Management of Indwelling Pleural Catheter
advertisement

A Policy for the Management of Indwelling Pleural
Catheter
V6.0
September 2015
Summary.
Drainage Procedure – all of the equipment should be found in the dressing pack.
6.1.1. Ensure the patient is comfortable and fully informed about the procedure.
6.1.2. Wash hands.
6.1.3. Open dressing pack and drainage bottle.
6.1.4. Wearing disposable gloves, remove the dressing.
6.1.5. Wash hands
6.1.6. Put on sterile gloves
6.1.7. Clamp drainage bottle.
6.1.8. Remove cover from access tip on drainage bottle.
6.1.9. Remove catheter cap from catheter.
6.1.10. Using sterile alcohol swabs, wipe the end of the catheter.
6.1.11. Insert access tip into catheter until you hear and feel a click.
6.1.12. Release both clamps.
6.1.13. Drain slowly. It is recommended that you limit a single drainage to no more than
1000mls.
6.1.14. Drain fluid until it stops draining. If patient experiences pain, excessive coughing
or
becomes breathless, stop draining. Administer analgesia if required.
6.1.15. Clamp bottle.
6.1.16. Remove drainage line from catheter.
6.1.17. Place sterile cap on the end of the catheter (a new cap each time).
6.1.18. Position the pad around the catheter.
6.1.19. Wind the catheter around the pad.
6.1.20. Cover with gauze
6.1.21. Secure with vapour-permeable adhesive film. Do not apply film directly to the
catheter.
6.1.22. Dispose of all equipment in the appropriate bag for clinical waste. (For
community
patients – arrange for local county council to collect for incineration. Do not cut
off the
green indicator and empty).
Management of Indwelling Pleural Catheter
Page 2 of 11
Table of Contents
1. Introduction................................................................................................................. …
3
2. Purpose of this Policy ................................................................................................ ....
3
3. Scope ........................................................................................................................ ....
3
4. Definitions / Glossary................................................................................................... …
3
5. Ownership and Responsibilities......................................................................................
3
6. Standards and Practice ...................................................................................................
4
7. Dissemination and Implementation..................................................................................
5
8. Monitoring compliance and effectiveness........................................................................
5
9. Updating and Review.......................................................................................................
6
10. Equality and Diversity.....................................................................................................
6
Appendix 1. Governance Information ..................................................................................
7
Appendix 2.Initial Equality Impact Assessment Screening Form.........................................
9
Management of Indwelling Pleural Catheter
Page 3 of 11
1. Introduction
1.1. The indwelling pleural catheter is used for the drainage of a pleural
effusion. The catheter is inserted into the pleural space of patients who have
recurrent pleural effusions or where pleurodesis is not possible.
2. Purpose of this Policy/Procedure
2.1. To provide all staff treating patients who have an indwelling pleural catheter insitu
with the appropriate information, education and training to ensure there is an
understanding of the management of the catheter to –
• Relieve breathlessness
• Stop readmission to hospital for repeated pleural aspirations
• Improve quality of life
• Delivering a cost saving
3. Scope
3.1. This strategy applies to all those involved in service redesign, from Executive level,
through to Divisional Management teams to staff members working directly in clinical
services who are involved in looking at their own service redesign.
3.2. The RCHT lead for overseeing the management of the indwelling pleural drain will
be supported by the Divisional Management Team
4. Definitions / Glossary
5. Ownership and Responsibilities
All members of staff involved in the drainage of pleural fluid using and indwelling pleural
catheter.
5.1. Role of the Managers
Line managers are responsible for ensuring their staff have had the correct training to
carry out the procedure.
5.2. Role of Individual Staff
5.21. All staff members are responsible for ensuring they have read the document and
adhere to the information given.
5.22. Staff should ensure the equipment is sterile and in date.
Management of Indwelling Pleural Catheter
Page 4 of 11
5.23.All staff should be aware of personal limitations. They should declare to a senior
member of staff it they do not feel they are competent to carry out the procedure.
5.24. A standardized approach will be used by all nurses for individual patients. If any
further training is required then the nurse should seek advice from a senior member of
the team.
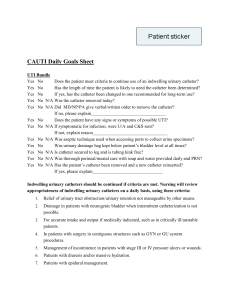
6. Standards and Practice
6.1 Drainage Procedure – all of the equipment should be found in the dressing pack.
6.1.1. Ensure the patient is comfortable and fully informed about the procedure.
6.1.2. Wash hands.
6.1.3. Open dressing pack and drainage bottle.
6.1.4. Wearing disposable gloves, remove the dressing.
6.1.5. Wash hands
6.1.6. Put on sterile gloves
6.1.7. Clamp drainage bottle.
6.1.8. Remove cover from access tip on drainage bottle.
6.1.9. Remove catheter cap from catheter.
6.1.10. Using sterile alcohol swabs, wipe the end of the catheter.
6.1.11. Insert access tip into catheter until you hear and feel a click.
6.1.12. Release both clamps.
6.1.13. Drain slowly. It is recommended that you limit a single drainage to no more than
1000mls.
