to leave as hazardous waste
2.6
Provide employee training in hazardous materials management and waste minimization.
3-0 Regulation and control system
6
The M of H should enforce the Act of Medical Waste Management to regulates, manages, and controls the treatment and disposal of medical waste in a safe and proper manner. It requires
3.1
Define the responsibility of the waste management in each health facility
3.2
Laws and regulatory programs addressing medical waste management also should be enacted by several states in response to the public's concerns over the AIDS epidemic.
3.3
Secure financial resources for waste management
3.4
Raise the awareness among decision ( municipality officers , civil societies , environmentalist and/or university in each state ) about the importance of biomedical waste management
These measures will reduce effectively waste and it’s the spread around the health facilities.
4.0 Medical Waste collection
A routine programmed for biomedical waste collection should be established as part of the health-care waste management plan.
Certain recommendations should be followed by the ancillary workers in charge of waste collection:
4.1
Collection of MW should be Source Collection, within the Wards , Nursing Stations/
Others , to the common collection Point for Segregation or treatment
4.2
Waste should be collected daily (or as frequently as required) and transported to the designated central storage site.
4.3
No bags should be removed unless they are labelled with their point of production
(hospital and ward or department) and contents.
4.4
The bags or containers should be replaced immediately with new ones of the same type.
4.5
A supply of fresh collection bags or containers should be readily available at all locations where waste is produced.
4.6
The wastes should be placed in rigid or semi-rigid and leak-proof containers.
7
6.0
Handling and disposal facilities
6.1
All personnel handling infectious medical waste shall wear gloves and additional protective medical clothing and personal protective equipment (PPE) appropriate to the level of risk they encounter as illustrated in Fig ( ) and shall remove any protective medical clothing used prior to leaving the work area and to place it in a designated area or container.
6.2
Protective medical clothing and PPE should not be submitted for laundering unless sterilized. When-performing procedures where splashing is not expected, gloves are the minimum PPE that may be worn.
6.3
When performing procedures where smashing may occur or when infectious medical waste bags or containers may contact more than the worker's hands and wrists, the following medical protective clothing and PPE is required in addition to gloves
6.4
. Appropriate protective medical clothing is that does not permit infectious medical waste from penetrating and reaching work clothes or skin
6.5
Eye protection, surgical face masks, and face shields when personnel may reasonably anticipate facial exposure to infectious medical waste.
Proper protection is must for handling biomedical waste
8
Proper segregation and handling of Medical waste
Containers should be replaced when full and carefully sealed shut. Also, containers that are to be reused should be thoroughly decontaminated before reuse and should not be used for any other purpose. Containers to be transported should be protective of transport workers. For example, sharps (glass, syringes, needles, etc.) should be placed in puncture-proof containers. Before any medical/infectious waste container or package is moved to another on-site location for storage, treatment, disposal, or repackaging should be done, and it should be clearly labeled/relabeled as medical/infectious waste.
Fig.( ) Examples of reusable plastic medical waste containers for all medical waste with the exception of trace chemo, cytotoxic, pharmaceutical and pathological wastes.
9
Fig.( )Examples of corrugated boxes which are disposable cardboard boxes that have a lab lid on the top. Once the box is full, the lid is closed, sealed and ready for removal, as well as biohazard bags fit inside of the medical waste containers
Fig. ( ) Example of disposable sharps containers
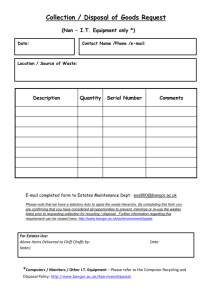
6.0 Medical waste Storage and packaging:
Biomedical waste other than sharps and bulk liquids must be packaged in sealed red bags which are leak proof and rip resistant. Sharps shall be placed in rigid leak and puncture resistant containers. Bulk liquids to be transported off-site shall, in addition to the above requirements, be placed in rigid containers.
All Medical waste must be stored in a secure area designated for this material.
