Name Dr Bartley Cryan
advertisement
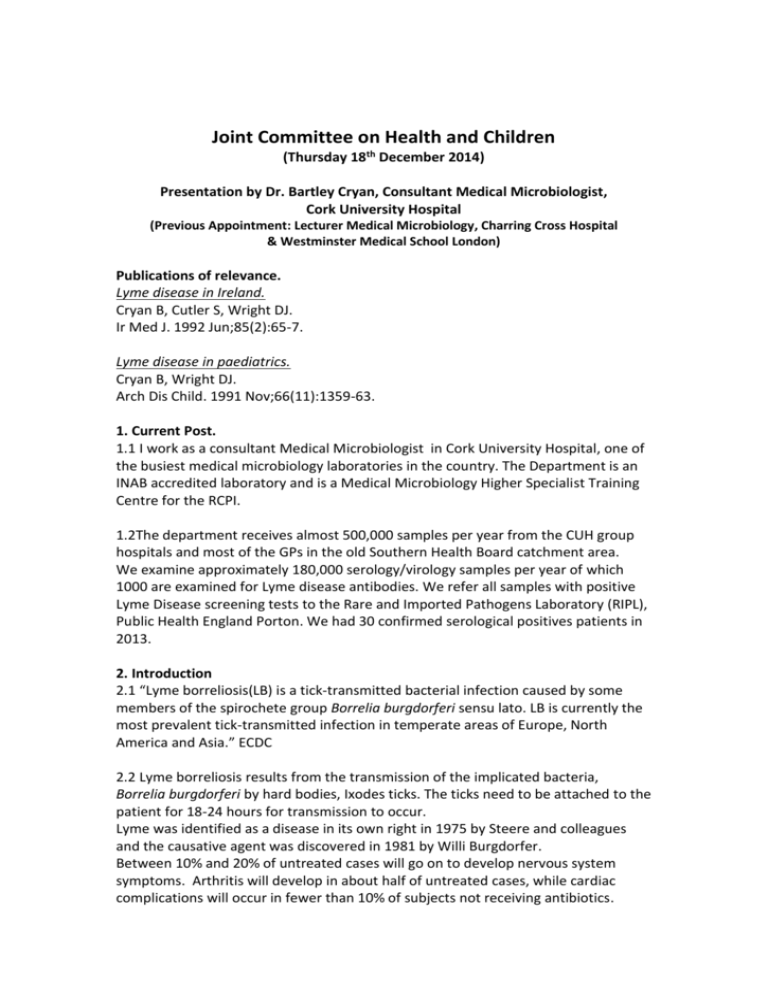
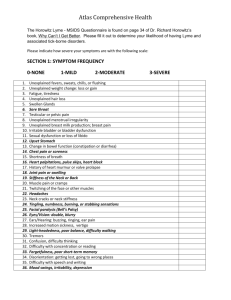
Joint Committee on Health and Children (Thursday 18th December 2014) Presentation by Dr. Bartley Cryan, Consultant Medical Microbiologist, Cork University Hospital (Previous Appointment: Lecturer Medical Microbiology, Charring Cross Hospital & Westminster Medical School London) Publications of relevance. Lyme disease in Ireland. Cryan B, Cutler S, Wright DJ. Ir Med J. 1992 Jun;85(2):65-7. Lyme disease in paediatrics. Cryan B, Wright DJ. Arch Dis Child. 1991 Nov;66(11):1359-63. 1. Current Post. 1.1 I work as a consultant Medical Microbiologist in Cork University Hospital, one of the busiest medical microbiology laboratories in the country. The Department is an INAB accredited laboratory and is a Medical Microbiology Higher Specialist Training Centre for the RCPI. 1.2The department receives almost 500,000 samples per year from the CUH group hospitals and most of the GPs in the old Southern Health Board catchment area. We examine approximately 180,000 serology/virology samples per year of which 1000 are examined for Lyme disease antibodies. We refer all samples with positive Lyme Disease screening tests to the Rare and Imported Pathogens Laboratory (RIPL), Public Health England Porton. We had 30 confirmed serological positives patients in 2013. 2. Introduction 2.1 “Lyme borreliosis(LB) is a tick-transmitted bacterial infection caused by some members of the spirochete group Borrelia burgdorferi sensu lato. LB is currently the most prevalent tick-transmitted infection in temperate areas of Europe, North America and Asia.” ECDC 2.2 Lyme borreliosis results from the transmission of the implicated bacteria, Borrelia burgdorferi by hard bodies, Ixodes ticks. The ticks need to be attached to the patient for 18-24 hours for transmission to occur. Lyme was identified as a disease in its own right in 1975 by Steere and colleagues and the causative agent was discovered in 1981 by Willi Burgdorfer. Between 10% and 20% of untreated cases will go on to develop nervous system symptoms. Arthritis will develop in about half of untreated cases, while cardiac complications will occur in fewer than 10% of subjects not receiving antibiotics. Cases contracted in North America tend to be more severe in every sense than those contracted in Europe. 2.3 Since January 2012, Lyme disease has been mandatorily notifiable in Ireland as the entity ‘neuroborreliosis’ 2.4 A vaccine for Lyme disease was introduced in 1998, but it has since been withdrawn by the manufacturer due to controversies over alleged side effects. 3. Clinical Diagnosis of Lyme borreliosis 3.1 Traditionally, infections are provisionally diagnosed by eliciting clinical signs and symptoms characteristic to the illness and the diagnosis is then confirmed by detecting or growing the implicated microorganism from the infected tissue . 