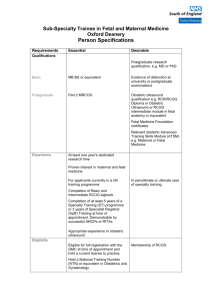
oxford deanery subspecialist training in fetal and maternal medicine
advertisement

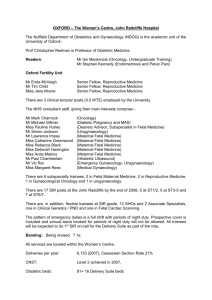
OXFORD DEANERY SUBSPECIALIST TRAINING IN FETAL AND MATERNAL MEDICINE The Fetal and Maternal Medicine Subspecialist Training Programme The Fetal and Maternal Medicine Subspecialist training programme is a two year programme, starting at a minimum of ST6 level. During this time, the trainee's work will be monitored for satisfactory progress and subject to annual reviews in the form of both ARCPs and a mid-term and final review, organised by the RCOG. Progression on the programme will be dependent upon these reviews. Essential Information Title of Post Grade Duration Specialty Base Hospital District Renumeration Consultant Supervisor District College Tutor Work Pattern Reason for Vacancy Sub Specialist Trainee in Fetal and Maternal Medicine Specialty Registrar year 6/7 2 years Obstetrics and Gynaecology John Radcliffe Hospital Oxford according to previous experience Mr Lawrence Impey Mrs Rebecca Black EWTD compliant band 1A rota Replacement SST post This post is governed by the Medical and Dental Terms and Conditions of Service Career Counselling Career advice and guidance should be sought, in the first instance, from your Educational Supervisor, who will normally be a Consultant with whom you work. Some, but not all, Units will appoint a medically qualified and trained counsellor who will contact you directly. Career problems may be discussed with your Unit Clinical Tutor and/or your Postgraduate Dean. Useful Names Postgraduate Dean Consultant Supervisor Medical Personnel Officer Dr Michael Bannon Mr Lawrence Impey Mrs Julie Gray The Department The Department of Obstetrics and Gynaecology at present provides a maternity and gynaecology service to the Oxford region. This is an approved training centre for the Subspecialty of Fetal and Maternal Medicine directed by Mr Lawrence Impey. The centre is approved by the RCOG for two posts. The successful applicant will share an office, have their own PC and access to secretarial services. The John Radcliffe Hospital is a busy teaching and district general hospital and a regional referral centre, responsible for over 7000 deliveries per year. A large number of referrals from within the unit and from the region are made to the fetal and maternal medicine services. It has close links to the Nuffield Department of Obstetrics and Gynaecology. Women’s Health is one of the themes of Oxford’s BRC (Biomedical Research Centre), a scheme funded through a large grant awarded in 2007 from the NIHR. The appointee will be based in the Feto-Maternal Medicine Unit. This manages a wide range of obstetric, medical and fetal problems. Maternal medicine is led by two obstetricians, Miss Harrington and Miss Greenwood, and an Obstetric Physician, Miss Lucy Mackillop. Fetal medicine is led by Mr Impey, Mrs Black and Miss Greenwood. There are two medical complications in pregnancy clinics and two fetal medicine outpatient clinics, a miscarriage/ early pregnancy clinic, a preterm labour clinic, a placental screening (incl uterine arteries) clinic and a cervical screening clinic. In addition there are daily outpatient ultrasound/prenatal diagnosis clinics run by Dr Chamberlain, Mr Impey, Miss Greenwood, Miss Harrington, Miss Hurley and Mrs Black. The diabetic service is currently run by Miss Harrington and Dr Mackillop. Rhesus disease is managed by the Oxford Rhesus Therapy Unit, led by Miss Hurley. The fetal cardiology service is run by Dr Archer (Paediatric cardiologist) and Dr Manning (Associate Specialist in Obstetric Ultrasound). The Ultrasound Department performs over 21000 scans per year. Supportive services are provided by the Cytogenetic and DNA laboratories at the Churchill Hospital and the Institute of Molecular Medicine at the Oxford site. There is a large Regional Neonatal Intensive Care Unit with 8 Consultant Neonatal Paediatricians. The Unit works closely with the High Risk Pregnancy Service. There is a regional Perinatal Pathology Service within the Women’s Centre run by Dr S Gould, Consultant Pathologist. The National Perinatal Epidemiology Unit is based at the Churchill site. The Delivery Suite is supported by a team of Consultant Obstetric Anaesthetists, led by Dr Robin Russell. Neonatologists, obstetric anaesthetists and junior and middle grade obstetricians are available at all times. All obstetric consultants maintain an active Delivery Suite role. Duties of the Post This is a two year training programme covering all aspects of fetal and maternal medicine. The appointee will be exposed to sufficient clinical experience to enable them to meet the clinical criteria to complete subspecialty training in