Briedwell-Unit.5-Cardiovascular-System
advertisement

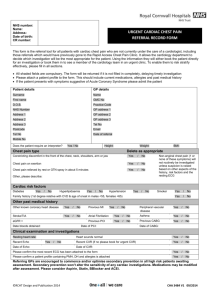
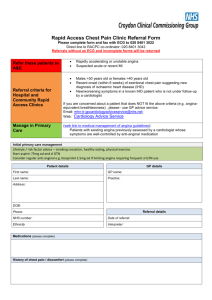
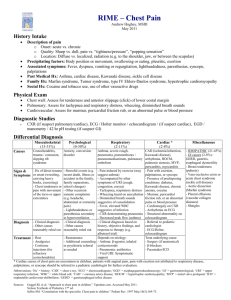
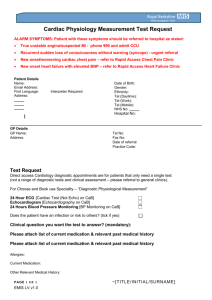
MU PT 7780 – Differential Diagnosis Teresa Briedwell PT, DPT Cardiovascular System Objectives: 1. The student will recognize and screen for signs and symptoms associated with cardiovascular disease. 2. The student will recognize situations requiring immediate medical attention and those that warrant referral relative to the cardiovascular system. 3. The student can discuss the prevalence of cardiovascular disease and the relevance of that to the practice of physical therapy. 4. The student will explain the rule of the three P’s related to likelihood of myocardial infarction. 5. The student will identify appropriate screening tools relative to the cardiovascular system. 6. The student will recognize normal and abnormal vital signs and utilize such information to screen and monitor patients. 7. The student will utilize the Wells’ Clinical Decision Rule to determine the likelihood of a DVT. Heart Disease – • One of leading causes of death in industrialized countries • CVD ~1 million deaths/year in United States • >1 in 4 Americans has some form CVD • ~ half of deaths from heart disease are sudden and unexpected • 63% of women who died unexpectedly from heart disease had no prior symptoms • Sudden death is first symptoms for half of all men who have heart attack • Likelihood of heart attack in morning is 40% higher • Presence of silent MI increases with age What does this mean to us? This means many of your patients will have heart disease and could experience sudden distress, have silent disease or subtle symptoms. This means as therapists we need to be aware and screening for these possibilities with every patient! Need to know CPR and how to use a defibrillator! Signs and Symptoms of Heart Disease: • Chest pain • Neck and/or arm pain • Palpitations • Dyspnea (shortness of breath) • Syncope (fainting) • Cough • Diaphoresis • Cyanosis • Pain with sweats Signs and Symptoms of Vascular Disease: • Edema • Claudication (leg pain) • Cold hands and feet • Open wounds • Skin discoloration Cardiovascular disease can affect other systems: Page 1 of 8 General: weakness, fatigue, weight change, poor exercise tolerance, peripheral edema Integumentary: pressure ulcers, loss of body hair, cyanosis (lips and nail beds) Central Nervous System: headaches, impaired vision, dizziness or syncope Pulmonary: labored breathing, dyspnea, productive cough Genitourinary: urinary frequency, nocturia, concentrated urine, decreased urine output Musculoskeletal: chest, shoulder, back, neck jaw or arm pain, myalgias, muscular fatigue, muscle atrophy, edema, claudication Gastrointestinal: nausea, vomiting, ascites Chest Pain • May be cardiac or non-cardiac in origin • Can radiate to neck, jaw, upper trapezius, upper back, shoulder or arms (most commonly left arm) • Radiating pain follows ulnar nerve distribution • Cardiac-related chest pain may be related to • Angina • MI • Pericarditis • Endocarditis • Mitral valve prolapse • Dissecting aortic aneurysm • Often associated with other signs and symptoms – nausea, vomiting, diaphoresis, dyspnea, fatigue, pallor, or syncope • Cervical disk disease and arthritic changes can mimic atypical chest pain of angina pectoris (location and description of complaints vary with the underlying pathology) Palpitations: • • • • • • • • • • Presence of an irregular heartbeat Referred to as arrhythmias or dysrhythmias May be considered physiologic (normal) if less than six beats per minute Related to benign conditions such as mitral valve prolapse, ‘athlete’s heart”, caffeine, anxiety or exercise Related to severe conditions such as coronary artery disease, cardiomyopathy, complete heart block, ventricular aneurysm, atrioventricular valve disease, mitral or aortic stenosis Describes as racing, jump, bump, pound, flop, or flutter sensation of heart, sense of skipping beats Associated signs can include lightheadedness or syncope Palpitations lasting for hours or occurring in conjunction with pain, SOB, fainting, or severe lightheadedness or in individuals with family history of sudden death require medical referral Patients can describe ‘palpitations’ related to overactive thyroid, caffeine use, medication