File - Respiratory Therapy Files
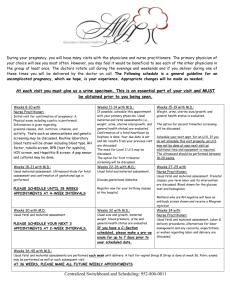
advertisement

Infant of a Diabetic Mother (IDM) Background: Diabetes has long been associated with maternal and perinatal morbidity and mortality. Before the discovery of insulin in 1921, diabetic women rarely reached reproductive age or survived pregnancy. In fact, pregnancy termination was recommended routinely for pregnant diabetic patients because of high mortality rates. Fetal and neonatal mortality rates were as high as 65% before the development of specialized maternal, fetal, and neonatal care. Since then, infants of diabetic mothers (IDMs) have experienced a nearly 30-fold decrease in morbidity and mortality rates. Today, 3-10% of pregnancies are affected by abnormal glucose regulation and control. Of these, 80% are related to abnormal glucose control of pregnancy or gestational diabetes mellitus. Infants born to mothers with glucose intolerance are at an increased risk of morbidity and mortality related to the following: Respiratory distress Growth abnormalities (large for gestational age [LGA], small for gestational age [SGA]) Hyperviscosity secondary to polycythemia Hypoglycemia Congenital malformations Hypocalcemia, hypomagnesemia, and iron abnormalities These infants are likely to be born by cesarean section for many reasons, among which are such complications as shoulder dystocia with potential brachial plexus injury related to the infant's large size. It is important for these mothers to be monitored closely throughout pregnancy. If optimal care is provided, the perinatal mortality rate, excluding congenital malformations, is nearly equivalent to that observed in normal pregnancies. Pathophysiology: It is necessary to understand the physiology of fetal glucose control to appreciate the causes of the associated complications. Increased levels of both estrogen and progesterone affect glucose homeostasis as counter-regulatory hormones in the mother early in pregnancy. As a result, beta-cell hyperplasia occurs in the pancreas, stimulating an increased release of insulin. Increased insulin levels stimulate glycogen deposition and decrease hepatic glucose production. It is not uncommon to recognize a decreased need for insulin in the diabetic patient in early pregnancy. Furthermore, amino acids decrease and fatty acid triglycerides and ketones both increase with increased fatty acid deposition. As a result, increased protein catabolism and accelerated renal gluconeogenesis occurs. As pregnancy progresses, human placental lactogen is released by the syncytiotrophoblast, leading to lipolysis in the mother. The subsequent release of glycerol and fatty acids reduces maternal use of glucose and amino acid, thus preserving these substrates for the fetus. The release of increasing amounts of contrainsulin factors as placental growth continues causes up to a 30% increase in maternal insulin needs as pregnancy progresses. Mothers with previous borderline glucose control, obesity, or frank diabetes may require initiation of or increase in their insulin requirements to maintain glucose homeostasis. Glucose and amino acids traverse the placental membrane. On the other hand, insulin is unable to cross from maternal to fetal circulations. Using a carrier-mediated facilitated diffusion mechanism, fetal glucose levels are maintained at a level that is 20-30 mg/dL lower than those of the mother. The fetus is subjected to high levels of glucose during times of maternal hyperglycemia. Before 20 weeks' gestation, fetal islet cells are incapable of responding, subjecting the fetus to unchecked hyperglycemia and decreased fetal growth. Poor growth is especially noted in mothers with diabetic vascular disease. After 20 weeks' gestation, the fetus responds to hyperglycemia with pancreatic beta-cell hyperplasia and increased insulin levels. Proinsulin (insulinlike growth factor-1 [IGF-1], insulinlike growth factor–binding protein-3 [IGFBP-3]) also acts as a growth factor that, in the presence of increased fetal amino acids, results in fetal macrosomia. Fetal growth acceleration can be noted on ultrasound by 24 weeks' gestation, especially with fluctuating maternal glucose levels. The combination of hyperglycemia and insulin increases fat and glycogen stores, resulting in weight increases marked by hepatosplenomegaly and cardiomegaly without an increase in head circumference. Chronic fetal hyperglycemia and hyperinsulinemia increase the fetal basal metabolic rate and oxygen consumption, leading to a relative hypoxic state. The fetus responds by