5 pages article - why
advertisement

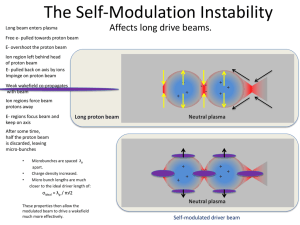
HARNESSING THE POWER OF PROTONS TO FIGHT CANCER Belgian company, IBA, designs and equips proton therapy centers worldwide As charged particles in atoms, protons have a long history of use in laboratories around the world as a staple of nuclear physics research. Today, the power of protons is also being employed in clinical environments to treat a range of cancers in children and adults. Protons have a number of favorable qualities that make them increasingly effective tools for physicians and physicists to successfully treat cancer patients and offer them a new life. IBA has been at the forefront of harnessing proton beams for the treatment of cancer. Since 1986, the company has provided advanced technology, as well as clinical, scientific and engineering expertise, to the majority of clinically-dedicated proton therapy facilities in the world. Headquartered in Brussels, Belgium, with offices in Beijing, China, and Jacksonville, Florida, USA, IBA works continuously to innovate and provide the most effective and cost-efficient solutions to make this lifesaving therapy available to more people. Proton therapy vs. conventional X-ray radiation Proton therapy (also known as particle therapy) is a form of external beam radiotherapy that uses beams of energized protons to treat cancer. These proton beams are aimed at the tumor and damage the DNA of cancer cells, ultimately destroying them. Cancerous cells are particularly vulnerable to such attacks. The primary advantage of proton therapy is its ability to localize beam dosage more precisely than other types of external beam radiotherapy, such as traditional X-ray (photon) therapy, without harming healthy, neighboring tissue. X-rays are electromagnetic waves that are highly penetrating, delivering a dose throughout any volume of tissue irradiated, regardless of thickness. As a result, they always deliver substantial doses of irradiation anterior and posterior to any tumor volume. X-ray beams also deliver their maximum dose of radiation from a depth of as little as 0.5 cm to a maximum of 3 cm, depending on the energy utilized. Because a tumor is almost always located deeper than these ranges, a higher dose is delivered to the normal tissues anterior to the tumor, and the tumor is treated in the region of the beam where the energy deposition is falling off. 1 Conversely, the absorbed dose of a proton beam increases very gradually with depth, suddenly rising to a peak at the end of a proton range. This is known as the Bragg peak. The proton beam can be directed so that the Bragg peak occurs precisely within the tumor volume, something that can never be achieved with X-rays. 2 Proton therapy offers the most favorable dose deposition properties possible with external beam techniques. And, it can easily be combined with chemotherapy and/or surgery, depending upon the needs of each patient. With fewer and less-severe treatment side effects, proton therapy can mean a better quality of life for patients and, ultimately, healthcare cost savings. How proton therapy works In IBA-equipped proton therapy centers, cyclotrons accelerate protons to an extremely high speed, generating a controlled beam. The energy required for a particular treatment is transformed from the cyclotron-generated energy using a variable Energy Degrader along with an Energy Selection System October 2012 www.iba-protontherapy.com 1 (ESS). October 2012 www.iba-protontherapy.com 2 The ESS transforms the fixed energy beam from the cyclotron into a variable energy beam with a verified and controlled absolute energy, spread and emittance. Degrading and scraping the beam in the ESS shields the patient from the neutrons that would otherwise be generated in the treatment room. This proton beam travels through a Beam Transport and Switching System which consists of a series of powerful electromagnets that focus the beam as it leaves the cyclotron, transport it via a beam tube, and direct it to the entry point of each selected treatment room. The beam is then delivered through a nozzle to the targeted tumor. The proton beam can be contoured to the shape of the tumor, further decreasing radiation exposure to healthy cells and limiting side effects. Protons have very specific and useful properties. As previously mentioned, they deposit the majority of their destructive energy only at a specific depth, the Bragg peak, which can be precisely calculated as a function of the beam’s initial energy. Brief history of proton therapy In 1946, American physicist Robert Wilson first proposed the use of protons for cancer treatment in a scientific article. Two years later, researchers at the Lawrence Berkeley Laboratory (LBL) in Berkeley, California, USA, confirmed Wilson’s predictions that proton beam therapy could be an effective cancer therapy. The first treatments on humans took place at LBL and, in the 1950s, treatments were successfully replicated on patients at a facility in Uppsala, Sweden. In the 1960s, the Harvard Cyclotron Facility at Harvard University in Boston, Massachusetts, USA, expanded the use of protons in patients with a variety of malignancies. The world's first hospital-based proton therapy center was built in 1990 at the Loma Linda University Medical Center in Loma Linda, California, USA. Eight years later, IBA introduced its first cyclotron for proton therapy, which revolutionized the world of radiation oncology. In 2001, IBA installed its first proton therapy system at the Francis H. Burr Proton Therapy Center at Massachusetts General Hospital in Boston, USA. Advantages of proton therapy Proton therapy’s primary advantage is superior dose distribution, giving physicians more precise control while delivering the highest possible dose directly to the tumor, sparing surrounding tissues and critical structures, and reducing overall toxicity. Proton therapy • precisely delivers an optimal radiation dose to the tumor; • safely escalates the dose within a confined treatment volume, with