w COMIRB Protocol - University of Colorado Denver
advertisement

On the Web at http://comirbweb.uchsc.edu
w
PROTOCOL #:
COMIRB Protocol
(Use Protocol Manager on the COMIRB Website)
COLORADO MULTIPLE INSTITUTIONAL REVIEW BOARD
CAMPUS BOX F-490 TELEPHONE: 303-724-1055 Fax: 303-724-0990
Project Title:
CoPARC: Colorado Pulmonary Alcohol Research Consortium
Principal Investigator:
Ellen L. Burnham, MD, MS
I. Hypotheses and Specific Aims
Our resource will be focused on establishing pulmonary effects of alcohol use disorders
(AUDs), including alcohol abuse and dependence that contribute to an increased
susceptibility for pneumonia. Based on prior investigations, we hypothesize that alcoholrelated alterations on pulmonary oxidative stress, the cytokine milieu, and endogenous
proteins lead to an increased susceptibility to pneumonia through their adverse effects on
alveolar macrophage (AM) and bronchial airway epithelial cell (BAEC) function, and their
influence on the respiratory tract microbiome. These abnormalities may be further
augmented in the setting of smoking.
Specific Aims: Determine the mechanisms whereby AUDs increase the predisposition to
pneumonia via effects on
1. Alveolar macrophage (AM) efferocytosis, apoptosis, and maturation, and their
relationship to:
1a. Zinc deficiency
1b. Pulmonary oxidative stress
2. Bronchial airway epithelial cell (BAEC) function, including:
2a. Expression of toll-like receptor-2 (TLR-2) and ciliary motility
2b. Response to protein adducts formed in the setting of AUDs and smoking
3. Respiratory tract microbial ecology, and its relationship to alterations in antimicrobial
protein composition and function within the alveolar space
II. Background and Significance:
The effect of AUDs on the incidence and severity of pneumonia poses a substantial
burden to our health care system. Pneumonia (along with influenza) is responsible for
approximately 1.3 million hospitalizations and costs our economy $40.2 billion dollars
annually(1). It ranks as the eighth leading cause of death, and is the most common cause
of death from infectious diseases in the US(2). An estimated 50% of patients with
pneumonia have an AUD(3), and these patients have more severe symptomatology,
longer and more expensive hospitalizations, and higher mortality (4);(5);(6), despite their
relatively younger age (<60 years old(7;8)). Among surgical patients with AUDs, an
increased risk of post-operative pneumonia has similarly been described(9) in association
with prolonged ventilator dependence, a longer ICU stay, and mortality(10;11). As a result,
there are more AUD-associated deaths from pneumonia when compared to the number of
deaths due to alcohol-related liver disease(12), traffic accidents(13), or alcohol-related
pancreatitis(14). Successful completion of the proposed aims will lead to identification of
therapies to decrease the incidence of alcohol-associated pneumonia.
Protocol Template
CF-146, Effective 7/10/11
Page 1
On the Web at http://comirbweb.uchsc.edu
Co-morbid factors, including smoking, can further alter susceptibility for
pneumonia in the setting of AUDs. For example, investigations in animal models have
revealed that ciliary dysfunction is compounded in the presence of both alcohol and
cigarette smoke compared to either exposure alone(15), suggesting that a smoke/AUD
interaction may adversely affect airway innate immune function (16). Prior clinical
investigations have not accounted for the influence of these common co-morbid factors on
pneumonia in the AUD setting. Therefore, investigations proposed will specifically do so
by (1) ensuring sample sizes are large enough to explore differences between AUD/nonAUD subjects, with and without a specific confounder, (2) utilizing study designs (e.g. pairmatching) and statistical analyses (e.g. stratification by smoking) to factor in confounder
effects on outcome variables.
Four other institutions that are leaders in alcohol-related lung research have
expressed overwhelming interest in establishing a consortium with UCD to improve
translational discoveries related to alcohol-associated pneumonias. The majority of
investigations from sites outside of UCD have been conducted in animal models, although
the population and infrastructure at all but one of these sites (University of Nebraska) can
support the research focus of this consortium. Combining four sites’ clinical research
capabilities will greatly enhance the feasibility of the proposed translational research
projects by ensuring sizable numbers of human subjects, with and without AUDs. Denver
is home to a large population of racially diverse AUD subjects with little other co-morbidity.
Emory, the only other site presently conducting clinical alcohol-related lung research, has
a largely African-American population, as does LSU, where clinical lung investigations in
subjects with HIV/healthy controls are on-going. Emory and LSU have agreed to further
supplement our UCD resource with samples from their sites. With a large cohort of
diverse subjects, we can explore effects of AUDs on the predisposition for pneumonia
while accounting for important confounders, including smoking. Our resource will create
productive interactions in a forum that encourages a logical investigative pathway
extending from animal models to the bedside. It will also facilitate the recruitment of new
investigators interested in alcohol-associated pulmonary research.
The research paradigm for alcohol-related pneumonia has historically been weighted
heavily toward animal model and cell-line based research. This paradigm has resulted in
few phase III trials, and so far has failed to provide clinically relevant interventions for
humans(17). The establishment of this consortium seeks to shift the standard paradigm
and transform this research model by establishing a logical progression of investigations
with human subjects in order to fuel the conduct and improve success of phase III clinical
trials. This consortium’s proposed experiments focus on animal-to-human investigations,
confirming differences in lung-specific outcome measures in individuals with AUDs
compared to healthy individuals. The goals of planned experiments are (1) to explore
novel hypotheses relevant to the development of pneumonia, (2) to confirm significant
alcohol-related animal model abnormalities, and (3) to extend small-scale observations
made previously in in vitro human investigations into a larger cohort to better account for
confounders, to determine the most important mechanisms in AUDs that predispose to
pneumonia. Importantly, this research will identify potential therapies to decrease the
incidence of pneumonia in individuals with AUDs and other critical illnesses, such as
sepsis. Robust and persistent AUD-associated alterations will be targeted for expanded
investigations, while differences initially observed in animal models but not confirmed in
humans will not require further interest or investigations.
Protocol Template
CF-146, Effective 7/10/11
Page 2
On the Web at http://comirbweb.uchsc.edu
The proposed research capitalizes on the expertise of a diverse group of
investigators and will promote cross-site synergy and discovery in the field of
alcohol-related pneumonias. By design, this R24 will facilitate frequent interactions
between our sites that will encourage collaboration. For example, LSU investigators have
prior experience in assessing the respiratory tract microbiome, and will establish its
microbial diversity in the setting of AUDs, while UCD is focused on determining
antimicrobial protein composition in the alveolar space. Collectively, these two groups’
observations could identify new antimicrobial approaches in patients with AUDs.
Alternatively, alterations in zinc homeostasis assessed by investigators at Emory may
ultimately prove to modulate AM maturity (as they hypothesize), and can also be explored
in the context of other AM activities, including efferocytosis, one focus of UCD
investigators.
III. Preliminary Studies/Progress Report:
We have successfully enrolled otherwise healthy subjects with alcohol use
disorders and matched controls into protocols involving the CTRC at UCH. Since
2007, we have been recruiting subjects from Denver CARES for IRB-approved protocols
examining the effects of alcohol on the lung. One of these protocols involved a 2 night
observational trial including one bronchoscopy (n=50 subjects with AUDs, n=15 controls),
while the other involved an 8 day clinical trial with two bronchoscopies (n=30 subjects) on
the CTRC. All planned bronchoscopies were completed successfully on the unit, using
conscious sedation, without adverse events. Subjects with AUDs were managed for
alcohol withdrawal symptoms with the CIWA protocol; no episodes of complicated alcohol
withdrawal requiring escalation of care occurred. No subjects failed to complete assigned
protocols.