side effects or use of illegal drugs (cocaine) Palpitations as a recurring symptom requires medical referral Dyspnea: breathlessness or shortness of breath • Can be cardiac or pulmonary in origin • Can be related to activity, exertion or body position • Orthopnea – difficulty breathing when recumbent • Platypnea – difficulty breathing when sitting upright and ease of breathing when recumbent • Severity of dyspnea is related to extent of disease Page 2 of 8 • • • • • • • Dyspnea on exertion (DOE) – often result of left ventricle dysfunction, failure to clear all blood from lungs resulting in pulmonary congestion and SOB Extreme dyspnea includes Paroxysmal nocturnal dyspnea (PND) and orthopnea (breathlessness relieved by sitting upright with pillows to support the trunk and head) PND and sudden, unexplained episodes of SOB often accompany congestive heart failure upright position during day, fluid shunted away from lungs, increased perfusion; recumbent position at night, increase fluid returned to lungs creating dyspnea Dyspnea relieved by specific breathing (pursed-lip breathing) or by specific body position (leaning forward on arms) generally related to pulmonary disease rather than cardiac Patients with known cardiac involvement who develop progressively worse dyspnea needs referral to physician Patients who cannot climb a single flight of stairs without feeling moderately or severely winded should have referral to physician Patients who are awakened at night or experience shortness of breath when lying down need referral to physician Cardiac syncope (fainting): • Sudden loss of consciousness accompanied by an inability to maintain postural tone • Can be related to reduced oxygen delivery to brain • Cardiac causes include – arrhythmias, orthostatic hypotension, poor ventricular function, coronary artery disease, vertebral artery insufficiency • Non-cardiac causes – anxiety, metabolic, emotional stress can cause hyperventilation and subsequent lightheadedness (vasovagal syncope) • Related to side effects of medications (vasodilators) • Syncope without warning period of lightheadedness, dizziness, or nausea may be heart valve or arrhythmia • increased incidence with age, especially marked after age 70 • Medical referral recommended for unexplained syncope, especially in presence of heart or circulatory problems or if risk factors for heart attack or stroke are present Fatigue: • Can be related to cardiac dysfunction, provoked by minimal exertion, possible causes include coronary artery disease, aortic valve dysfunction, cardiomyopathy, myocarditis • Fatigue of cardiac nature often accompanied by associated symptoms – dyspnea, chest pain, palpitations, headache • Beta-blockers prescribed for cardiac problems (hypertension, angina, anti-arrhythmias) can create unusual fatigue • Can be related to metabolic, neurologic, muscular or pulmonary pathology • Is there an explanation? Sleep disturbances, etc. • Fatigue beyond expectations during or after exercise is RED FLAG Cough: • •Generally associated with pulmonary disease, but can be pulmonary complication of cardiac disease • Cough, especially at night, can be associated with heart failure, side effect of calcium channel blockers • Left ventricular dysfunction, mitral valve dysfunction resulting in pulmonary edema or left ventricular CHF • Cough associated with exercise, metabolic stress, supine position, or PND • Hacking cough, can produce large amount of frothy, blood-tinged sputum • Congestive heart failure – large amount of fluid trapped in pulmonary tree, irritating lung mucosa Page 3 of 8 Cyanosis: • Bluish discoloration of lips, and nail beds of fingers and toes • Suggests inadequate blood oxygen levels, reduced hemoglobin levels • Most often associated with cardiac and pulmonary problems • Can be related to hematologic or CNS disorder • Central cyanosis – oxygen levels reduced in arterial blood (lung disease, congestive heart disease, abnormal hemoglobin) • Peripheral cyanosis – normal blood oxygenation but decreased or slow blood flow (congestive heart failure, venous obstruction, anxiety, cold environment) Edema: • Accumulation of fluid, 3 lb. weight gain or greater or gradual, continuous gain over several days that results in swelling of the ankles, abdomen, and hands combined with SOB, fatigue and dizziness may be red-flag for CHF • Other accompanying