Pathological waste, cultures, and animal carcasses stored anywhere for more than 24 hours must
10
be refrigerated. Storage of biomedical wastes may need to be stored at the facility of origin until a large enough quantity is accumulated to warrant on-site treatment, or until transport to an offsite treatment facility is scheduled. The following general guidelines apply to typical medical waste storage, transfer, and collection areas:
6.1 Store medical/infectious waste in a designated area located at or near the treatment site or the waste pickup point.
6.2 Areas used to store medical/infectious waste should be durable, easily cleanable, impermeable to liquids, and protected from vermin and other potential mechanisms that might spread infectious agents.
6.3 The manner of storage should maintain the integrity of the containers, prevent leakage of waste from the container, provide protection from the weather, and maintain the waste in a nonputrescent, odorless state (this may include refrigeration).
6.4 Storage areas should have adequate ventilation systems.
6.5 Access should be securely controlled and limited. Due to the hazardous nature of some medical wastes, appropriate methods of storing waste will help to prevent accidents and infections. Storage locations should be accessible, exclusive, secure, hygienic and sanitary, located as far as possible from patient treatment areas. Storage locations should be integrated with the physical and architectural infrastructure of the healthcare facility.
11
7.0 Proposal of Appropriate Treatment/disposal methods of Medical waste
Applicable for Rural Health facilities in Sudan
7.1 Disposal of Contaminated Waste
Best Practice for disposal of contaminated waste may include:
Pouring liquids or wet waste directly into a safe sewerage system If a sewerage system does not exist, dispose of waste in a deep hole and cover.
Incinerating (burning) items to destroy the item as well as any microorganisms. (This is the best method for disposal of contaminated waste. Burning also reduces the bulk volume of waste and ensures that the items are not scavenged and reused.)1
Burying all contaminated wastes to prevent further handling.
Encapsulation is recommended as the easiest way to safely dispose of sharps. Sharps are collected in puncture-resistant and leak proof containers. When the container is threequarters full, a material such as cement (mortar), plastic foam or clay is poured into the container until completely filled. After the material has hardened, the container is sealed and may be landfilled, stored or buried. It is also possible to encapsulate chemical or pharmaceutical waste together with sharps (WHO 1999).
7.2 BEST PRACTICE FOR THE DISPOSAL OF LIQUID CONTAMINATED WASTES
Liquid contaminated waste (e.g., human tissue, blood, feces, urine and other body fluids) requires special handling, because it may pose an infectious risk to healthcare workers who contact or handle the waste.
STEP 1 : Wear PPE (utility gloves, protective eyewear and plastic apron)
STEP 2 : Carefully pour wastes down a utility sink drain or into a flushable toilet and rinse the toilet or sink carefully and thoroughly with water to remove residual wastes. Avoid splashing .
12
STEP 3 : If a sewage system doesn’t exist, dispose of liquids in a deep, covered hole, not into open drains.
STEP 4 : Decontaminate specimen containers by placing them in a 0.5% chlorine solution for 10 minutes before washing them.
STEP 5 : Remove utility gloves (wash daily or when visibly soiled and dry).
STEP 6 : Wash and dry hands or use an antiseptic hand rub as described above.
Cholera Epidemic In case of a cholera epidemic, hospital sewage must also be treated and disinfected. Vibrio cholerae, the causative agent of cholera, is easily killed and does not require use of strong disinfectants. Buckets containing stools from patients with acute diarrhea may be disinfected by the addition of chlorine oxide powder or dehydrated lime oxide (WHO 1999).
7.3 BEST PRACTICE FOR THE DISPOSAL OF SOLID CONTAMINATED WASTES
Solid contaminated waste (e.g., surgical specimens, used dressings and other items contaminated with blood and organic materials) may carry microorganisms.
Remember :
Never use hands to compress waste into containers.
Hold plastic bags at the top.
Keep bags from touching or brushing against the body while lifting or during transport.