SA 1 [EU Project 1]: Alternative (M2) activation of AMs antagonizes M1 activation, leading
to AMs that are unable to phagocytize particles but can abnormally generate reactive
oxygen species, arginase, TGF-, and fibronectin (18;19). This can contribute to
fibroblast proliferation with collagen production in the lung(19). Our preliminary data with
NR8383 cells (a macrophage cell line), and AMs from a rat AUD model suggest that
chronic ethanol treatment leads to increased expression of AM M2 activation markers. In
our preliminary studies, expression of M2 activation markers was examined on human
AMs via fluorescent microscopy. AUDs were associated with decreased AM expression of
CD32, a marker of terminal differentiation, while expression of arginase-1, galectin-3, IL13, mannose receptor, and TGF-β1 were increased.
SA 1a [EU Project 2]: AUDs are associated with zinc deficiency which has the potential to
affect normal epithelial and immune cell functions, and lead to an increased susceptibility
for pneumonia. Our group has demonstrated in a rat model that chronic alcohol ingestion
is associated with altered expression of key zinc transporters and storage proteins in the
lung, and decreased zinc levels in the alveolar compartment(20). In AMs from these
animals, in vitro treatments with zinc increased intracellular zinc levels, promoted these
cells’ terminal differentiation, and improved their bacterial phagocytic capacity. If zinc
improves AM function and maturation, zinc therapy could be a logical choice to restore
normal AM function in those with AUDs.
SA 1b [EU/UCD Project]: AUDs have been associated with excessive pulmonary
oxidation through effects on the thiol glutathione(21);(22). However, the impact of AUDs
on cysteine/cystine thiol pairs is not known. Oxidation of cysteine/cystine pairs promotes
signal transduction and alters cellular responses(23;24). Therefore, it is a key factor
influencing proper innate immune function.
Establishing the thiol species most
Protocol Template
CF-146, Effective 7/10/11
Page 3
On the Web at http://comirbweb.uchsc.edu
prominently affected by AUDs, and developing methods to measure intrapulmonary
oxidation non-invasively may expedite the identification of individuals who would most
benefit from anti-oxidant therapy to restore proper immune function. We have examined
redox potential in non-invasively collected exhaled breath condensate (EBC) from those
with AUDs (n=27) compared to controls (n=8) and determined that oxidative stress indices
reflect what is found in epithelial lining fluid (ELF) within BAL(25).
SA 2a [UNMC Project 1]: TLR-2 receptors on airway epithelium recognize peptidoglycan,
the cell wall component found in Gram (+) respiratory pathogens such as S. pneumoniae
(26). This initiates a signaling cascade that results in inflammatory cytokine secretion.
Our UNMC group reported that alcohol causes a biphasic modulation of TLR-2 expression
on airway epithelium, where brief alcohol exposure induces TLR-2 upregulation, while
prolonged alcohol exposure causes downregulation(26). These changes result in
dysfunctional inflammation. In our preliminary data, mice fed alcohol for 6 weeks
(according to the Cook model(27)) express very little TLR-2 on the airway epithelium;
moreover, we have observed similar changes in human airway epithelial cells lines in
vitro. However, the effects of AUDs on airway epithelial cells in vivo are not known.
SA 2b [UNMC Project 2]: Investigators at UNMC have developed a well-characterized
mouse model of co-exposure to alcohol and cigarette smoke(15) that we have utilized to
examine reactive aldehyde protein modification, specifically malondialdehde-acetaldehyde
(MAA) protein adducts to nascent lung proteins. These adducted lung proteins activate
Protein Kinase C epsilon (PKCε) through their effect on scavenger receptors (SR) of lung
epithelial cells (28). PKCε, in turn, affects airway epithelial cell production of proinflammatory cytokines in the lung(29). Human ELF from individuals with AUDs who
smoke has not been specifically examined to determine MAA protein adduct quantity.
SA 3 [LSU Project]: In the setting of immunodeficiency or mucosal injury to the lung,
normal interactions between the host and microorganisms are deranged, leading to
abnormal microbial colonization of the lower airways. Published data from our LSU group
in animal models suggests that alcohol consumption worsens pneumonia caused by both
bacterial and fungal organisms (reviewed in(30)). However, the spectrum of colonization
in the respiratory tract in patients with AUDs and its contribution to disease is not defined.
We contend that alcohol-induced perturbations in mucosal immunity allow specific species
of the normal lung microbiota to proliferate, competitively excluding other species,
unbalancing and restricting community diversity, and leading to further host immune
dysfunction. This establishes a vicious cycle in which the altered microbiota leads to
further dysregulation of mucosal immunity.
SA 3a [UCD Project 3]: ELF contains a variety of antimicrobial proteins(31) that have
gained additional recognition recently as immune regulators(32). Effects of AUDs on
antimicrobial proteins in the respiratory tract have remained relatively unexplored,
although alcohol metabolites have been demonstrated to adversely affect lysozyme, a
high-abundance antibacterial protein(33). We recently demonstrated that ELF from
subjects with AUDs (n=15, with n=6 controls) has significantly decreased lysozyme
activity (p<0.01) and lactoferrin concentration (p<0.02). Moreover, using linear regression
modeling across a range of ELF protein concentrations, killing of type 2 S. pneumoniae
was inferior by ELF from AUD subjects in an in vitro killing assay compared to ELF from
controls.
IV. Research Methods
A. Outcome Measure(s): Measures are dependent on the specific assay as delineated in the
study design and research measures, below. They include:
Protocol Template
CF-146, Effective 7/10/11
Page 4
On the Web at http://comirbweb.uchsc.edu
1. M2 activation markers on alveolar macrophages
2. alveolar macrophage zinc levels (intracellular)
3. thiol homeostasis in epithelial lining fluid and exhaled breath condensate
4. TLR2 expresssion on airway epithelial cells
5. MAA protein adducts in epithelial lining fluid
6. microbiome within lung
7. antimicrobial proteins in epithelial lining fluid
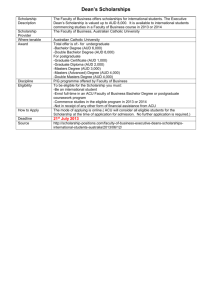
B. Description of Population to be Enrolled:
Subjects with AUDs. We have the capability of safely enrolling approximately 72 subjects
per year and following these subjects to the completion of their protocol(s). These
patients will be Table 1. AUD Subject Inclusion/Exclusion Criteria
recruited
from
Inclusion criteria: Subjects will be eligible to participate in the study if they meet all of the
Denver CARES, following criteria:
the detoxification 1. Alcohol Use Disorders Identification Test (AUDIT) score of 8 for men and ≥5 for women.
center associated 2. Last alcohol-containing beverage consumed within the seven days prior to enrollment.
with
Denver Exclusion criteria: Subjects will be ineligible to participate in the study if they meet any of the
Health. We have following criteria:
Prior medical history of liver disease: cirrhosis, total bilirubin ≥ 2.0 mg/dL, or albumin < 3.0
recruited research 1.
g/dL
subjects from this 2. Prior medical history of symptomatic gastrointestinal bleeding
3. Prior medical history of myocardial infarction or congestive heart failure
facility
Prior medical history of end-stage renal disease or serum creatinine ≥ 3 mg/dL
successfully since 4.
5. Prior medical history of asthma
2008.
We 6. Concurrent illicit drug use defined as a positive urine toxicology screen for opiates and
propose to enroll cocaine (to be performed on the CTRC prior to bronchoscopy).