signs may be jugular vein distention, cyanosis (lips and appendages), right upper quadrant pain-constant aching or sharp pain may occur secondary to enlarged liver • Right heart failure can occur secondary to cardiac surgery, venous valve incompetence or obstruction, cardiac valve stenosis, coronary artery disease, mitral valve dysfunction • Noncardiac causes of edema include pulmonary hypertension, kidney dysfunction, cirrohosis, burns, infection, lymphatic obstruction, use of nonsteroidal anti-inflammatory drugs or allergic reactions, deep venous thrombosis • Edema and accompanying symptoms persist despite rest, medical referral is required • Edema of peripheral origin requires treatment of underlying etiology Claudication: • Leg pain associated with peripheral vascular disease, often simultaneously with coronary artery disease • Often functional debilitating • Can occur with other symptoms such as angina or dyspnea • Pitting edema along with leg pain often seen with peripheral vascular disease • • • • • • Non-cardiac causes of leg pain should be ruled out – sciatica, pseudoclaudication, anterior compartment syndrome, gout, peripheral neuropathy Pseudoclaudication with low back disease often indicates spinal stenosis, discomfort frequently bilateral, relieved by rest or flexion of lumbar spine Vascular claudication may occur without physical findings, but usually accompanied by skin discoloration and trophic changes (dry, thin, hairless skin) in presence of vascular disease Assess core temperature, skin temperature and peripheral pulses, cool skin more indicative of vascular obstruction, warm skin likely infection or inflammation Abrupt onset of ischemic rest pain or sudden worsening of intermittent claudication may be due to thromboembolism, need immediate physician referral Intermittent claudication with normal-appearing skin, exercise to point of claudication, marked pallor in upper and lower extremities due to shunting of blood Three P’s: 1. Pleuritic Pain (exacerbated by respiratory movements involving the diaphragm such as sighing, deep breathing, coughing, sneezing, laughing or hiccups, can be cardiac in origin if pericariditis or may be pulmonary) 2. Pain on palpation (musculoskeletal in origin) Page 4 of 8 3. Pain with changes in position (musculoskeletal or pulmonary, pain that is worse when lying down and improves with sitting up or leaning forward is often pleuritic in nature) If two of three P’s are present, MI unlikely. MI or anginal pain occurs in approximately 5-7% of clients with pain reproduced with palpation. Symptoms alter with positioning, % drops to 2%. If chest pain reproduced with respiratory movements, likelihood of coronary event only 1%! Wells’ Clinical Decision Rule for DVT Clinical Presentation Score Active Cancer (within 6 months of diagnosis or receiving palliative care) Paralysis, paresis, or recent immobilization of lower extremity Bedridden for more than 3 days or major surgery in last 4 weeks Localized tenderness in the center of the posterior calf, the popliteal space, or along the femoral vein in the anterior thigh/groin Entire lower extremity swelling 1 Unilateral calf swelling (more than 3 mm larger than uninvolved side) Collateral superficial veins (nonvaricose) 1 An alternative diagnosis is as likely (or more likely) than DVT (cellulitis, postoperative swelling, calf strain) TOTAL POINTS -2 KEY -2 to 0 1 to 2 3 or more Low probability of DVT Moderate probability of DVT High probability of DVT 1 1 1 1 1 (3%) (17%) (75%) Medical consultation advised for low probability! Medical referral is required for moderate or high probability! MONITOR VITAL SIGNS!!! • • • Longer pulse counts (one minute) more accurate, greater detection of arrhythmias Look for abnormally high or low HR prior to activity, and in response to activity, monitor regularity of heart rate Increase in HR of 20bpm and that lasts > 3 minutes post rest or a change in position • Wolthius (1977): healthy men (n = 700) exercising at 66% of maximal capacity (13/20 RPE) showed the following increase in vital signs: • HR ~50 bpm • SBP ~30 mm • DBP ~8 mm • Wolthius RA (1977) The response of healthy men to treadmill exercise. Circulation 55:153-157. • DeTurk p.530: a rise in HR of > 50 bpm during exercise testing is a predictor of successful CHF rehab. Page 5 of 8 This is a little bit like apples and oranges