STEP 1 : Wear heavy-duty or utility gloves when handling and transporting solid wastes.
STEP 2 : Dispose of solid wastes by placing them in a plastic or galvanized metal container with a tight-fitting cover.
STEP 3 : Collect the waste containers on a regular basis and transport the burnable ones to the incinerator or area for burning.
Note : If incineration is not available or waste is non burnable, bury it.
STEP 4 : Remove utility gloves (wash daily or when visibly soiled and dry).
STEP 5 : Wash and dry hands or use an antiseptic hand rub as described above.
13
7.4 INCINERATION
Incineration is a high-temperature process that reduces the volume and weight of waste. This process is usually selected to treat waste that can not be recycled, reused or disposed of in a sanitary landfill or dumpsite.
7.4.1 Types of Incinerators
Incinerators can range from extremely sophisticated, high-temperature ones to very basic units that operate at much lower temperatures. All types of incinerators, if operated properly, eliminate microorganisms from waste and reduce the waste to ashes. Four basic types of incinerators are used for treating waste: a. Double-chamber, high-temperature incinerators are designed to burn infectious waste. b. . Single-chamber, high-temperature incinerators are less expensive and are used when doublechamber incinerators are not affordable.
Note : In this chapter, only inexpensive drum or brick incinerators will be discussed. c . Rotary kilns operate at high temperatures and are used for destroying cytotoxic substances and heat-resistant chemicals. d. Drum or brick (clay) incinerators operate at lower temperatures and are less effective, but can be made locally using readily available materials.
7.4.2 Types of Waste That Should Not Be Incinerated
Pressurized gas containers (aerosol cans)
Large amounts of reactive chemical waste
Silver salts and photographic or radiographic wastes
Plastic containing polyvinyl chloride (blood bags, IV tubing or disposable syringes)
Waste with high mercury or cadmium content, such as broken thermometers, used batteries and lead-lined wooden panels Adapted from : WHO 1999.
14
7.4.3 How to Build and Use a Simple Drum Incinerator for Waste Disposal
Simple drum incinerator is the Best practice for biomedical waste treatment For healthcare facilities with limited resources and where high-temperature incinerators are not affordable, waste may be incinerated in a drum incinerator, a drum incinerator is the simplest form of singlechamber incinerator. It can be made inexpensively and is better than open burning. in rural health facilities in Sudan , since the quantity of waste is limited and there are no other alternatives.
STEP 1 : Where possible, select a site downwind from the clinic.
STEP 2 : Build a simple incinerator using local materials (mud or stone) or a used oil drum (e.g., a 55-gallon drum). The size depends on the amount of daily waste collected.
STEP 3 : Make sure the incinerator has:
Sufficient air inlets underneath for good combustion
Loosely placed fire bars to allow for expansion
An adequate opening for adding fresh refuse and for removal of ashes 2 Adapted from :
SEARO/WHO 1988.
A long enough chimney to allow for a good draft and evacuation of smoke
STEP 4 : Place the drum on hardened earth or a concrete base.
STEP 5 : Burn all combustible waste, such as paper and cardboard, as well as used dressings and other contaminated wastes. If the waste or refuse is wet, add kerosene so that a hot fire burns all the waste. Ash from incinerated material can be treated as non contaminated waste.
15
16
7.5 Open burning
Open is not recommended because it is dangerous, unsightly and the wind will scatter the waste.
If open burning must be done, burn in a small, designated area, transport waste to the site just before burning and remain with the fire until it is out.
7.6 BURYING WASTE
Only contaminated and hazardous waste needs to be buried. In healthcare facilities with limited resources, safe burial of wastes on or near the facility may be the only option available for waste disposal. To limit health risks and environmental pollution, some basic rules are:
Access to the disposal site should be restricted. (Build a fence around the site to keep animals and children away.)
The burial site should be lined with a material of low permeability (e.g., clay), if available.