7. Prior history of diabetes mellitus
up to 360 subjects 8. Prior history of HIV, not controlled on medications
with AUDs for 9. Peripheral white blood cell count of less than 3000
Abnormal chest radiograph or spirometry (forced vital capacity or forced expiratory
Years 1-5 of the 10.
volume in 1 second <60% predicted)
proposal.
Their 11. Failure of the subject or the subject’s substance abuse counselor to provide assent
age ranges are 12. Nutritional risk index of less than 95
13. Actively withdrawing from alcohol (defined as a CIWA score of >10)
anticipated to be 14. Age < 18 or > 60
between 35 and 15. Pregnancy
60,
and
their
overall health status should be good, aside from their history of alcohol abuse. Inclusion
and exclusion criteria for subjects with AUDs are listed on table 1. At the UCD site,
subjects with AUDs will be recruited from Denver Health and Hospital Administration’s
Denver
Comprehensive
Table 2. Control Subject Inclusion/Exclusion Criteria
Addictions Rehabilitation and
Evaluation Services (Denver Inclusion criteria: Subjects will be eligible to participate in the study if they
all of the following criteria:
CARES), a local detoxification meet
1. Alcohol Use Disorders Identification Test (AUDIT) score of <2 for men
center and our collaborating and <1 for women.
site, after their discharge from
Exclusion criteria: Subjects will be ineligible to participate in the study if they
this facility. At the Emory site, meet any of the following criteria:
subjects with AUDs will be 1. Prior medical history of liver disease: cirrhosis, total bilirubin ≥ 2.0
recruited from the outpatient mg/dL, or albumin < 3.0 g/dL
2. Prior medical history of symptomatic gastrointestinal bleeding
detoxification clinic at the 3. Prior medical history of myocardial infarction or congestive heart failure
Atlanta VA Medical Center, and 4. Prior medical history of end-stage renal disease or serum creatinine ≥ 3
from the Grady Memorial mg/dL
5. Prior medical history of asthma
Hospital
Emergency 6. Concurrent illicit drug use defined as a positive urine toxicology screen
Department population.
IRB for opiates and cocaine (to be performed on the CTRC prior to
bronchoscopy).
approval to recruit patients at 7. Prior history of diabetes mellitus
Protocol Template
CF-146, Effective 7/10/11
8. Prior history of HIV positivity not controlled on medications
9. Peripheral white blood cell count of less than 3000
10. Abnormal
radiograph or spirometry (forced vital capacity or forced
Pagechest
5
expiratory volume in 1 second <60% predicted)
11. Nutritional risk index of less than 95
12. Age < 18 or > 60
13. Pregnancy
On the Web at http://comirbweb.uchsc.edu
the Emory site is in place currently.
Healthy control subjects. Approximately 250 healthy controls will also be enrolled over
this same time frame (50 per year for years 1-5).
These subjects will either be recruited from the Denver VA and Atlanta VA Medical
Centers’ smoking cessation clinics (smoking controls), and the pulmonary/general
medicine clinics at LSU HSC. Additionally, subjects may be enrolled from the UCD, EU,
and LSU medical center campuses. Their age ranges, smoking history, and gender will be
reflective of the characteristics of our subjects with AUDs. Since it is possible for smoking
to affect many of the lung-specific outcome variables we intend to explore, a detailed
history of current and former smoking practices will be obtained from control subjects in
order to match them as closely as possible to the smokers contained within the AUD
subject cohort. Inclusion and exclusion criteria are listed in table 2. Of note, a positive
urine toxicology screen will be performed on the CTRC for all AUD subjects and controls;
evidence of recent cocaine and heroin use will automatically exclude individuals from
participation.
C. Study Design and Research Methods
Costs of performing these experiments (e.g. reagent costs, equipment costs) will be shared
by UCD investigators and external collaborating sites.
SA 1 [EU Project 1]: We hypothesize that a history of AUDs will be associated with
upregulation of M2 activation markers in human subjects. We will test this hypothesis by
assessing expression of M2 markers on AMs obtained from subjects with and without
AUDs, including FIZZ1, SR-A, MR, CD11c, CD32, arginase, galectin-3, IL-13, TGF-β, and
fibronectin(18;34;35). We will also determine their arginase activity. For proposed
experiments, flow cytometry and Western blot will be used to confirm differences in AM
M2 marker expression in the setting of AUDs.
SA 1a [EU Project 2]: we hypothesize that AUDs will be associated with AM zinc
deficiency that mediates alcohol-induced dysfunction of these cells. To test this
hypothesis, we will determine (1) if AUDs are associated with decreased intracellular zinc
levels in AMs and (2) if in vitro zinc supplements can restore AM bacterial phagocytic
capacity.
SA 1b [EU/UCD Project]: We hypothesize that AUDs will be associated with abnormal
cysteine/cystine homeostasis within ELF. We further hypothesize that measurements of
thiol pairs in EBC will reflect thiol homeostasis in ELF within the same subject over time.
We will test these hypotheses by measuring the thiol pairs GSH/GSSG and
cysteine/cystine from ELF and EBC samples obtained concurrently from subjects with
AUDs immediately after sobriety, and from control subjects and again after one week of
supervised abstinence, matched as closely as possible for smoking, age, and gender in
both smokers and non-smokers(22;25).
SA 2a [UNMC Project 1]: We hypothesize that AUDs decrease TLR-2 expression on
human airway epithelial cells through a mechanism that involves TLR-2 promoter
methylation. We will test this hypothesis by utilizing BAECs derived from AUD subjects
and matched controls to (1) measure baseline TLR-2 expression using quantitative
polymerase chain reaction (PCR), and fluorescence activated cell sorting (FACS) (36); (2)
assess inflammatory cytokine production for IL-6, IL-8, TNF, and IL-1 by these cells in
response to peptidoglycan stimulation via ELISA(36); (3) measure ciliary beat frequency
Protocol Template
CF-146, Effective 7/10/11
Page 6
On the Web at http://comirbweb.uchsc.edu
of BAECs using microscopic and videoscopic techniques, and correlate with NO levels in
ELF(37);(38), and (4) quantify methylation of the TLR-2 promoter. These latter
experiments will be conducted in the methylation core lab at UNMC under the direction of
Dr. Tricia LeVan.
SA 2b [UNMC Project 2]: We hypothesize that the combination of alcohol and smoking
will lead to increased MAA protein adducts in human ELF compared to either stimulus
alone, and their quantity will be associated with lung inflammatory cytokines. Further, we
hypothesize that specific SR-A polymorphisms will also be associated with lung
inflammatory cytokine quantity. We will test these hypotheses by quantifying MAA adducts
in the ELF of subjects with AUDs and healthy controls (smokers and non-smokers)(39).
Additionally, we will perform genotyping assays on extracted DNA from blood using the
Sequenom iPLEX technique (year 5 of proposal). Panels will be developed to incorporate
all of tag SNPs and missense mutations in the SR-A gene.
SA 3 [LSU Project]: We hypothesize that excessive alcohol consumption reduces
microbial ecosystem diversity, which, in turn, initiates both pulmonary and systemic
immune activation. We will test this hypothesis by (1) defining the respiratory tract
microbial ecology in individuals with AUDs and controls, and (2) correlating the AUDassociated microbiota with pulmonary and systemic immune activation (as measured in
SA 3b). These analyses will characterize the microbial community composition and/or
specific lineages of interest in relation to AUDs, and correlate these with biomarkers of
inflammation and clinical parameters. For our experimental approach, PCR amplification
of the V4 hypervariable region and the ITS1 region in rRNA genes along with massively
parallel Roche 454 pyrosequencing will be used by our laboratory at LSU to survey
bacterial / archaeal and fungal species diversity and abundance, respectively, in whole
BAL specimens. At least 10,000 sequences per sample will be generated that will allow
us to detect rare operational taxonomic units present at less than 0.1% of the overall
population. The results of the rRNA survey will be used to analyze the composition of
microbial communities from AUD and control subjects. A custom script will be used to
calculate several alpha-diversity indices(40), as well as the estimators of species
richness(41). Intergroup community membership will be compared using Metastats (42).