maternal fetal medicine. With short attachments to the Genetics Department, Neonatal Unit and Obstetric Anaesthesia, there are regular sessions in the Fetal Medicine Unit, Prenatal Diagnosis, High Risk Pregnancy / Silver Star Unit, Oxford Rhesus Therapy Unit and for recurrent miscarriage and labour management. The post involves a full time on call commitment, currently as part of a 9-cell rota which involves one weekend set of daytime duties and one set of weekend night duties per 9-week cycle. There is enough flexibility within the unit to be able to accommodate the learning and training needs of the successful applicant. The exact timetable will be designed following discussion and agreement with the trainee and the Programme Director, Mr Lawrence Impey, and will be subject to review. Teaching Teaching of undergraduates and postgraduates is an essential part of the normal commitments in this teaching district. The post holder will be expected to take an active role in the teaching of medical students and junior medical staff. Administration The organisation and running of perinatal morbidity and mortality meetings. Responsibility for collecting and analysing annual fetal medicine unit and occasionally obstetric statistics Formulating, under appropriate supervision, guidelines for obstetric high risk and fetal medicine patients. Research The Fetal and Maternal Medicine RCOG Subspecialty Training Programme does not include a dedicated research year. This should have been performed prior to appointment, with either two first author publications in Medline peer-reviewed journals, or a higher research degree such as Ph D or MD. However, there will be the opportunity for research projects during the programme. Trust Information Information about the John Radcliffe Hospital, part of the Oxford University Hospitals NHS Trust, can be found on the hospital’s website www.ouh.nhs.uk Information about the Nuffield Department of Obstetrics and Gynaecology can be found at www.obs-gyn.ac.uk Department members The staffing of the Department, together with their special interest are listed below: Nuffield Department of Obstetrics and Gynaecology Professor Stephen Kennedy Head of Department Special interests include endometriosis, subfertility and pelvic pain Dr Paul Chamberlain Senior Lecturer Ultrasound, Prenatal Diagnosis Mr Enda McVeigh Senior Fellow, Reproductive medicine Mr Tim Child Senior Fellow, Reproductive medicine IVF, PCOS, recurrent miscarriage Miss Jane Moore Senior Fellow, Reproductive medicine IVF, pelvic pain, undergraduate teaching Mr Christian Becker Senior Lecturer Endometriosis Mr Ahmed Ahmed Senior Lecturer Gynaecological Oncology Prof Chris Redman Professor of Obstetric Medicine NHS Staffing Mr Vic Rai Mr Simon Jackson Miss Natalia Price Miss Lee Lim Miss Maryam Pezeshki Lead for Gynae Risk Management Urogynaecology Urogynaecology and obstetrics Obstetrics and gynaecology, infertility (locum) Obstetrics and gynaecology (locum) Miss Pauline Hurley Miss Catherine Greenwood Mrs Rebecca Black Mr Lawrence Impey Miss Debbie Harrington Fetal Medicine, Rhesus Disease Maternal Fetal Medicine, Labour Ward Lead Maternal Fetal Medicine, District College Tutor Fetal Medicine Lead Maternal Medicine Lead Dr Lucy Mackillop Obstetric Physician Associate Specialist:Dr Nicky Manning Fetal Cardiology Clinical Lecturers:Miss Katy Vincent Dr Karin Hellner Subspecialty Trainees:Miss Ingrid Granne Mr Peter Yeh Miss Brenda Kelly Mr Pathi Pathiraja Mr Philip Rahmanou Reproductive Medicine Maternal Fetal Medicine Maternal Fetal Medicine Gynaecological Oncology Urogynaecology Middle grade trainees: ST 3-5: ST 6/7: 6 trainees, core training (including one Academic Clinical Fellow) 6 trainees, allocated to ATSMs Junior trainees ST1/2 FTSTAs GP VTS FY2 6 trainees 1 trainee 3 as part of Oxford VTS rotation 3 for 4 month attachment Main Conditions of Service Appointments to this programme are subject to the Terms and Conditions of Service (TCS) for Hospital Medical and Dental Staff (England and Wales). In addition appointments are subject to: Applicants having the right to work and be a doctor or dentist in training in the UK Registration with the General Medical Council Pre-employment checks carried out by the Trust HR department in line with the NHS employment check standards, including CRB checks and occupational health clearance. The employing Trust’s offer of employment is expected to be on the following nationally agreed terms: Hours – The working hours for junior doctors in training are now 48-hours (or 52hours if working on a derogated rota) averaged over 26 weeks (six months). Doctors in training also have an individual right to opt-out if they choose to do so, but they cannot opt-out of rest break or leave