minimal or no exit dose; • reduces the probability and/or severity of side effects on healthy surrounding tissues; • can increase the long-term, progression-free survival rates for certain types of tumors. Proton therapy is especially appropriate for cancers with limited treatment options and those where conventional X-ray radiotherapy presents an unacceptable risk to the patient. These include cancers of the eye and brain, tumors close to the brain stem and spinal cord, prostate, lung and pediatric cancers. With pediatric cancers in particular, avoiding even moderate amounts of radiation to normal tissues is vital to preventing cognitive impairments, growth defects, cardiac damage, radiation-induced tumors and other morbidities later in life. In addition to cancer, proton therapy has been effectively used to treat Parkinson’s disease, epilepsy, macular degeneration, arteriovenous malformations, severe rheumatologic conditions and seizure disorders. October 2012 www.iba-protontherapy.com 3 Proton therapy equipment Some aspects of a proton therapy center are standard. For example, because proton therapy equipment, such as a cyclotron and gantry, are enormous in size and very heavy, a substantial concrete foundation and main floor, and 8- to 12-foot-thick walls are required in every center. The foundation and floor support the heavy equipment, and the thick walls offer shielding from harmful neutrons. Even with these requirements, IBA offers a modular approach to facility design that is scalable and adaptable to the specific goals of a particular medical group. A number of customers choose to start with a larger center of four or five patient treatment rooms while others opt to begin with a single treatment room and add rooms as the practice expands. IBA is at the forefront of developing the technology used in proton therapy systems. With FDA clearance in the United States, CE marking in Europe and SFDA clearance in China, IBA leads the world in regulatory clearance of proton-beam treatment systems. IBA offers a number of leading-edge beam delivery equipment and patient-positioning systems, all designed for reliability, flexibility, ease of use and patient comfort. The IBA Universal Nozzle offers the flexibility to select the preferred beam delivery mode automatically within a single treatment room. It delivers a proton beam in any of four delivery modes: Single Scattering, Double Scattering, Uniform Scanning and Pencil Beam Scanning. IBA is the first and only company with this all-in-one, integrated system. Pencil Beam Scanning uses a proton beam that is actively scanned through the target tumor volume. It provides improved three-dimensional conformity to the target, allowing for better sparing of organs at risk and healthy tissues. This technology was developed by IBA in close collaboration with the Francis H. Burr Proton Therapy Center at Massachusetts General Hospital in Boston. A Fixed-Beam Treatment Room can be designed for ocular, intracranial, and head and neck treatment, or for research. The room features a horizontal beam that can also be used with a Robotic Patient Positioning System (RPPS*) for more treatment versatility. The RPPS can also be used in a gantry treatment room. It offers six degrees of freedom of motion, allowing maximum flexibility to position the patient more precisely for proton beam treatment. The 360° Gantry Treatment Room offers a less intimidating, more pleasant environment to help minimize patient anxiety, with functional and aesthetic improvements in color, lighting and contoured surfaces. The future of proton therapy Because there are relatively few proton therapy facilities, existing sites treat not only patients from their region, but also those from around the world. It is clear that when seeking the best possible cancer treatment, patients are not deterred by distance. With tens of thousands of patients who could benefit from proton therapy and only 24 centers in the world, access is a significant problem. One of the reasons for the shortage of clinically-based proton therapy centers is financial. On average, it costs anywhere from $25 million to $150 million to build and equip a proton therapy center. IBA is dedicated to making proton therapy more available to patients, as well as more affordable to healthcare systems. For example, IBA is currently developing ProteusONE*, a smaller, more cost-effective proton therapy system. This new design produces fewer construction-related treatment disruptions, requires less space and leaves a smaller footprint. The single-room system is about one-third the size of the current gantry configuration. This is made possible by a much smaller cyclotron, a shorter beam route from cyclotron to treatment room and a smaller, more compact gantry. This decreased size will translate to significant cost savings. October 2012 www.iba-protontherapy.com 4 To date, IBA has installed 12 proton therapy centers worldwide. Ten more are in various stages of development in Krakow, Poland; Prague, Czech Republic; Trento, Italy; Dresden, Germany; Essen, Germany; Uppsala, Sweden; Dimitrovgrad, Russia; Seattle, Washington, USA; Knoxville, Tennessee; and Shreveport, Louisiana. The company is committed to developing innovative solutions to make proton therapy more personalized, more efficient and more accessible, both now and in the future. * Subject to review by Competent Authorities (FDA, European Notified Bodies, et al.) before being put on the market. Visit IBA online at www.iba-protontherapy.com. FOOTNOTES 1. Shinohara, E. Module 1: An Introduction to Proton Therapy. OncoLink, The Abramson Cancer Center of the University of Pennsylvania. http://www.oncolink.org/treatment/article.cfm?c=9&s=131&id=412. Accessed Feb. 11, 2011. 2. Ibid. [SUGGESTED GRAPHICS] [GRAPHIC THAT INCLUDES BRAGG PEAK] [GRAPHIC: ProteusPLUS Center Birds Eye View] [GRAPHIC: IBA 360° GANTRY TREATMENT ROOM] [GRAPHIC: WORL MAP OF IBA-EQUIPPED PROTON THERAPY CENTERS] CURRENT WORD COUNT: Approx. 1,840 October 2012 www.iba-protontherapy.com 5