Partitioning of biological diversity between different subject groups (beta-diversity) will be
analyzed using unweighted and weighted UniFrac(43).
SA 3a [UCD Project 3]: We hypothesize that ELF from subjects with AUDs has decreased
quantity and activity of antimicrobial proteins, and will be associated with impaired killing
of S. pneumoniae in vitro. We will test our hypothesis by quantifying specific antimicrobial
proteins/peptides in ELF from AUD subjects and controls, including secretory
leukoprotease inhibitor, cathelicidin, and SP-D, and determine the contribution of ELF to
killing S. pneumoniae with and without AMs in an in vitro killing assay (44).
D. Description, Risks and Justification of Procedures and Data Collection Tools:
1. Sources of materials. Research material obtained from AUD subjects and pairmatched controls will include:
Clinical data will be collected in a specific case report form, and will include
demographic information; medical history including alcohol use history (e.g. AUDIT
scores), smoking history, and drug use history.
Blood (20 mL) will be drawn via peripheral vein with a minimum 21 G needle into the
appropriate vacutainer tubes. In subjects with AUDs, blood may be sampled up to 7 times
for projects related to specific aim 1b (~15 mL each time).
Protocol Template
CF-146, Effective 7/10/11
Page 7
On the Web at http://comirbweb.uchsc.edu
Exhaled breath condensate (EBC) will be collected from subjects breathing tidally for
10 minutes using an R-tube (Respiratory Research, Charlottesville, VA) that includes a
sterile polypropylene collection tube, mouthpiece, and saliva trap.
Oropharyngeal sampling will be collected by gargling for a total of 60-seconds (rests
permitted) with 10 mL of sterile saline solution. Following the gargle, subjects spit the
saline into a sterile specimen container.
Bronchoscopy procedures will then be performed utilizing telemetry monitoring and
standard conscious sedation protocols on the CTRC. Subjects will have a combination of
BAL, cytologic brushing, and protected specimen brushing (PSB) performed.
a. PSB (microbiologic): Subglottic respiratory tract sampling will be accomplished using
PSB (wire brush with retractable double-sheath and resorbable plug expelled at the time
of brushing) sampling of the right middle lobe (medial segment) bronchioles.
b. Bronchial brushings (cytologic): A paired specimen will be obtained with a sterile
cytology brush in order to collect bronchial epithelial cells for study.
c. BAL will be performed by a method previously described. The bronchoscope will be
wedged into a subsegment of the lobe contralateral to the side that was brushed (right
middle or lingular lobes). Six 35-mL aliquots of sterile, room temperature 0.9% NaCl will
be sequentially instilled (210 mL total) and recovered with gentle aspiration. BAL contents
will be transported to the laboratory in sterile 50 mL conical tubes.
The bronchoscopist will ensure that hemostasis has been achieved prior to scope
removal and the patient monitored closely on telemetry until stable. Subjects will be
discharged after completion of their specific protocol when clinical stability is ensured. If
subjects do not have a responsible adult to take them home, they may stay on the CTRC
or research unit until the following morning after bronchoscopy. AUD subjects will be
reimbursed with supermarket gift cards for their time and effort that cannot be used for the
purchase of alcohol at an amount commensurate with the time and effort required to
complete the protocol. Healthy control subjects will be reimbursed with a check card/debit
card for the same amount as AUD subjects.
Subjects with AUDs will have clinical data collected by research team members at
UCD. All AUD subjects and controls’ samples will be collected in a CTRC (or similar
research) setting. Since all AUD subjects and controls are volunteers, all data and
samples are being collected specifically for the research project, and this fact will be
conveyed to all participants. Using HIPAA language, we will inform all AUD subjects and
controls that their information will be used only for research.
2. Potential risks.
All subjects will be subjected to bronchoalveolar lavage and bronchial brushing
procedures, with the concomitant use of sedative agents (short acting benzodiazepines
and/or narcotics), and topical agents (1% lidocaine) to increase comfort during the
procedure. In general, these procedures are quite safe and well-tolerated, both in
spontaneously breathing individuals as well as those on mechanical ventilatory support.
Common minor side effects from bronchoscopy include cough and nasal or throat pain
from bronchoscopy insertion, and a sensation of difficulty breathing. In the 24 hours
following the procedure, fever is possible 8% of the time; bleeding in the lungs, severe
difficulty breathing or bronchospasm, and death have been reported <1% of the time.
From sedation medications alone, subjects may experience a momentary fall in blood
pressure (5%), slowing of the breathing rate (10%), nausea and vomiting, headache,
hiccoughs, or allergic reactions (each less than 5%). Numbers in parentheses represent
the percentage of subjects who experience this side effect with each bronchoscopy
performed.
We will need to obtain venous access to administer conscious sedation
Protocol Template
CF-146, Effective 7/10/11
Page 8
On the Web at http://comirbweb.uchsc.edu
and to draw blood samples. We will obtain blood from indwelling catheters when they are
present. In some of subjects we will need to obtain blood via a needle stick. We will
initially collect approximately 20 mL of blood. When a venous catheter is placed, or a
needle stick is necessary to obtain blood samples, the subject may feel pain with the
venipuncture. In addition, he or she may receive a small bruise at the site. Collection of
exhaled breath condensate carries a small risk of feeling light-headed (1%).
In AUD subjects and healthy controls, a chest radiograph will be required that will
expose the subject to a small dose of ionizing radiation. This dose of radiation is
generally considered safe. Additionally, spirometry will also be performed that carries a
very small risk of pneumothorax (much less than 1%). Collection of oral gargles with
saline should be associated with no risk to the subject.
In AUD subjects, there is a risk for alcohol withdrawal since patients will be
admitted during the first seven days of abstinence. We will implement the alcohol
withdrawal protocol used by UCH nursing on all AUD subjects admitted. This protocol is
based on the Clinical Institute Withdrawal Assessment (CIWA) where from 30 signs and
symptoms suggesting alcohol withdrawal, the scale has been carefully refined to a list of
10 signs and symptoms(45). The protocol provides for as-needed benzodiazepines (e.g.
Chlordiazepoxide), as well as vitamins; this is considered standard of care for patients
with unhealthy alcohol use. The use of benzodiazepines may result in a fall in blood
pressure (5%), slowing of the breathing rate (10%), nausea and vomiting, headache,
hiccoughs, or allergic reactions (each less than 5%).
There is a financial risk to participating in the study if problems arise that require
medical attention or hospitalization, and a risk of discovering information during conduct of
the research project that may have an effect on the subject’s later health.
Since this protocol is voluntary, an alternative to participating in the described
protocols is not to participate.
3. Adequacy of protection against risks:
a. Recruitment and informed consent.
i. AUD subjects: The rationale for recruiting subjects from Denver CARES
is based on our group’s experience with subjects from this facility having AUDs, but
infrequent abuse of other substances, making them ideal for the study of alcohol on the
lung. Dr. Burnham has conducted the informed consent process in subjects with AUDs
since 2001, and her colleagues at both UCD and EU will be educated in this process to
ensure uniformity across sites. At Denver CARES, the screening and informed consent
process will be performed by visiting the facility, in person, and interacting with the charge
nurse and staff prior to approaching eligible subjects being discharged from Denver
CARES. This population has been utilized in the past by the PI personally and her
colleagues to successfully recruit research subjects with AUDs with the cooperation of
faculty and staff located at these three sites, and there have been no safety concerns.
