View
advertisement
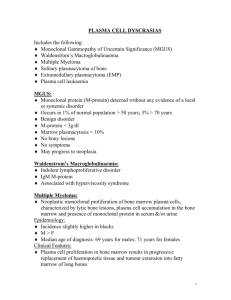
MULTIPLE MYELOMA Pathophysiology Male predominant, African Americans, average age 68 at diagnosis. Risk factors: toxins, heredity Immature B cells differentiate into plasma cells which secrete immunoglobulins. Chromosomal alteration in plasma cells leads to monoclonal proliferation of myeloma cells (IgG>A, usually heavy chains, 20% light chain, rarely nonsecretory). Myeloma cells have low growth potential and are initially dependent on bone marrow environment for survival=Bone- CA interaction. They can later become stromaindependent and have extramedullary spread=Malignant Melanoma. In the initial phases, M cells bind to marrow cells which produce cytokines for Mcell growth and survival. Cytokines include OAFs, which damage the marrow by increasing resorption and decreasing bone formation, allowing M cell growth, and other cytokines which impair immune function. Clinical Presentation reflects presence of plasma cells in bone and Ig in serum/urine Bone: hypercalcemia in 30%, osteoporosis, lytic lesions (pain, fracture) due to increased osteoclasts. Not apparent on bone scan as process is destruction not formation. Renal: 25%, impairment due to hypercalcemia /dehydration, or direct toxicity of light chains; see increased creatnine and proteinuria. Often cause of death. Hematologic: anemia of chronic disease/CRI in 80%, hyperviscosity in IgA disease, abnormal platelet function Infection: due to decrease in other circulating Ig, decreased APC function by cytokines. Typically gm negative/polysaccharide encapsulated organisms. Cause of death. Extramedullary: metastatic myeloma can go to pleura, blood, skin Spectrum of Disease/Subtypes MGUS: probably precursor to MM- first chromosomal hit causes MGUS, second causes transformation to MM (transformation in 16% over about 10 years). Dx=hypergammaglobulinemia (monoclonal, IgG or A usually) with <10% plasma cells in marrow, no features of myeloma. Smoldering: not quite myeloma, monoclonal gammopathy with abnormal marrow cells Multiple Myeloma: 1 major and 1 minor criteria, or 3 minor criteria in patient with symptoms and progressive (bone) disease Other: plasma cell leukemia (>5x10^9 plasma cells in peripheral blood), solitary plasmacytoma (solid tumor of monoclonal plasma cells on pathology), POEMS (bone sclerosis, demyelinating neuropathy, HSM, endocrinopathy, skin disease) Diagnosis Plasma cells in marrow, monoclonal Ig protein peripherally Criteria: Major- plasmacytoma, >30% plasma cells in marrow, monoclonal protein (IgG>3.5, IgA>2, or Bence Jones proteins >1 g/24 hour) Minor- lytic lesions, monoclonal hypergammaglobulinemia with others hypo, 10-30% plasmacytosis marrow Evaluation Laboratory: CBC, Calcium, Creatnine, 24hour urine protein (or ratio), LDH, U.A., CRP/ESR, beta2microglobulin (LMW protein HLA light chain, renally excreted) Immunoglobulins in urine or serum Peripheral smear Immunoglobulin levels (one predominates), kappa to lambda ration Immunofixation- monoclonal spike in paraprotein. Serum: IgG 53%, IgA20%, k/l Immunofixation of urine: light chain disease- 20% bence jones proteins Bone evaluation: BMAspirate/bx- plasma cells, cytogenetics Skeletal survey BMD Staging Stage 1- low tumor mass (Hb>10, IgG<5, IgA<3, BJ<4g, normal calcium, <2 lytic bone) Stage 2- int. tumor mass Stage 3- high tumor mass (any: Hb<8.5, IgG>7, IgA>5, BJ>12g, Ca>12, multiple lytic) Subclass by renal function (A if creatnine less than 2, B if greater) Prognosis: poor if higher burden of tumor- LDH, UA, anemia, hypercalcemia, Beta2microglobulin, also if older, cytogenetics, extramedullary, increase CRP/ESR (cytokines) Treatment Supportive: radiotherapy to fracture, RRT, analgesia, hypercalcemia, Epo, infection px Bisphosphonates: Supportive for bone disease (improved QOL), possibly directly therapeutic. Indication= osteopenia, lytic lesion, fracture. Mechanism of action: inhibit osteoclast function by decreasing recruitment/ inhibiting maturation, also decrease IL production (OAF)- leads to decreased pain, fracture, and preservation of bone structure/integrity. Rx Clodronate 2400 mg/day, or monthly IV Pamidronate/Zolendronate. Duration uncertain, adjunct to chemotherapy as well. Chemotherapy: Goal is remission (IF negative at 6 weeks, <5% plasmacytosis, no evidence dz progression). Median survival with conventional chemo 2-3 years, increased to 50% 5 year survival with high dose chemo and BMT. Drug resistance high. Alkylating agents: Melphalan alone CR30%, Melph/Pred is standard. Combination chemo (VAD or CVAMP) 3-5 cycles induces remission faster but not more effective. Induce with combination chemo, then HIGH DOSE MELPHALAN myeloablation with rescue autotransplantation of peripheral stem cells leads to 30-50% CR, 81% OR, 50% 5 year survival. OS is 6-9 years, in 21%. Tandem autotxp has 42%OS. Thalidomide if relapse. Biologic/immunologic: Interleukins; PEG IFN toxic, 4 mos increased survival; Steroids to maintain remission also with side effects, Monoclonal Ab to B cells, Allogeneic transplant high mortality.