T`was that time of year… A review of Canine Acute Pancreatitis
advertisement

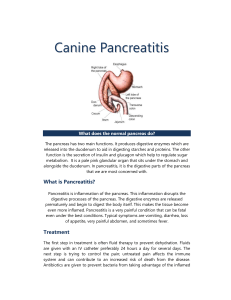
‘Twas that time of year… A Review of Canine Acute Pancreatitis As we all have noted, the last few months have been a time of over indulgence for both ourselves and our patients. Acute pancreatitis in canines is often associated with fatty meals - and so the vomiting, abdominal pain, and anorexia begin. This article aims to review the overall management of acute pancreatitis including available diagnostics, current treatment options, and recent changes in how we approach these cases. 1. cPLI and ultrasound remain the gold standard for diagnosing pancreatitis. 2. Pain and nausea should be treated aggressively. 3. Free choice feeding or tube feeding of a low fat diet is recommended. Food should only be withheld in cases of intractable vomiting and pain. 4. Nutritional support is necessary in cases where anorexia is likely for >3-5 days. Enteral feeding is preferred over parenteral feeding. 5. Antibiotics are indicated in patients with evidence of severe pancreatitis, sepsis, or systemic inflammatory response syndrome (SIRS). Diagnosing pancreatitis can be tricky and is based on an index of suspicion, as well as laboratory and clinical tests. An overweight dog with a recent history of a fatty meal is considered a classic risk factor for pancreatitis. Other causes of pancreatitis include neoplasia, trauma, and drugs (azothioprine, sulfonamides, tetracycline, and potassium bromide). Amylase and lipase are only 50% sensitive and specific for the disease and so they remain fairly unhelpful in confirming a diagnosis. The newer test, cPLI (immunoreactive canine pancreatic lipase assay) is 90% sensitive for pancreatitis, therefore there are very few false negatives. The in-house SNAP test is valuable in ruling out pancreatitis. Unfortunately, an “abnormal” result means further testing (cPLI and /or ultrasound) is needed to diagnose pancreatitis. Abdominal ultrasound is thought to be between 40-70% sensitive for detecting pancreatitis. In general, using cPLI and ultrasound may be the best way to currently detect pancreatitis. Serial cPLI testing and ultrasounds may also better detect pancreatitis and its progression/resolution. Initial treatment should be focused around correcting fluid deficits, pain control, and antiemetics. The traditional reasoning of “resting” the pancreas by fasting is now considered incorrect. Autodigestion of the pancreas with pancreatitis is more likely caused by intracellular premature activation of protelytic enzymes, not pancreatic stimulation. However, withholding food may help to decrease pain and vomiting; therefore, once this has been addressed feeding should be reinstituted. In addition to correcting fluid deficits caused by vomiting and peritoneal loss, balanced crystalloids are used to improve perfusion of the pancreas. Electrolytes should be monitored, as well as renal output and patient hydration via repeat physical exams, serial weight monitoring, and urine specific gravity. Colloids may also be needed to improve pancreatic perfusion. Opiods (fentanyl CRI 2-5 mcg/kg/hr or repeated doses of morphine or hydromorphone) offer a good start to pain control. Analgesics are indicated in any case of pancreatitis, even if no pain or only mild pain is noted. Adding lidocaine and ketamine as constant rate infusions can also be beneficial with severe pain. Anti-emetics that act peripherally and centrally such as maropitant, ondansetron, or dolansetron are recommended. Metoclopramide only acts centrally to control nausea so it may be less effective. Unfortunately, there is still no consensus on the best way to manage nutrition in cases of pancreatitis in dogs. In 2012, international consensus guidelines for nutritional support were established for people with acute pancreatitis. These guidelines established that enteral nutrition (EN) within 3-4 days is indicated and preferred over parenteral nutrition (PN). In people, if eating is not anticipated within 5-7 days, nutritional therapy should be considered regardless of disease severity. Recent studies also show that post-pyloric placement of feeding tubes is not required, making nasogastric tubes for EN a viable option in human patients. In canine acute pancreatitis, there is very little evidence available. Recent clinical studies have shown similar results to human studies, so the human guidelines may be relevant to our patients as well. A recent study compared early enteral feeding via esophagostomy tube and parenteral nutrition in 10 dogs with severe acute pancreatitis. It showed that pre-pyloric EN was well tolerated. The dogs in the EN group did not show postprandial pain, and had less vomiting and regurgitation than the PN group. Patients should be offered low fat meals frequently and in small amounts. If anorexia is likely past 3 days then enteral feeding via nasoesophageal, esophageal, gastrotomy, or jejunostomy tube should be pursued. Only if enteral feeding is not tolerated, such as in cases with intractable vomiting and pain, should parenteral nutrition (PN) be instituted. PN requires a central IV line and specific compounding which generally limits its use to referral hospitals. Ready-made solutions of amino acids and glucose should only make up 40% of RER and should not be used for more than 3-5 days. Antibiotic usage is recommended for cases of severe pancreatitis, and with evidence of sepsis or SIRS. When antibiotics are indicated, broad-spectrum coverage for aerobes and anerobes is recommended. This can be accomplished with a second-generation cephalosporin (cefoxitin), or a combination of amoxicillin with a fluoroquinolone. Additional therapies, such as plasma transfusions (FFP) or heparin therapy, may be indicated in cases suspected to have disseminated intravascular coagulation. A retrospective paper did not show any benefit with administration of FFP with acute pancreatitis. Mortality rate was higher in dogs that received FFP. This was not associated with disease severity or evidence of SIRS, DIC, or sepsis. Other studies have shown that free radical scavenger administration may ameliorate the severity of pancreatitis. The administration of Vitamin E and S-adenosyl L methionine (SAMe) may be potentially beneficial. The diagnosis and treatment of acute pancreatitis continues to revolve around supportive care and stabilization. Further studies are needed to establish guidelines in veterinary medicine for the optimal treatment of pancreatitis.