Concussion Injuries: These injuries should be reported to the
advertisement

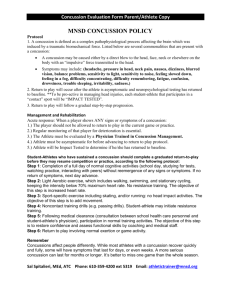
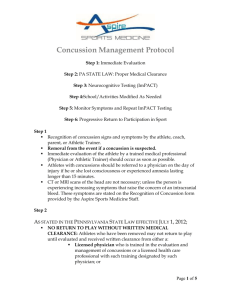
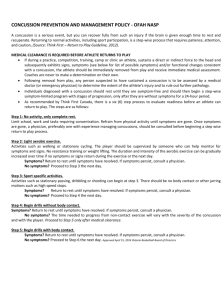
Concussion Injuries: These injuries should be reported to the athletic training staff immediately. The Athletic Training Staff/Team Physicians utilize the following guidelines from the, American Academy of Neurology and the National Athletic Trainers’ Association Position Statement: Management of Sport Related Concussion when evaluating concussions. Return to competition is at the discretion of the evaluating ATC/Team Physician. GRADES OF CONCUSSION: Grade 1: 1. Transient confusion (inattention, inability to maintain a coherent stream of thought and carry out goal-directed movements) 2. No loss of consciousness 3. Concussion symptoms or mental status abnormalities on examination resolve in less than 20 minutes Grade 1 concussion is the most common yet the most difficult to recognize. The athlete is not rendered unconscious and suffers only momentary confusion (e.g., inattention, poor concentration, inability to process information or sequence tasks) or mental status alterations. Grade 2: 1. Transient confusion 2. No loss of consciousness 3. Concussion symptoms or mental status abnormalities (including amnesia) on examination last more than 20 minutes Grade 2 concussion, the athlete is not rendered unconscious but experiences symptoms or exhibits signs of concussion or mental status abnormalities on examination that last longer than 20 minutes (e.g., poor concentration or post-traumatic amnesia). Grade 3 1. Any loss of consciousness, either brief (seconds) or prolonged (minutes). Grade 3 concussion is usually easy to recognize if the athlete is unconscious for any period of time. Concussion Evaluation Procedures: 1. Student-Athletes participating in contact/collision sports will be pre-tested prior to the start of their season. This baseline testing will include the Standardized Assessment of Concussion (SAC) and Balance Error Scoring System (BESS) evaluations. Follow-up SAC and BESS scores will be used during the recovery process to provide the most reliable measure of pre-injury performance. 2. At the time of injury, ATC’s will also use a Graded Symptom Checklist (GSC) to determine the extent of the student-athlete’s symptoms. The GSC will also be used during the recovery process. 3. Student-athletes participating in non-contact sports will not be pre-tested. At the time of injury, ATC’s and/or Team Physicians will still utilize the SAC, BESS, and GSC after injury to monitor progress and help determine return to play decisions. The SAC, BESS, and GSC can be found in: Appendix A Concussion Management Recommandations: Grade 1 1. Remove from contest. 2. Examine immediately and at 5-minute intervals for the development of mental status abnormalities or post-concussive symptoms at rest and with exertion. 3. May return to contest if mental status abnormalities or post-concussive symptoms clear within 20 minutes. 4. A second Grade 1 concussion in the same contest eliminates the player from competition that day. Once symptom free, the athlete will be reassessed using the SAC, BESS and GSC evaluations, as well as cardiovascular activities. The athlete can be released to full participation as long as no recurrent signs and symptoms are present. Grade 2 1. 2. 3. 4. Remove from contest and disallow return that day. Examine on-site frequently for signs of evolving intracranial pathology. A trained person should reexamine the student-athlete the following day. A physician should perform a neurological examination to clear the Student-Athlete for return to play if symptoms persist for longer then one full week at either rest or with exertion. 5. CT or MRI scanning is also recommended in all instances where headache or other associated symptoms worsen or persist longer than one week. 6. Following a second Grade 2 concussion, return to play should be deferred until the studentathlete is symptom free at rest and with exertion and reassessed using the SAC, BESS, and GSC evaluations. This process could take two weeks or longer. 7. Terminating the season for that player is mandated by any abnormality on CT or MRI scan consistent with brain swelling, contusion, or other intracranial pathology. Grade 3 1. Transport the student-athlete from the field to the nearest emergency department by ambulance if still unconscious or if worrisome signs are detected (with cervical spine immobilization, if indicated). 2. A thorough neurological evaluation should be performed emergently, including appropriate neuro-imaging procedures when indicated. 3. Hospital admission is indicated if any signs of pathology are detected, or if the mental status of the athlete remains abnormal. 4. ** Following a second Grade 3 concussion, the student-athlete should be withheld from play until an evaluation by a Neurologist. The return to play decision will then be determined upon clinical evaluation by the neurologist and team physician. ** Once again, this is the decision of the evaluating Team Physician/Neurologist When To Return To Play: Once the student athletes’ concussion symptoms are gone, the grade of the concussion can be determined. At that point, the Team Physician or Athletic Trainer will decide if the studentathlete can return to play. Grade I concussions, the student-athlete may return to physical activity if asymptotic, under the discretion of the Sports Medicine Staff. If symptoms persist or worsen the student-athlete will be sent to see the Team MD. The student-athlete will be given a head injury sheet, in all cases, by the athletic trainer, which should be followed by the student-athlete. Also the athletic trainer must inform parent/roommate or whomever the student-athlete is staying with of this sheet. If the student-athlete suffers a grade II or a second concussion of any degree in one season, the student-athlete will be sent to the Team MD. If the student-athlete suffers any loss of consciousness, he/she will be referred to the Team MD. Once the student-athlete is sent to the Team MD, the student-athlete must be cleared by that evaluating Physician for physical activity. In cases of severe concussions the student-athlete will be sent to the emergency room immediately.