Select a site at least 50 meters (55 feet) away from any water source to prevent contamination of the water table.
The site should have proper drainage, be located downhill from any wells, free of standing water and not in an area that flood.
Large quantities (over 1 kg) of chemical (liquid) wastes should not be buried at the same time; burial should be spread over several days. Safe on-site burial is practical for only limited periods of time (1–2 years), and for relatively small quantities of waste. During the interval, staff should continue to look for a better, permanent method for waste disposal.
7.6.1 How to Make and Use a Small Burial Site for Waste Disposal
STEP 1 : Find an appropriate location
STEP 2 : Dig a pit 1 meter (3 feet) square and 2 meters (6 feet) deep. The bottom of the pit should be 2 meters (6 feet) above the water table.4
STEP 3 : Dispose of the contaminated waste in the pit and cover the waste with 10–15 cm (4–6 inches) of dirt each day. The final layer of dirt should be 50–60 cm (20–24 inches) and
17
compacted to prevent odors and attraction of insects, and to keep animals from digging up the buried waste. Depending on the volume of waste, this pit should last 30 to 60 days.
A Small Burial Pit Adapted from : WHO 1999.
3 Adapted from : SEARO/WHO 1988.
4 Burial can be used as a method of waste disposal only where the water table is more than 12 feet below the surface.
18
7.7 BEST PRACTICE OF DISPOSAL OF HAZARDOUS WASTE5
7.7.1 Chemical Waste
Chemical waste includes residues of chemicals in their packaging, outdated or decomposed chemicals, or chemicals that are no longer required. Small quantities of chemical waste are generally collected in containers with infectious waste, and are incinerated, encapsulated or buried. Large quantities should not be collected with infectious waste. Because there is no safe and inexpensive method for their disposal, the treatment options are the
Following:
Incineration at a high temperature is the best option for the disposal of chemical waste.
If this is not possible, return the chemical waste to the original supplier.
Remember :
Chemical waste of different types should never be mixed.
Chemical waste should not be disposed of in sewer systems. Because either method is expensive and may be impractical, it is important to keep chemical waste to a minimum.
7.7.2 How to Dispose of Used Chemical Containers
Rinse glass containers thoroughly with water. Glass containers may be washed with soap, rinsed and reused.
For plastic containers that contained toxic substances such as glutaraldehyde (e.g.,
Cidex®) or formaldehyde, rinse three times with water and dispose of by burning, encapsulating or burying. Do not reuse these containers for other purposes.
7.7.3 Pharmaceutical Waste Small quantities
Pharmaceutical (drugs or medicine) waste are usually placed in containers with infectious waste and disposed of in the same way— either incinerated, encapsulated or safely buried. It should be noted, however, that temperatures reached in a single-chamber drum or brick incinerator may be insufficient to totally destroy the pharmaceuticals; therefore, they can
19
remain hazardous.Small quantities of pharmaceutical waste, such as outdated drugs (except cytotoxics and antibiotics), may be discharged into the sewer but should not be discharged into natural waters (rivers, lakes, etc.).
7.7.4 Disposal of Large amounts of pharmaceutical waste
Large quantities of pharmaceutical waste may be disposed of by the following methods: may be disposed of by the following methods:
Cytotoxics and antibiotics may be incinerated with the residues then going to the landfill.
(An incinerator, like those used in making cement, that is capable of reaching a combustion temperature of at least 800°C should be used.)6 5
Adapted from : WHO 1999.
When incineration is not available, these pharmaceuticals should be encapsulated.
Water-soluble, relatively mild pharmaceutical mixtures, such as vitamin solutions, cough syrups, intravenous solutions, eye drops, etc., may be diluted with large amounts of water and then discharged to sewers (where sewerage systems exist).
If all else fails, return pharmaceutical waste to the original supplier if
Possible.