3.2 Unfortunately Borrelia burgdorferi, the causative organism of Lyme Disease is very difficult to grow or detect by molecular or other methods. In such cases evidence of infection is inferred by the presence of antibodies or activated cells. Such serological methods have inherent problems, It takes time to develop a response There may be cross reactions/false positive results Presence of antibody implies previous exposure to the organism, it does not necessarily confirm that the patients clinical symptoms are caused by B. burgdorferi. Antibodies remain positive after treatment. 3.4 The earliest, clinical manifestation of Lyme borelliosis is the pathognomonic erythema migrans, a circular erythematous rash spreading peripherally from the central site of a tick bite. This is seen in 70-80% of infections and develops between 3 and 32 days following a tick bite. Serology can be negative in up to 30% of patients with erythema migrans, later samples will be positive and confirm the diagnosis. 3.5 Other features of early Lyme Disease include, flu-like symptoms such as headache, sore throat, neck stiffness, fever, muscle aches and general fatigue. 3.6 Occasionally, there may be more serious symptoms involving the nervous system, joints, the heart or other tissues. 4. Diagnostic strategy 4.1 We follow the testing guidelines recommended by the US Centre for Disease Control & Infectious Diseases Society of America and the UK Health Protection Agency which recommend a two tire testing protocol. This system is also the one currently most recommended by European authorities. 4.2 The first required test is the Enzyme Immunoassay (EIA) if this is negative an alternative diagnosis should be considered. However bearing in mind that the antibody response takes several weeks to reach a detectable level if the patients symptoms are present for less than 30 days a repeat sample may be considered. 4.3 For positive results a confirmatory western blot should be performed. We refer all our positive EIA assays to the RIPL for confirmatory Western Blots, results are usual available within 3 weeks. 4.4 While awaiting the Western Blot results the doctor looking after the patient is contacted by the laboratory medical staff and the implications of the screening test result are reviewed in the light of the patient’s clinical condition. 4.5 Once the confirmed positive result is available the case is again discussed with the clinician and consideration may be given to the possibility of further tests such as Lyme EIA of cerebrospinal fluid in cases of potential neurological Lyme disease or joint fluid in the case of arthritis. 4.6 Of the 1000 samples examined for Lyme antibodies in 2013 only 30 were confirmed positive. Samples are submitted throughout the year with a peak in late summer. 4.7 While not formally recorded, patients predominantly receive their tick bites in Ireland with some in the US or Europe. 4.8 While the collation of laboratory results with recognized Lyme Disease syndromes can give rise to a confident diagnosis the usefulness of serology in reactivation or post Lyme syndrome is less beneficial as such patients have pre existing antibodies to B. burgdorferii and reliable tests for such conditions need to be developed. Bartley Cryan 16. Dec. 2014 MC Reg 003789