6.1.14. Drain fluid until it stops draining. If patient experiences pain, excessive coughing or
becomes breathless, stop draining. Administer analgesia if required.
6.1.15. Clamp bottle.
6.1.16. Remove drainage line from catheter.
6.1.17. Place sterile cap on the end of the catheter (a new cap each time).
6.1.18. Position the pad around the catheter.
6.1.19. Wind the catheter around the pad.
6.1.20. Cover with gauze
6.1.21. Secure with vapour-permeable adhesive film. Do not apply film directly to the
catheter.
6.1.22. Dispose of all equipment in the appropriate bag for clinical waste. (For community
patients – arrange for local county council to collect for incineration. Do not cut off the
green indicator and empty).
6.1 Further Recommendations
6.2.1. Indwelling pleural catheters are inserted to drain pleural fluid and relieve
breathlessness, stop re-admission into hospital for repeated pleural aspirations and
improve quality of life.
Management of Indwelling Pleural Catheter
Page 5 of 11
6.2.2. Sutures are to be removed from incision site after 7 days post line insertion.
The sutures around the line itself should be removed 3 weeks post line insertion
6.2.3. Change in colour of pleural fluid: if the pleural fluid were to become cloudy
then take a sample of fluid.
6.2.4. Redness: If redness develops around the line then swab the area, check vital
signs.
6.2.5. If redness increases or patient feels unwell, contact GP, Wellington Ward or Lung
Cancer CNS’s on 01872 252015
6.2.6. Drainage: Catheter to be drained 3 times weekly (for the first 3 weeks). Record
fluid drained on the monitoring sheet.
6.2.7. Generally : patients have their pleural catheter drained 3 times a week for the
first 3 weeks, then twice weekly for a couple of weeks. If pleural fluid continues to
diminish, drainage becomes weekly – fortnightly. If no fluid has been drained on 2 – 3
occasions, contact lung cancer CNS’s for advice about co-ordinating removal. Patients
will need a CXR to confirm pleurodesis and a date will then be given for removal.
6.2.8. If you need advice before changing the drainage regime contact the Lung Cancer
Nurses on 01872 252015 for further instructions.
Useful contact numbersLung cancer CNS Sue Pascoe / Paul Kneller 01872 252015
Wellington Ward (Respiratory) 01872 252100
Crown Hill Ward (Derriford) 0845 1558274
7. Dissemination and Implementation
7.1. This document will be added to the Trust electronic Documents Library.
7.2. All staff who are involved in the care of patients requiring drainage pleural fluid
using an indwelling pleural catheter will be informed of the new policy.
8. Monitoring compliance and effectiveness
Element to be
All staff who are involved in the care of patients requiring
monitored
drainage pleural fluid using an indwelling pleural catheter
Lead
Unit / Line Managers
Tool
Staff training records
Frequency
As required
Reporting
Any incidents regarding the use of the indwelling pleural catheter
arrangements
will be reported on DATIX
Acting on
Recommendations made will be implemented by the various staff
recommendations
groups – Lung Cancer Clinical Nurse Specialists, Ward Manager
and Lead(s)
Wellington Ward.
Change in
Required changes will be identified and actioned within 4 weeks or
practice and
as agreed in the action plan. A lead member of the team will be
lessons to be
identified to take each change forward where appropriate. Lessons
shared
will be shared with all the relevant stakeholders.
9. Updating and Review
9.1. This policy will be reviewed no less than 3 years after issue unless changes
in equipment provision require an earlier review.
10. Equality and Diversity
10.1.This document complies with the Royal Cornwall Hospitals NHS Trust
Management of Indwelling Pleural Catheter
Page 6 of 11
service Equality and Diversity statement.
10.2.Equality Impact Assessment
10.21 The Initial Equality Impact Assessment Screening Form is at Appendix 2.
Management of Indwelling Pleural Catheter
Page 7 of 11
Appendix 1. Governance Information
Document Title
Guidelines on the management of the indwelling
pleural catheter
Date Issued/Approved:
1 September 2015
Date Valid From:
1st September 2015
Date Valid To:
31st August 2018
Directorate / Department
responsible (author/owner):
Sue Pascoe, Lung Cancer Clinical Nurse
Specialist
Contact details:
01872 252015 or bleep 3061
Brief summary of contents
To provide guidance for all staff treating patients
who have an indwelling pleural catheter
Suggested Keywords:
Pleural drain, effusion
Target Audience
RCHT
PCH
CFT
KCCG
Executive Director responsible
for Policy:
Medical Director
Date revised:
1st September 2015
This document replaces (exact
title of previous version):
A Policy for the management of Indwelling
pleural catheter
Approval route (names of
committees)/consultation:
Respiratory Consultants
Divisional Manager confirming
approval processes
Head of relevant Division
Signed copy on file
Name and Post Title of additional
signatories
Not required
Name and Signature of
Divisional/Directorate
Governance Lead confirming
approval by specialty and
divisional management meetings
Signature of Executive Director
giving approval
Publication Location (refer to
Policy on Policies – Approvals
and Ratification):
Document Library Folder/Sub
Folder
Dr John Myers
Name:
{Original Copy Signed}
Internet & Intranet
Respiratory
Management of Indwelling Pleural Catheter
Page 8 of 11
Intranet Only
Links to key external standards
Governance Team can advise
Related Documents:
Reference and Associated documents
Training Need Identified?