increasing oxygen-carrying capacity through increased erythropoieten production, possibly leading to polycythemia. The fetus redistributes iron from developing organs, including the heart and brain, to support this expanded blood mass, leaving these organs iron deficient and with possible long-term functional consequences. Prior to birth, elevated insulin levels may inhibit the maturational effect of cortisol on the lung, including the production of surfactant from type 2 pneumocytes. This puts the fetus at risk for developing respiratory distress syndrome after birth. Frequency: In the US: The 1988 National Maternal and Infant Health Survey reported that diabetes complicated 4% of pregnancies resulting in live births. Of these, 88% were the result of gestational diabetes mellitus, 8% were the result of non–insulin-dependent diabetes, and 4% were from insulin-dependent diabetes mellitus. Given recent estimates of 0.2-0.3% of pregnancies complicated by preexisting diabetes and a further 1-5% complicated by gestational diabetes mellitus, approximately 50,000-150,000 infants are born to diabetic mothers every year. Internationally: Women of Asian, Indian, or Middle-Eastern descent are at a higher risk than the general population. Mortality/Morbidity: Birth defects in infants of diabetic mothers have risen from 1-2% to 8-15% as a consequence of increased perinatal survival. Major congenital malformations are found in 5-9% of affected infants and account for 30-50% of perinatal deaths of infants of mothers with gestational diabetes. In mothers with insulin-dependent diabetes, the stillbirth and perinatal mortality rate is 5 times the rate in the general population, and neonatal and infant mortality rates are 15 and 3 times the rate in the general population, respectively. These infants are 3 times more likely to be born by cesarean delivery, twice as likely to suffer serious birth injury, and 4 times as likely to be admitted to a neonatal intensive care unit. Major causes of morbidity include the following: o LGA or SGA infants o Hypoglycemia o Prematurity o Respiratory distress syndrome o Intrapartum asphyxia Race: Incidence is higher in Latinos and African-Americans than in whites. Diabetes occurs more frequently in persons of American Indian descent, particularly among the Pimas of the southwestern United States. Sex: Frequency of involvement in boy and girl IDMs is equal. Age: Generally, the first 1-3 hours after birth are the most critical for the development of hypoglycemia. History: Fetal congenital malformations are most common when maternal glucose control has been poor during the first trimester of pregnancy. Given that many pregnancies are unplanned, the need for preconceptional glycemic control in diabetic women cannot be overstated. Maternal hyperglycemia during late gestation is more likely to lead to fetal macrosomia, neonatal electrolyte abnormalities, or cardiomegaly with outflow tract obstruction. Fetal macrosomia o Quality of fetal growth is determined by plotting birthweight against gestational age on standard growth curves. Infants whose weight exceeds the 90th percentile for gestational age are classified as large for gestational age. Maternal hyperglycemia during late pregnancy is commonly followed by excessive fetal growth. o LGA infants should be routinely screened for potential hypoglycemia. This is particularly important if the mother has received large amounts of glucose-containing fluids during her labor. o Fetal macrosomia is observed in 26% of IDMs and in 10% (by definition) of infants of nondiabetic women. While most common as a consequence of maternal hyperglycemia and hyperinsulinemia, fetal macrosomia may occur despite maternal euglycemia. Impaired fetal growth o o Infants whose birthweight is below the 10th percentile, when plotted against gestational age on a standard growth curve, are considered small for gestational age. Impaired fetal growth may occur in as many as 20% of diabetic pregnancies, compared to a 10% incidence (by definition) for infants born to nondiabetic mothers. Maternal renovascular disease is the common cause of impaired fetal growth in pregnancies complicated by maternal diabetes. Pulmonary disease o These infants are at an increased risk of respiratory distress syndrome and may present within the first few hours after birth with tachypnea, nasal or intercostal retractions, and hypoxia. Operative delivery due to macrosomia also increases the risk for transient tachypnea of the newborn, while polycythemia predisposes the infant for persistent pulmonary