however, because stress testing is a more medical, controlled environment, especially maximal exertion testing. In the clinic, we have to be more conservative. • Resting SBP > 120 mmHg and/or DBP > 80 mmHg, especially with other risk factors • Persistent rise or fall in BP over time (at least 3 consecutive readings over 2 weeks), especially if taking NSAIDs or woman on birth control pills • Watch for systolic BP that does not rise as work level increases • Watch for systolic BP that falls with increasing work loads • Lower standing SBP in adults over age 65 with history of falls • A difference in resting pulse pressure greater than 40 mmHg Healthy men exercising at 66% of maximal capacity (13/20 RPE) had a pulse pressure (SBP – DBP) of ~80 mm HRWolthius RA (1977) The response of healthy men to treadmill exercise. Circulation 55:153-157. • Watch for change in diastolic BP greater than 15-20 mmHg • Remember some BP meds can keep HR lower (beta-blockers, digitalis, anti-dysrhythmias), use of rate of perceived exertion is an acceptable gauge of exercise intensity • Persons taking medications, such as beta-blockers or calcium channel blockers, may not achieve target heart rate above 90bpm, safe rate of exercise, heart rate at two minutes post exercise should return to resting level • Patients being treated with NSAIDs and ACE inhibitors must be monitored closely during exercise for elevated blood pressure • Older adults (over 75) with decreasing BP over time may be early sign of Alzheimer’s, DBP <70mmHg or decreases in SBP > 15 mmHg over 3 year period- increases risk of dementia • Clients with stable angina usually has normal BP, BP may be elevated when anxiety accompanies chest pain or during acute coronary insufficiency • BP in lower extremities that is lower than in upper extremities • BP changes in the presence of other warnings signs such as new or unstable angina, dizziness, nausea, pallor, extreme diaphoresis • Sudden fall in blood pressure (more than 10 to 15 mmHg of SBP) or more than 10 mmHg DBP with concommitant rise in pulse (orthostatic hypotension), watch for postural hypotension in hypertensive patients especially those on diuretics Normal values: Heart rate: Adult: 60-100 bpm Child 5-12: 65-110 bpm Child 1-7: 70-110 bpm Infant, 6 months: 100-160 bpm Newborn: 120-200 bpm Normal Ranges for Blood Pressure by Patient Age Systolic Systolic Diastolic Diastolic Age (years) Maximum Minimum Maximum Minimum Newborn Children 90 60 60 30 Less than 130 75 90 45 3 6-9 120 90 80 50 Key notes: heart rate and respiratory rate go down with age, BP goes up Age Systolic Diastolic Page 6 of 8 Young Adults Adults <120 <80 14-19 <120 <80 20-60 <120 <80 60+ <120 <80 Well-conditioned athletes tend to have lower BP values Values combined from: The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, 2004. Long T., Toscano K. Handbook of Pediatric Physical Therapy (2nd ed). Lippincott, Williams, and Wilkins, 2002. Guidelines for Immediate Medical Attention: • Sudden worsening of intermittent claudication may be due to thromboembolism • Symptoms of TIAs especially in individuals with history of heart disease, hypertension, or tobacco use • Onset of angina requires immediate cessation of exercise, should subside within 3-5 minutes, use of nitroglycerin (females can get results with antacids) as prescribed, anginal pain not relieved within 20 minutes or in presence of nausea, vomiting or profuse sweating – immediate attention • Changes in presence of angina, such as increased intensity, decreased threshold of stimulus, or longer duration of pain; pain associated with MI is not relieved by rest, change of position, or administration of nitroglycerin or antacids • Have patient contact physician before leaving therapy, do not leave nursing unit unaccompanied; return to Guidelines for Physician Referral: • Client has combination of systemic signs or symptoms at presentation • Women with chest or breast pain with positive family history or breast cancer • Palpitations in any person with history of unexplained sudden death in the family; more than six episodes of palpitations in 1 minute; palpitations lasting for hours or occurring in association with pain, SOB, fainting, or severe lightheadedness • Anyone who cannot climb a single flight of stairs without feeling moderately to severely winded or who awakens at night or experiences shortness