Potential subjects from each site will have a “sober time” determined based on initial
breathalyzer value or blood alcohol level. Once a potential subject has reached his/her
“sober time” staff members at each site will help identify potential subjects that might be
eligible for enrollment by research team members. Subjects not to be screened include:
those on a legal hold, and those who are receiving benzodiazepines for alcohol
withdrawal symptoms (<5% of those screened). When the potentially eligible subject is
identified, the charge nurse or patient care technician, who is also familiar with the
Protocol Template
CF-146, Effective 7/10/11
Page 9
On the Web at http://comirbweb.uchsc.edu
protocol, will introduce the potential subject to the research team member. After being
introduced to the potential subject, the applicant or her designate will then interact with the
potential subject in an environment to ensure confidentiality, and explain the study
verbally, including information regarding its inpatient nature and all procedures involved.
After allowing enough time to answer questions and provide further clarifications, the
subject will sign an informed consent document, and a HIPAA waiver designating what
information can be reviewed by the investigators. Any subject consenting to participate in
research at any site will also have the assent of his or her counselor at Denver CARES.
Informed consent will be confirmed again several hours after an individual has been
observed in the research setting (e.g. CTRC) to confirm understanding of the research
protocol. Participation in this study in no way affects the subject’s discharge from a health
care facility. All consent documents will be reviewed and approved by the appropriate
UCD and local IRBs. Individuals with AUDs might be considered a vulnerable population.
Despite this characteristic, we feel that investigations in this specific group of people are
important in improving their overall state of health, as without such work, they are
disproportionately affected by pulmonary infections with increased morbidity and mortality
compared to people who do not drink alcohol heavily.
ii. Control Subjects: Smoking control subjects will be recruited from the
Denver VAMC smoking cessation clinics. Smoking cessation nurse practitioners will
introduce the research team member to the clinic attendees. After describing the
research protocol, interested subjects may provide contact information to the team
member, who will then contact them by telephone to conduct the screening process. If an
individual meets inclusion criteria and agrees to participate, he or she will be scheduled
for a visit in the appropriate CTRC to complete the screening protocol and sign the
informed consent document. Additional control subjects (smoking and non-smoking) will
be recruited from the UCD campuses, and outpatient clinics. Advertisements regarding
research protocols will be posted on the internet and university billboards. The screening
and informed consent process will be performed as described above, and testing
conducted in the CTRC or similar research setting.
b. Protections against risk.
i. Minimizing risks of sample collection: The majority of research samples
will be collected by research coordinators/personnel who are extremely familiar with
performing research sampling. Some blood sampling will be performed by bedside
nurses with extensive phlebotomy experience. Bronchoscopies will always be performed
by physicians (MDs) who have been specially trained in this procedure. Dr. Burnham has
performed over 500 bronchoscopies in her medical career, and over 150 in subjects with
alcohol use disorders for research purposes. Moreover, she has performed at least 150
bronchoscopies in critically ill patients as part of her clinical experience as an ICU
attending. Drs. Moss and Vandivier have similarly performed hundreds of bronchoscopies
on both ambulatory and critically ill patients. All bronchoscopic procedures and conscious
sedation will be administered in a controlled setting in an environment where such
procedures are routine. Telemetric monitoring and intravenous access are absolutely
required for bronchoscopy. Potential subjects deemed too medically unstable by either
the primary attending physician or research personnel for this procedure will not be
enrolled. As we have been conducting protocols for many years in individuals with a
history of AUDs, healthy controls, and critically ill patients, and have had no significant
adverse events related to research sampling, the risk for a research subject to require
additional medical care as a result of research protocols is believed to be low.
Protocol Template
CF-146, Effective 7/10/11
Page 10
On the Web at http://comirbweb.uchsc.edu
Physical or psychological risk from the study protocol will be addressed in a timely
fashion. Subjects may decline to participate at any point in the research protocol. If new
medical problems are discovered at any point in the research protocol, they will be
disclosed to the participant, their proxy for health care, and their primary medical
caregiver. If these issues are considered to increase the risk to the participant
substantially, the protocol will not be completed with the subject, and he or she will be
released from participation. Any potentially serious adverse event (SAE) will immediately
be brought to the attention of the principal investigator so that the event may be
addressed appropriately. Depending on the nature of the event, the study protocol may
be stopped for a given individual, and medical care provided at the university where
research is being performed as indicated by the situation. The CTRC has full capabilities
for monitoring. Therefore, if an SAE in fact occurs, it can be addressed in a seamless
fashion. All potential SAEs will be reported to a data safety and monitor associated with
this study. The institutional review board for the university will be apprised of potential
SAEs as well, and the NIH will be informed about SAEs if deemed appropriate by either
the data safety monitor or the university’s IRB.
ii. Minimizing risks of divulging private healthcare information: Clinical data
collected by research team members may include individually identifiable private
information about human subjects at their particular sites. Using HIPAA language, we will
inform all research participants that information we collect will be used only for research,
and not shared with others. The PI and lead co-investigators at each site will have access
to PHI. However, this information will remain confidential, and case report forms with this
information will be stored in a locked file cabinet in a locked office. Any information,
recorded in any form, relating to an individual’s past, present, or future physical or mental
health or the payment for such health care will remain anonymous, and will not be able to
be linked to the subject from research databases constructed for this proposal. In the
data utilized by investigators, subjects will be referred to by an assigned code number
instead of a name to ensure confidentiality. Data will be stored on a secure server under
the direction of Ms. Monica McNulty, the data manager/analyst.
Federal regulations require that all subjects and controls enrolled in research
protocols be told the extent to which their personally identifiable private information will be
held in confidence. Compliance with the Health Insurance Portability and Accountability
Act of 1996 (HIPAA) will be maintained for all studies conducted within this protocol,
specifically in regard to protecting research data. All patient information will remain
confidential. A Certificate of Confidentiality will be obtained prior to enrolling subjects with
AUDs to ensure that their substance abuse issues will remain confidential. During the
consent process, potential subjects will be asked for their permission to (1) store samples
at the University of Colorado (2) share their samples and de-identified information with
other institutions. The subject providing the sample will provide approval for their
continued storage and use for the purposes of research. If a subject wants his or her
sample discarded, this will be done with the subject’s written request. The subject will be
given a phone number to call if he or she wants his or her specimens destroyed. The
same process applies to storage of samples and clinical data for controls.
Collected samples designated for storage will be de-identified of personal health
information and catalogued using Freezerworks Unlimited (FUL)® software ver 4.0
(Mountlake Terrace, WA) to streamline sample inventory management. This software
Protocol Template
CF-146, Effective 7/10/11
Page 11
On the Web at http://comirbweb.uchsc.edu
meets FDA and GLP regulatory requirements (including 21 CFR Part 11), and creates an
audit trail to track all submission and distribution of specimens along with data entry.
E. Potential Scientific Problems:
Data and samples from this project will evolve to become a biorepository that may be
useful to others in the lung research community and beyond. Therefore, proper
management of the biorepository’s materials by the PI and her colleagues will be needed
to maintain its integrity. We have established a data and sample sharing committee
(DSSC) to safeguard the scientific integrity of research performed with data and samples
from the biorepository, and to ensure the ethical use of subject samples and data for
research unrelated to its original intent. The DSSC will be comprised of the lead PI, Dr.