hypertension of the newborn. o Initially, the differential diagnosis might include transient tachypnea of the newborn, respiratory distress syndrome, pneumonia, or persistent pulmonary hypertension. Metabolic and electrolyte abnormalities o Hypoglycemia may present within the first few hours of life, with such symptoms as jitteriness, irritability, apathy, poor feeding, high pitched or weak cry, hypotonia, or frank seizure activity. This hypoglycemia may persist for as long as one week. More commonly, the neonate is asymptomatic. o Hypoglycemia is caused by hyperinsulinemia due to hyperplasia of fetal pancreatic beta cells consequent to maternal-fetal hyperglycemia. Because the continuous supply of glucose is stopped after birth, the neonate develops hypoglycemia because of insufficient substrate. Stimulation of fetal insulin release by maternal hyperglycemia during labor significantly increases the risk of early hypoglycemia in these infants. Perinatal stress may have an additive effect on hypoglycemia due to catecholamine release and glycogen depletion. o The overall risk of hypoglycemia is anywhere from 25-40%, with LGA and preterm infants at highest risk. o Hypocalcemia or hypomagnesemia also may be apparent in the first few hours after birth; symptoms may include jitteriness or seizure activity. Hypocalcemia (levels <7 mg/dL) is believed to be associated with a delay in parathyroid hormone synthesis after birth. o Sixty-five percent of all IDMs demonstrate abnormalities of iron metabolism at birth. Iron deficiency increases an infant's risk for neurodevelopmental abnormalities. Iron is redistributed to the iron-deficient tissues after birth, as the RBC mass is postnatally broken down. Hematologic problems: Polycythemia, caused by increased erythropoiesis triggered by chronic fetal hypoxia, may present as a clinically "ruddy" appearance, sluggish capillary refill, or respiratory distress. Hyperviscosity due to polycythemia increases the IDM's risk for stroke, seizure, necrotizing enterocolitis, and renal vein thrombosis. Thrombocytopenia: Thrombopoiesis may be inhibited because of an excess of red blood cell precursors within the bone marrow as a result of chronic in utero asphyxia. Hyperbilirubinemia: This is common, especially in association with polycythemia. Excessive red cell hemolysis, caused by vascular sludging, leads to elevated bilirubin levels. Cardiovascular anomalies o o Cardiomyopathy with intraventricular hypertrophy and outflow tract obstruction may occur in as many as 30% of these infants. The cardiomyopathy may be caused by congestive failure with a weakly functioning myocardium or to a hypertrophic myocardium with significant septal hypertrophy and outflow tract obstruction. When cardiomegaly or poor perfusion and hypotension are present, it is important to obtain an echocardiogram to differentiate between these processes. These infants also are at an increased risk of congenital heart defects, including (most commonly) ventricular septal defect (VSD) and transposition of the great arteries (TGA). Congenital malformations Physical: o Central nervous malformations are 16 times more likely in these infants. In particular, the risk of anencephaly is 13 times higher, while the risk of spina bifida is 20 times higher. The risk of caudal dysplasia is up to 600 times higher in these infants. o Renal (eg, hydronephrosis, renal agenesis, ureteral duplication), ear, cardiovascular (eg, single umbilical artery, VSDs, atrial septal defects, TGA, coarctation of the aorta, cardiomegaly), and gastrointestinal (eg, duodenal or anorectal atresia, small left colon syndrome) anomalies are more frequent in these infants. Fetal macrosomia (>90th percentile for gestational age or >4000 g in the term infant) occurs in 1545% of diabetic pregnancies. When present, the infant appears puffy, fat, ruddy, and often mildly limp. Impaired fetal growth, secondary to poor placental blood flow, is a consequence of severe maternal diabetics with diabetic nephropathy. Perinatal asphyxia, more common in such infants, may be anticipated by prenatal history, thus stressing the importance of communication between obstetrician and pediatrician. Causes: HbA1C levels o Complications caused by maternal hyperglycemia during pregnancy are reflected by elevated HbA1C levels, particularly during the first trimester of pregnancy. o Because HbA1C is a direct measure of glucose control in the mother, higher levels are predictive of increased risks for congenital complications. Thus, the incidence of complications has been reported