8.0 Mercury spill handling and management:
Mercury usually becomes a waste because of instrument breakage and cannot be treated by techniques described here. Mercury should be collected in a special container and shipped to a recycler. Using electronic devices for measuring temperature and blood pressure is the most effective way to eliminate mercury from the waste streams.
While dealing with a mercury spill the hospital workers should be ready with the following items, which can be put together in all the wards in advance and labeled as
MERCURY CONTAIN-MENT KIT. This would ensure the availability of these things the moment the spill occurs. a. Nitrile gloves or at least two pairs of latex gloves (Mercury passes mercury can pas through single pair of latex gloves).
20
b. Face mask. c. Protection for the eyes. d. Scotch Tape. e. 10 c .c syringe. f. Covered plastic/ glass container with water. g. Posters depicting the process of mercury spill containment PRECAUTION: Mercury-based instruments should never be used in a carpeted area.
Once a mercury spill occurs the steps to be taken are: a. never touches mercury with bare hands, as mercury is absorbed quickly through the skin. b. Remove all jewellery when dealing with mercury, as mercury combines with gold, silver and other metals. c. Clear the area around the spill and contain the spread of mercury. d. Wear all the protective gear. e. Try to gather all the small droplets of mercury with the help of two hard cardboard sheets and then use a syringe to suck this big droplet of mercury. (Mercury is a non wetting liquid, which has the affinity to hold to itself; thus when you get all the small drops of mercury together, they join and form a big drop). f. Pour contents of the syringe into a plastic/ glass container with 5 to 10 ml of water. g. Put scotch tape, if used, in the plastic/ glass container. Put the used syringe back in the kit, upside down.
21
9.0 Personnel training procedures:
Health care facilities should develop policies and procedures for following up on employees who sustain a puncture wound from a used sharp. This information must be available in the occupational health service manual and the infection control manual, and be readily accessible to all appropriate staff. It should include procedures to protect and/or follow up with the employee possibly exposed to tetanus, Hepatitis B, Hepatitis C, and HIV. Health care facilities should ensure that a mechanism exists for following up on employees who suffer a puncture wound at any time of the day incorporating the most current recommendations of international heath organizations sources such as WHO and should train all the employees and health staff the training programs must emphasize the following:
1.0 Personal hygiene, especially washing hands; b. The facility's procedures for the reduction, segregation, collection, packaging,
Colored coding, labeling, storage, and in-house movement of waste; c. Methods for preventing the transmission of infections related to waste handling procedures; d. The hazards of those materials to which workers may be exposed; and e. The actions to be taken and which supervisory staff should be notified in the event of an accident.
2. Employee training programs should be continually assessed and reinforced, and their content periodically reviewed and updated as necessary. Consideration should be given to adapting the training programs to suit personnel who may not be fluent in the official language of predominant use or who may not be fully literate.
3. To minimize the occupational health risks associated with the handling and disposal of biomedical waste, occupational health care programs should: a. Include a regular assessment of waste management procedures to assure compliance with applicable standards and all applicable federal, territorial and municipal regulations and legislation;
22
b. Provide appropriate personal protective equipment and hand washing facilities for workers involved in various stages of waste handling and disposal; c. Include a written procedure to handle and report needle- stick injuries and other waste handling incidents. Injuries caused by needle- sticks and sharp instruments should be documented, reviewed, and changes implemented to prevent similar incidents in the future; d. Emphasize the need for point of generation segregation so that waste is placed within an appropriate waste container; e. Review the type and quality of waste containers used and, if necessary, have them upgraded to containers considered to be more suitable; f. Review handling practices to determine if problems are the result of excessive or inappropriate handling. If so, modify the handling techniques; and consult with employees being affected by inappropriate handling techniques and invite their participation in determining effective solutions.
4. Waste haulers and handlers should always be appropriately clothed and wear personal protective equipment so that harmful agents, whether physical, chemical, or infectious, are prevented from gaining access to open wounds, cuts, or by absorption through the skin. Personal protective equipment may include gloves, gowns, safety glasses, protective footwear, etc.
23