Yes, this can be carried out by competent ward
staff
Version Control Table
Date
Version
No
Summary of Changes
10 Jun 10 V1.0
Initial Issue
29 Oct 10 V2.0
Amendment of Governance coversheet to
include ‘Suggested Keywords’, ‘Training
Need’ and ‘Publication Location’.
1 Feb 11
Addition of Monitoring Compliance table.
V3.0
Changes Made by
(Name and Job Title)
Andrew Rogers
Corporate Records
Manager
Andrew Rogers
Corporate Records
Manager
Andrew Rogers
Corporate Records
Manager
Andrew Rogers
Corporate Records
Manager
Andrew Rogers
Corporate Records
Manager
15 Jan 12 V4.0
Governance information moved to an
appendix. EIA updated.
25 Jan 12 V4.1
Governance information amended to align
with format of Document Manager Upload
Form.
20 Sep 12 V5.0
Amended and updated
Sue Pascoe Lung
Cancer CNS
1 Sep 15
Amended and updated
Sue Pascoe Lung
Cancer CNS
V6.0
All or part of this document can be released under the Freedom of Information
Act 2000
This document is to be retained for 10 years from the date of expiry.
This document is only valid on the day of printing
Controlled Document
This document has been created following the Royal Cornwall Hospitals NHS Trust
Policy on Document Production. It should not be altered in any way without the
express permission of the author or their Line Manager.
Management of Indwelling Pleural Catheter
Page 9 of 11
Appendix 2. Initial Equality Impact Assessment Form
Name of Name of the strategy / policy /proposal / service function to be assessed:
Guidelines on the management of the indwelling pleural catheter
Directorate and service area:
Is this a new or existing Policy?
Medicine
Existing
Name of individual completing
Telephone:
assessment: Sue Pascoe
01872 252015 or bleep 3061
1. Policy Aim*
To provide guidance on the management of indwelling pleural
Who is the strategy /
catheters.
policy / proposal /
service function
aimed at?
2. Policy Objectives*
To provide guidance on the management of indwelling pleural
catheters.
3. Policy – intended
Outcomes*
To provide guidance on the management of indwelling pleural
catheters.
4. *How will you
measure the
outcome?
5. Who is intended to
benefit from the
policy?
6a) Is consultation
required with the
workforce, equality
groups, local interest
groups etc. around
this policy?
Correct use of the indwelling catheter.
Relief of breathless and avoid or reduce hospital stay.
b) If yes, have these
*groups been
consulted?
Yes
C). Please list any
groups who have
been consulted about
this procedure.
Nursing staff in Respiratory and Oncology
Patients with a a recurring pleural effusion..
Yes
7. The Impact
Please complete the following table.
Are there concerns that the policy could have differential impact on:
Equality Strands:
Age
Yes
Sex (male, female, trans-
No
√
Rationale for Assessment / Existing Evidence
√
gender / gender
reassignment)
Management of Indwelling Pleural Catheter
Page 10 of 11
Race / Ethnic
communities /groups
√
Disability -
√
Learning disability, physical
disability, sensory impairment
and mental health problems
Religion /
other beliefs
√
Marriage and civil
partnership
√
Pregnancy and maternity
√
Sexual Orientation,
√
Bisexual, Gay, heterosexual,
Lesbian
You will need to continue to a full Equality Impact Assessment if the following have been
highlighted:
You have ticked “Yes” in any column above and
No consultation or evidence of there being consultation- this excludes any policies
which have been identified as not requiring consultation. or
Major service redesign or development
No√
8. Please indicate if a full equality analysis is recommended.
Yes
9. If you are not recommending a Full Impact assessment please explain why.
Signature of policy developer / lead manager / director
Names and signatures of
members carrying out the
Screening Assessment
Date of completion and submission
1.
2.
Keep one copy and send a copy to the Human Rights, Equality and Inclusion Lead,
c/o Royal Cornwall Hospitals NHS Trust, Human Resources Department, Knowledge Spa,
Truro, Cornwall, TR1 3HD
A summary of the results will be published on the Trust’s web site.
Signed _______Sue Pascoe________
Date ___________17/07/2015_____
Management of Indwelling Pleural Catheter
Page 11 of 11