as 3.4% with HbA1C levels lower than 8.5% and 22.4% with levels higher than 8.5%. There is speculation that birth defects in IDMs may be related to reduced arachidonic acid and myoinositol levels and elevated sorbitol and trace metal levels in the fetus. o o Others speculate about the role of excess oxygen radicals and hydroperoxides in the mitochondria of susceptible fetal tissues because these prostacyclin inhibitors may cause disruption in the vascularization of developing tissues. o A past history of LGA infants, diabetes, stillbirth, hypertension, gestational diabetes, obesity, or glycosuria, or a current history of excessive weight gain in the present pregnancy or low socioeconomic class place the mother at an increased risk of poor glucose control during pregnancy and increase her risk of delivering an infant with subsequent complications. Fetal macrosomia o IDMs experience higher levels of glucose during gestation, resulting in pancreatic beta cell hyperplasia with increased secretion of insulin and proinsulin factors (IGF-1, IGFBP3). Amino acid availability also is increased. All of these factors are involved in the excessive growth observed in the infants of diabetic mothers. o All organ systems, aside from the kidney and brain, are sensitive to the increased glucose and amino acid pools. Increased insulin levels result in an increase in cell number and cell size. Impaired fetal growth o The major cause of impaired fetal growth is maternal diabetic nephropathy. Maternal vascular disease compromises uteroplacental blood flow and impairs fetal nutrient supply. o IDMs are at increased risk of preterm labor, stillbirth, neonatal death, birth injury, and perinatal asphyxia. Pulmonary disease o These infants are at increased risk for respiratory distress syndrome, transient tachypnea of the newborn, and persistent pulmonary hypertension. o Insulin restricts substrate availability for surfactant biosynthesis and interferes with the normal timing of glucocorticoid-induced biosynthesis. o Insulin also blocks cortisol action at the fibroblast level by reducing production of fibroblast-pneumocyte factor, which normally would stimulate type II cells to produce surfactant. o Several studies agree that the risk of respiratory distress syndrome in well-managed diabetic women delivered at term is no higher than in the general population. Electrolyte abnormalities o These infants are at high risk for hypoglycemia, especially within the early hours after birth. o High levels of fetal insulin with cessation of continued maternal glucose supply take place after birth. The neonatal shift to gluconeogenesis with fatty acid use may provide an insufficient supply of substrate, and, thus, the infant may experience hypoglycemia (<20-40 mg/dL), which may be asymptomatic. Alternatively, the infant may display such symptoms as jitteriness, irritability, lethargy, poor feeding tolerance, and seizures. With hypoglycemia, the body responds with increased counterregulatory hormones and production of ketones for use as an energy source. With continued hyperinsulinemia, this production of ketones is inhibited, thus lowering the source of energy for these infants even further. o Hypocalcemia, with or without hypomagnesemia, also may be present and is believed to be secondary to parathyroid hormone suppression. o Postnatal parathormone response of IDMs is decreased compared to their gestationally matched controls. The associated hypomagnesemia has been speculated to be secondary to increased urinary losses associated with a more severe diabetic state. This maternal hypomagnesemia is reflected in the fetus also. Cardiovascular anomalies o Cardiac hypertrophy may be observed in as many as 30% of IDMs. o Fetal growth is regulated by insulin binding to cell receptors. Compared to the adult, the fetus has an increased number of receptors. Because the fetal heart is particularly rich in receptors, this may lead to increased myocardial protein, glycogen, and fat synthesis with hyperplasia and hypertrophy of myocardial cells. Congenital malformations o Some speculate that many of the congenital anomalies in IDMs may arise from an insult to the developing somite mesoderm and cephalic neural crest cells. o Metabolic disturbances, such as hyperglycemia, hypoglycemia, hyperketonemia, and hypoxia, also may be involved. o Glucose-induced free radicals of oxygen also have been implicated. These kids have a good prognosis; As many as 50% of mothers with gestational diabetes develop insulindependent diabetes within 15 years of their pregnancy.