Burnham, all site PIs, safety officer Jim Maloney, MD, and Monica McNulty, BS, data
manager.
Initial sample and data distribution to participating sites will be determined during the
first meeting of the PI and DSSC members, and will be prioritized based on the following
factors:
Availability of required samples/data and their ease of acquisition
Quantity and type of samples/data needed
Timeframe that investigator(s) request to receive samples/data
Study design of proposed experiments with samples/data
Funding available to requesting investigator(s) to conduct project
At this first meeting, the DSSC will determine if existing IRB protocol modifications are
necessary for on-going sample/data collection to meet consortium needs. Any changes
will be implemented expeditiously by our experienced research coordinator, Meredith
Mealer, RN, along with regulatory experts at other participating sites. Material transfer
agreements (MTAs) between UCD and the EU/LUMC sites are in place, and will be
required and maintained prior to data and sample sharing with any consortium site. Once
requests are approved by the DSSC, a Data Access Group on the REDCaps site will be
created consisting of approved consortium investigators to allow them direct access to
project-related data.
We have established a mechanism to process new requests for samples and data.
Requests will be submitted in a standardized format to the DSSC by consortium
investigators. All requests will be reviewed and discussed by the DSSC during their
regular teleconferences, and need for clarifications or revisions will be directed to the
project’s PI. After approval, a Data Access Group will be created for the necessary
investigators.
Relevant to SA 1: Multiple investigators will require AMs for the experiments
described, and will utilize different experimental techniques. Given the populations
available for recruitment at each site, this consortium has the capability to increase the
number of enrolled AUD subjects and controls based on the needs of its users. Moreover,
we have expert bioresource consultants who will assist us in developing appropriate
processing/storage techniques for AMs so that multiple experiments can be performed on
a single subject’s sample to optimize its scientific yield.
Relevant to SA 2: Smoking is expected to influence our outcome variables for the
described experiments; therefore, careful pair-matching of AUD subjects and controls on
smoking history will be necessary. Additionally, we will have samples from sizable
numbers of non-smoking subjects, and can stratify our analyses to explore outcome
variables in these individuals. TLR-2 expression on human BAECs may not differ by
Protocol Template
CF-146, Effective 7/10/11
Page 12
On the Web at http://comirbweb.uchsc.edu
AUDs. To address this, we have developed methods to measure other molecules
important in pathogen recognition on these cells, including TLR-4 and mannose-binding
lectin. If MAA protein adduct concentration does not differ across our subject types by
AUD and smoking, we have the capability of examining other ELF protein adducts, such
as 4-hydroxy-2-nonenal.
Relevant to SA 3: We based our sample sizes to examine microbiota differences on
prior human investigations; however it is possible that a larger number of subjects may be
required to detect differences in microbiota. Moreover, expanding the examination of
microbiota in patients with burn injury, stratified by AUD history, could further improve our
ability to detect differences and enhance their clinical relevance. We may discover that
multiple antimicrobial proteins/peptides are affected by AUDs in the ELF. Additional
experiments with varying combinations of antimicrobial proteins, as well as experiments in
conjunction with AMs, will help determine the relative importance of these effectors.
F. Data Analysis Plan:
All subject clinical and laboratory data will be entered into a REDCap database created for
our resource. Data generated through the conduct of these investigations will include
clinical data and laboratory data. The REDCap data management system (ver. 3.0), is
available at no cost from Vanderbilt University (see http://project-redcap.org) and is
installed and utilized at the Colorado Clinical and Translational Sciences Institute (CCTSI)
at UCD. UCD has full-time information technology support available through the CCTSI to
assist with the design and management of projects through REDCap. As a CCTSI
member, this assistance is free to Dr. Burnham. Our data manager will initially create a
secure, HIPAA-compliant study database after first creating a data dictionary with clinical
and laboratory elements. REDCap can easily remove personal health information data
elements to create de-identified data sets for study statisticians and others with login
access to the consortium’s site. Once a data dictionary is created, it will be possible for
research coordinators and investigators involved with the consortium’s studies to enter
subject data in real time. The PI and data manager will control the data elements, data
validation, data display, data export, and user export rights. All data generated from
subject samples in the laboratories at University of Colorado and participating sites will
also be entered into the REDCap database by research associates with the approval and
oversight of the data manager. All sites within the consortium will be able to securely
access data within the database via the internet. REDCap has a data logging feature to
track and log any changes in the dataset and by whom they were made. REDCap meets
all HIPAA Security provisions, including single-user logons, complete data entry, edit, and
deletion audit trails that records user names and date/time stamps for all actions. The
database will reside in a restricted directory on a central university server. Access to this
directory will be limited to personnel performing data entry, or analysis of data. All files on
university servers are backed up daily, weekly, and monthly with backup tapes stored at a
remote site that limits the possibility of data loss. To minimize the potential for personal
health information disclosure, records will be identified by a unique study identifier that is
distinct from medical record numbers. UCD has a sophisticated security system that
allows maximal access while not compromising system integrity. It is completely
monitored and has extensive back up to prevent loss of data or unauthorized data
manipulation.
Ms. McNulty, Dr. Burnham, and other consortium members have experience and
training in straightforward statistical analyses. Moreover, both Ms. McNulty and Dr.
Burnham are CCTSI members and will seek biostatistical support prior to finalizing
protocols and data collection and analysis for the consortium. Specific attention will be
Protocol Template
CF-146, Effective 7/10/11
Page 13
On the Web at http://comirbweb.uchsc.edu
paid to the potential effect of confounders including smoking history, age, and gender;
oversight by individuals with additional biostatistical expertise will be integral to ensuring
the validity of the analyses. Additionally, biostatistical support is available at all external
consortium sites to assist investigators on-site. While we will attempt to use samples and
data from each subject enrolled for multiple experiments both at UCD and elsewhere, the
amount of sample obtained from each subject is limited, and not all planned experiments
will be possible with a single subject’s specimens. Additionally, due to the nature of
bronchoscopic sampling, the amount of sample collected from each subject can vary. For
example, the number of cells collected from subject A’s BAL might be 10 million, whereas
in subject B they might be 5 million. Reasons for this include differences in subject
anatomy, differences in subject tolerance of the procedure, and differences in operator
technique. While we will attempt to standardize procedures as much as possible, it will be
impossible to completely remove these differences.
Power and sample size analyses for projects to be completed in the next two years at
the UCD sites have been completed.
SA 1b [EU/UCD Project]: Analyses for this project are based on prior experiments
examining the thiol glutathione (GSH), and its oxidized form, GSSG, in ELF from human
subjects with AUDs and smoking-matched controls. In these prior investigations, we
identified that the percentage of total glutathione present in its oxidized form (GSSG) was
significantly elevated in subjects with AUDs. Since reduced glutathione (GSH) is
quantitatively the most important pulmonary antioxidant, our findings suggested alcohol
influenced thiol homeostasis within the lung, leading to an abnormally oxidized
intrapulmonary milieu in those who consume alcohol heavily. We anticipate that
differences in cysteine/cystine homeostasis (more specifically, differences in %CySS
between those with AUDs and controls) between our AUD subjects and controls for the
thiols cystine and cysteine will be similar in magnitude to what we have observed for
GSH/GSSG. Therefore, we will base our power and sample size analysis on previous
measurements of %GSSG, the percentage of glutathione in ELF present in its oxidized
form, to circumvent issues with dilution of glutathione/GSSG in ELF that are inherent to
bronchoscopic collection. (%GSSG= {[GSSG]/[GSSG+GSH]} x 100). In a sample size of
30 subjects with AUDs, %GSSG was 58.5±28, and in 9 controls was 36.4±26 (p<0.05).