of breath when lying down • Fainting (syncope) without warning period of lightheadedness, dizziness or nausea may be sign if valve disease or arrhythmia; unexplained syncope in presence of heart or circulatory problems (or risk factors for heart attack or stroke) • Clients who are neurologically unstable often exhibit new arrhythmias, these new arrhythmias require referral • Known cardiac clients who • Fail to relieve anginal pain with use of nitroglycerin • Change in pattern of angina • Abnormally severe chest pain with nausea and vomiting • Anginal pain not relieved by rest • Anginal pain radiates to jaw or left arm • Upper back abnormally cool, sweaty, or moist to touch • Client develops progressively worse dyspnea • Individual with coronary artery stent experiencing chest pain Page 7 of 8 • Client demonstrates difference of more than 40 mmHg in resting pulse pressure; alternatively, if pulse pressure is < 10 mm in resting or in response to exercise, that is not good either (DeTurk p.530). (SBP-DBP=pulse pressure) Client has any doubt about his or her present condition • • • Clues for Screening Cardiovascular Signs and Symptoms: • • • • • • • • • • • • • • • • • Personal history of heart disease including hypertension Age (postmenopausal women, anyone over 65) Ethnicity (black women) Other signs or symptoms – pallor, unexplained profuse perspiration, inability to talk, nausea, vomiting, sense of impending doom or extreme anxiety Three P’s Chest pain may occur from intercostal muscle or periosteal trauma from vigorous coughing, palpation of local chest wall produces tenderness, look for associated signs or symptoms Angina is activated by physical exertion, emotional reactions, large meal or exposure to cold – lag time of 5-10 minutes, immediate pain is likely to be musculoskeletal, TOS, or psychologic Chest pain, shoulder pain or TMJ pain occurring in presence of coronary artery disease or previous history of MI, especially if accompanied by associated signs or symptoms Upper quadrant pain, that can be induced or reproduced by lower quadrant activity, such as biking, stair climbing, or walking without use of arms – usually cardiac in origin Recent history of pericarditis in presence of new chest, neck, or left shoulder pain, observe for additional symptoms of dyspnea, increased pulse rate, elevated body temperature, malaise or myalgias Individual with known risk factors for congestive heart disease, especially a history of angina, becomes weak or short of breath while working with arms overhead, ischemia or infarction is likely cause of pain and associated symptoms Insidious onset of joint or muscle pain in older client who has previously diagnosed heart murmur may be caused by bacterial endocarditis, usually no morning stiffness to differentiate it from RA Back pain associated with herniated lumbar disk but without neurologic deficits especially in presence of heart murmur may be caused by bacterial endocarditis Watch for arrhythmias in neurologically unstable clients (SCI, new CVA or new brain injury, check pulse and ask/observe for dizziness Anyone with chest pain must be evaluated for trigger points; if palpation of chest reproduces symptoms (especially radiating pain), deactivation of trigger points must be carried out and followed by reevaluation as part of screening for cardiac origin Symptoms of vascular occlusive disease include exertional calf pain that is relieved by rest (intermittent claudication), nocturnal aching of foot and forefoot (rest pain), and classic skin changes, especially hair loss of foot and ankle; ischemic rest pain is relieved by placing limb in dependent position Throbbing pain at base of neck and/or along the back into interscapular areas that increases with exertion requires monitoring of vital signs and palpation of peripheral pulses to screen for aneurysm, check for palpable abdominal heartbeat that increases in supine References: 1. 2. 3. 4. Goodman CC., Snyder TE. Differential Diagnosis for Physical Therapists: Screening for Referral (4th ed.). St. Louis: Saunders-Elsevier, 2007. Boissonnault WG. Primary Care for the Physical Therapist: Examination and Triage. St. Louis: Saunders-Elsevier, 2005. Long T., Toscano K. Handbook of Pediatric Physical Therapy (2nd ed). Lippincott, Williams, and Wilkins, 2002. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, 2004. Page 8 of 8