requirements. However, the contracts for doctors in training make clear that overall hours must not exceed 56 hours in a week (New Deal Contract requirements) across all their employments and any locum work they do. http://www.nhsemployers.org/PlanningYourWorkforce/MedicalWorkforce/EWT D/Pages/EWTD.aspx Pay – you should be paid monthly at the rates set out in the national terms and conditions of service for hospital medical and dental staff and doctors in public health medicine and the community health service (England and Wales), “the TCS”, as amended from time to time. The payscales are reviewed annually. Current rates of pay may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircular sMedicalandDental.aspx Part time posts will be paid pro-rata Pay supplement –depending upon the working pattern and hours of duty you are contracted to undertake by the employer you should be paid a monthly additional pay supplement at the rates set out in paragraph 22 of the TCS. The current payscales may be viewed at http://www.nhsemployers.org/PayAndContracts/Pay%20circulars/Pages/PayCircular sMedicalandDental.aspx . The pay supplement is not reckonable for NHS pension purposes. The pay supplement will be determined by the employer and should be made clear in their offer of employment and subject to monitoring. Pension – you will be entitled to join or continue as a member of the NHS Pension Scheme, subject to its terms and rules, which may be amended from time to time. If you leave the programme for out of programme experience you may have a gap in your pension contributions. More information can be found at http://www.nhsbsa.nhs.uk/pensions Annual Leave – your entitlement to annual leave will be five or six weeks per annum depending on your previous service/incremental point, as set out in paragraphs 205206 of the TCS. The TCS may be viewed at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTS GPREG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx Sick pay – entitlements are outlined in paragraph 225 of the TCS. Notice –you will be required to give your employer and entitled to receive from them notice in accordance with paragraphs 195-196 of the TCS. Study Leave –the employer is expected to offer study leave in accordance with paragraphs 250-254 of the TCS. Local policy and procedure will be explained at induction. Travel Expenses – the employer is expected to offer travel expenses in accordance with paragraphs 277-308 of the TCS for journeys incurred in performing your duties. Local policy and procedure should be explained at induction. Subsistence expenses – the employer is expected to offer subsistence expenses in accordance with paragraph 311 of the TCS. Local policy and procedure should be explained at induction. Relocation expenses – the employer will have a local policy for relocation expenses based on paragraphs 314 – 315 of the TCS and national guidance at http://www.nhsemployers.org/PAYANDCONTRACTS/JUNIORDOCTORSDENTISTS GPREG/Pages/DoctorsInTraining-JuniorDoctorsTermsAndConditions150908.aspx. You are advised to check eligibility and confirm any entitlement with the employer before incurring any expenditure. Pre-employment checks – all NHS employers are required to undertake preemployment checks. The employer will confirm their local arrangements, which are expected to be in line with national guidance at http://www.nhsemployers.org/RecruitmentAndRetention/Employmentchecks/Pages/Employment-checks.aspx Professional registration – it will be a requirement of employment that you have professional registration with the GMC/GDC for the duration of your employment. Though the post is covered by NHS Indemnity, you are strongly advised to register with the MPS for professional indemnity. Health and Safety – all employers have a duty to protect their workers from harm. You should be advised by the employer of local policies and procedures intended to protect your health and safety and expected to comply with these. Disciplinary and grievance procedures – the employer will have local policies and procedures for dealing with any disciplinary concerns or grievances you may have. They should advise you how to access these, not later than eight weeks after commencement of employment. Educational Supervisor – the employer or a nominated deputy (usually the Director of Medical Education) will confirm your supervisor on commencement. General information on the Deanery’s management of Specialty Training programmes, including issues such as taking time out of programme and dealing with concerns or complaints, is available at www.oxforddeanery.nhs.uk and in the national ‘Gold guide’ to Specialty Training at http://www.mmc.nhs.uk Please ensure that you inform Oxford Deanery of any changes to your contact details.