Given that the difference in the means of the two groups (AUD versus controls, 2 sample
means test) was 23, using a pooled standard deviation of 28, an alpha of 0.05, and power
of 0.8, we estimate that we would need to examine 24 subjects with AUDs and 24
smoking matched controls to perceive a significant difference in cystine/cysteine
homeostasis (e.g. differences in the %CySS).
SA 3a [UCD Project 3]: For this aim, we have proposed to assess additional
antimicrobial proteins, including cathelicidin and SLP, in ELF, and hypothesize that their
values will be significantly lower in subjects with AUDs. Analyses for this project are based
on prior experiments examining ELF antimicrobial proteins in subjects with AUDs and
smoking-matched controls. Lysozyme activity in ELF from 6 control subjects was 104±79
(AUs), while in 15 AUD subjects it was 27±26 (AUs), a significant difference. Using a
mean difference of 77 (AUD subjects versus controls, 2 sample means test), with a pooled
SD of 46, an alpha of 0.05 and a power of 0.9, we would need to enroll approximately 18
subjects total, or 9 in each group, to perceive significant differences in the mean value. A
different antimicrobial protein in ELF, lactoferrin, was also measured to be 2.1±1.4ug/mL
in 6 control subjects, and 0.7±0.57ug/mL in 13 subjects with AUDs, a significant
difference. Using the mean difference of 1.4, with a pooled SD of 0.90, an alpha of 0.05
and a power of 0.9, we would need to enroll approximately 20 subjects total, or 10 in each
group, to perceive significant differences in antimicrobial proteins. Therefore, we estimate
Protocol Template
CF-146, Effective 7/10/11
Page 14
On the Web at http://comirbweb.uchsc.edu
that we would need approximately 10 subjects with AUDs and 10 smoking-matched
control subjects, to perceive significant differences in antimicrobial proteins between
groups.
We will also determine the effect of different concentrations of BAL protein from
individual subjects and controls to kill S. pneumoniae in an in vitro killing assay. In short,
we will compare the number of colony-forming units (CFUs) that are able to grow in
culture in the presence of BAL protein at differing concentrations to the number of CFUs
that grow in its absence. To calculate the “percent kill” of S. pneumoniae by the subjects’
or controls’ BAL protein, the following equation will be used: {[CFUs with bacteria
only − (CFUs with bacteria + BAL fluid)]/CFUs with bacteria only} × 100. We will assess
the relationship between acellular BAL fluid protein concentrations and percent kill of S.
pneumoniae (i.e. the pneumococcus) using a mixed effect model to account for correlation
between repeated observations from each subject. This will be necessary as we will be
examining the effect of different concentrations of BAL protein on bacterial killing from the
same subject. The model will be fit separately for AUD and control groups. We have
used this method previously with assistance from the Department of Biostatistics at
UCD(46).
G. Summarize Knowledge to be Gained:
The knowledge gained from this research proposal is important in improving the health of
individuals with AUDs. It will specifically contribute to the body of knowledge related to
why such individuals are predisposed to developing pneumonia and complications
associated with this, including higher morbidity and mortality. It will potentially affect the
care of thousands of individuals who are admitted to hospitals every year with a history of
an AUD to decrease both the risk and the severity of pulmonary infections. The risks of
the proposal’s protocols, including procedural risks and risks of potential drug side effects,
are minimal in relationship to the benefit of developing new therapies for these vulnerable
individuals.
H. References:
Reference List
1. Fiore,A.E., Shay,D.K., Broder,K., Iskander,J.K., Uyeki,T.M., Mootrey,G.,
Bresee,J.S., and Cox,N.S. 2008. Prevention and control of influenza:
recommendations of the Advisory Committee on Immunization Practices (ACIP),
2008. MMWR Recomm. Rep. 57:1-60.
2. Niederman,M.S. 2009. Community-acquired pneumonia: the U.S. perspective.
Semin. Respir. Crit Care Med. 30:179-188.
3. Goss,C.H., Rubenfeld,G.D., Park,D.R., Sherbin,V.L., Goodman,M.S., and Root,R.K.
2003. Cost and incidence of social comorbidities in low-risk patients with communityacquired pneumonia admitted to a public hospital. Chest 124:2148-2155.
4. Saitz,R., Ghali,W.A., and Moskowitz,M.A. 1997. The impact of alcohol-related
diagnoses on pneumonia outcomes. Arch. Intern. Med. 157:1446-1452.
5. Fernandez-Sola,J., Junque,A., Estruch,R., Monforte,R., Torres,A., and UrbanoMarquez,A. 1995. High alcohol intake as a risk and prognostic factor for communityacquired pneumonia. Arch. Intern. Med. 155:1649-1654.
Protocol Template
CF-146, Effective 7/10/11
Page 15
On the Web at http://comirbweb.uchsc.edu
6. Perlino,C.A., and Rimland,D. 1985. Alcoholism, leukopenia, and pneumococcal
sepsis. Am. Rev. Respir. Dis. 132:757-760.
7. Gacouin,A., Legay,F., Camus,C., Volatron,A.C., Barbarot,N., Donnio,P.Y.,
Thomas,R., and Le,T.Y. 2008. At-risk drinkers are at higher risk to acquire a
bacterial infection during an intensive care unit stay than abstinent or moderate
drinkers. Crit Care Med. 36:1735-1741.
8. Zaridze,D., Brennan,P., Boreham,J., Boroda,A., Karpov,R., Lazarev,A.,
Konobeevskaya,I., Igitov,V., Terechova,T., Boffetta,P. et al 2009. Alcohol and
cause-specific mortality in Russia: a retrospective case-control study of 48,557 adult
deaths. Lancet 373:2201-2214.
9. Tonnesen,H., and Kehlet,H. 1999. Preoperative alcoholism and postoperative
morbidity. Br. J. Surg. 86:869-874.
10. Joshi,P.C., and Guidot,D.M. 2007. The alcoholic lung: epidemiology,
pathophysiology, and potential therapies. Am. J. Physiol Lung Cell Mol. Physiol
292:L813-L823.
11. Silver,G.M., Albright,J.M., Schermer,C.R., Halerz,M., Conrad,P., Ackerman,P.D.,
Lau,L., Emanuele,M.A., Kovacs,E.J., and Gamelli,R.L. 2008. Adverse clinical
outcomes associated with elevated blood alcohol levels at the time of burn injury. J.
Burn Care Res. 29:784-789.
12. Kung,H.C., Hoyert,D.L., Xu,J., and Murphy,S.L. 2008. Deaths: final data for 2005.
Natl. Vital Stat. Rep. 56:1-120.
13.
1993. Reduction in alcohol-related traffic fatalities--United States, 1990-1992.
MMWR Morb. Mortal. Wkly. Rep. 42:905-909.
14. Steinberg,W., and Tenner,S. 1994. Acute pancreatitis. N. Engl. J. Med. 330:11981210.
15. Elliott,M.K., Sisson,J.H., and Wyatt,T.A. 2007. Effects of cigarette smoke and
alcohol on ciliated tracheal epithelium and inflammatory cell recruitment. Am. J.
Respir. Cell Mol. Biol. 36:452-459.
16. Sisson,J.H. 2007. Alcohol and airways function in health and disease. Alcohol
41:293-307.
17. Dyson,A., and Singer,M. 2009. Animal models of sepsis: why does preclinical
efficacy fail to translate to the clinical setting? Crit Care Med. 37:S30-S37.
18. Gordon,S. 2003. Alternative activation of macrophages. Nat. Rev. Immunol. 3:23-35.
19. Martinez,F.O., Helming,L., and Gordon,S. 2009. Alternative activation of
macrophages: an immunologic functional perspective. Annu. Rev. Immunol. 27:451483.
Protocol Template
CF-146, Effective 7/10/11
Page 16
On the Web at http://comirbweb.uchsc.edu
20. Joshi,P.C., Mehta,A., Jabber,W.S., Fan,X., and Guidot,D.M. 2009. Zinc deficiency
mediates alcohol-induced alveolar epithelial and macrophage dysfunction in rats.
Am. J. Respir. Cell Mol. Biol. 41:207-216.
21. Moss,M., Guidot,D.M., Wong-Lambertina,M., Ten,H.T., Perez,R.L., and Brown,L.A.
2000. The effects of chronic alcohol abuse on pulmonary glutathione homeostasis.
Am. J. Respir. Crit Care Med. 161:414-419.
22. Yeh,M.Y., Burnham,E.L., Moss,M., and Brown,L.A. 2007. Chronic alcoholism alters
systemic and pulmonary glutathione redox status. Am. J. Respir. Crit Care Med.
176:270-276.
23. Iyer,S.S., Jones,D.P., Brigham,K.L., and Rojas,M. 2009. Oxidation of plasma
cysteine/cystine redox state in endotoxin-induced lung injury. Am. J. Respir. Cell
Mol. Biol. 40:90-98.
24. Jones,D.P., Go,Y.M., Anderson,C.L., Ziegler,T.R., Kinkade,J.M., Jr., and Kirlin,W.G.
2004. Cysteine/cystine couple is a newly recognized node in the circuitry for biologic
redox signaling and control. FASEB J. 18:1246-1248.
25. Yeh,M.Y., Burnham,E.L., Moss,M., and Brown,L.A. 2008. Non-invasive evaluation of
pulmonary glutathione in the exhaled breath condensate of otherwise healthy
alcoholics. Respir. Med. 102:248-255.
26. Bailey,K.L., Sisson,J.H., Romberger,D.J., Robinson,J.E., and Wyatt,T.A. 2010.
Alcohol up-regulates TLR2 through a NO/cGMP dependent pathway. Alcohol Clin.
Exp. Res. 34:51-56.
27. Song,K., Coleman,R.A., Zhu,X., Alber,C., Ballas,Z.K., Waldschmidt,T.J., and
Cook,R.T. 2002. Chronic ethanol consumption by mice results in activated splenic T
cells. J. Leukoc. Biol. 72:1109-1116.
28. Wyatt,T.A., Kharbanda,K.K., Tuma,D.J., Sisson,J.H., and Spurzem,J.R. 2005.
Malondialdehyde-acetaldehyde adducts decrease bronchial epithelial wound repair.
Alcohol 36:31-40.
29. Wyatt,T.A., Slager,R.E., DeVasure,J., Auvermann,B.W., Mulhern,M.L., Von,E.S.,
Mathisen,T., Floreani,A.A., and Romberger,D.J. 2007. Feedlot dust stimulation of
interleukin-6 and -8 requires protein kinase Cepsilon in human bronchial epithelial
cells. Am. J. Physiol Lung Cell Mol. Physiol 293:L1163-L1170.
30. Nelson,S., and Kolls,J.K. 2002. Alcohol, host defence and society. Nat. Rev.
Immunol. 2:205-209.
31. Travis,S.M., Singh,P.K., and Welsh,M.J. 2001. Antimicrobial peptides and proteins in
the innate defense of the airway surface. Curr. Opin. Immunol. 13:89-95.
32. Diamond,G., Beckloff,N., Weinberg,A., and Kisich,K.O. 2009. The roles of
antimicrobial peptides in innate host defense. Curr. Pharm. Des 15:2377-2392.
Protocol Template
CF-146, Effective 7/10/11
Page 17
On the Web at http://comirbweb.uchsc.edu
33. Brecher,A.S., Riley,C., and Basista,M.H. 1995. Acetaldehyde-modified lysozyme
function: its potential implication in the promotion of infection in alcoholics. Alcohol
12:169-172.
34. MacKinnon,A.C., Farnworth,S.L., Hodkinson,P.S., Henderson,N.C., Atkinson,K.M.,
Leffler,H., Nilsson,U.J., Haslett,C., Forbes,S.J., and Sethi,T. 2008. Regulation of
alternative macrophage activation by galectin-3. J. Immunol. 180:2650-2658.
35. Nair,M.G., Cochrane,D.W., and Allen,J.E. 2003. Macrophages in chronic type 2
inflammation have a novel phenotype characterized by the abundant expression of
Ym1 and Fizz1 that can be partly replicated in vitro. Immunol. Lett. 85:173-180.
36. Bailey,K.L., Wyatt,T.A., Romberger,D.J., and Sisson,J.H. 2009. Alcohol functionally
upregulates Toll-like receptor 2 in airway epithelial cells. Alcohol Clin. Exp. Res.
33:499-504.
37. Sisson,J.H., May,K., and Wyatt,T.A. 1999. Nitric oxide-dependent ethanol
stimulation of ciliary motility is linked to cAMP-dependent protein kinase (PKA)
activation in bovine bronchial epithelium. Alcohol Clin. Exp. Res. 23:1528-1533.
38. Sisson,J.H. 1995. Ethanol stimulates apparent nitric oxide-dependent ciliary beat
frequency in bovine airway epithelial cells. Am. J. Physiol 268:L596-L600.
39. Xu,D., Thiele,G.M., Kearley,M.L., Haugen,M.D., Klassen,L.W., Sorrell,M.F., and
Tuma,D.J. 1997. Epitope characterization of malondialdehyde-acetaldehyde adducts
using an enzyme-linked immunosorbent assay. Chem. Res. Toxicol. 10:978-986.
40. Keylock,C.J. 2005. Simpson diversity and the Shannon-Wiener index as special cases of a
generalized entropy. 203-207.
41. Hughes,J.B., Hellmann,J.J., Ricketts,T.H., and Bohannan,B.J. 2001. Counting the
uncountable: statistical approaches to estimating microbial diversity. Appl. Environ.
Microbiol. 67:4399-4406.
42. White,J.R., Nagarajan,N., and Pop,M. 2009. Statistical methods for detecting
differentially abundant features in clinical metagenomic samples. PLoS. Comput.
Biol. 5:e1000352.
43. Lozupone,C.A., Hamady,M., Kelley,S.T., and Knight,R. 2007. Quantitative and
qualitative beta diversity measures lead to different insights into factors that structure
microbial communities. Appl. Environ. Microbiol. 73:1576-1585.
44. Fasching,C.E., Grossman,T., Corthesy,B., Plaut,A.G., Weiser,J.N., and Janoff,E.N.
2007. Impact of the molecular form of immunoglobulin A on functional activity in
defense against Streptococcus pneumoniae. Infect. Immun. 75:1801-1810.
45. Sullivan,J.T., Sykora,K., Schneiderman,J., Naranjo,C.A., and Sellers,E.M. 1989.
Assessment of alcohol withdrawal: the revised clinical institute withdrawal
assessment for alcohol scale (CIWA-Ar). Br. J. Addict. 84:1353-1357.
Protocol Template
CF-146, Effective 7/10/11
Page 18
On the Web at http://comirbweb.uchsc.edu
46. Burnham,E.L., Gaydos,J., Hess,E., House,R., and Cooper,J. 2010. Alcohol use
disorders affect antimicrobial proteins and anti-pneumococcal activity in epithelial
lining fluid obtained via bronchoalveolar lavage. Alcohol Alcohol 45:414-421.
Protocol Template
CF-146, Effective 7/10/11
Page 19