NS350 Exam 1 - WordPress.com
advertisement
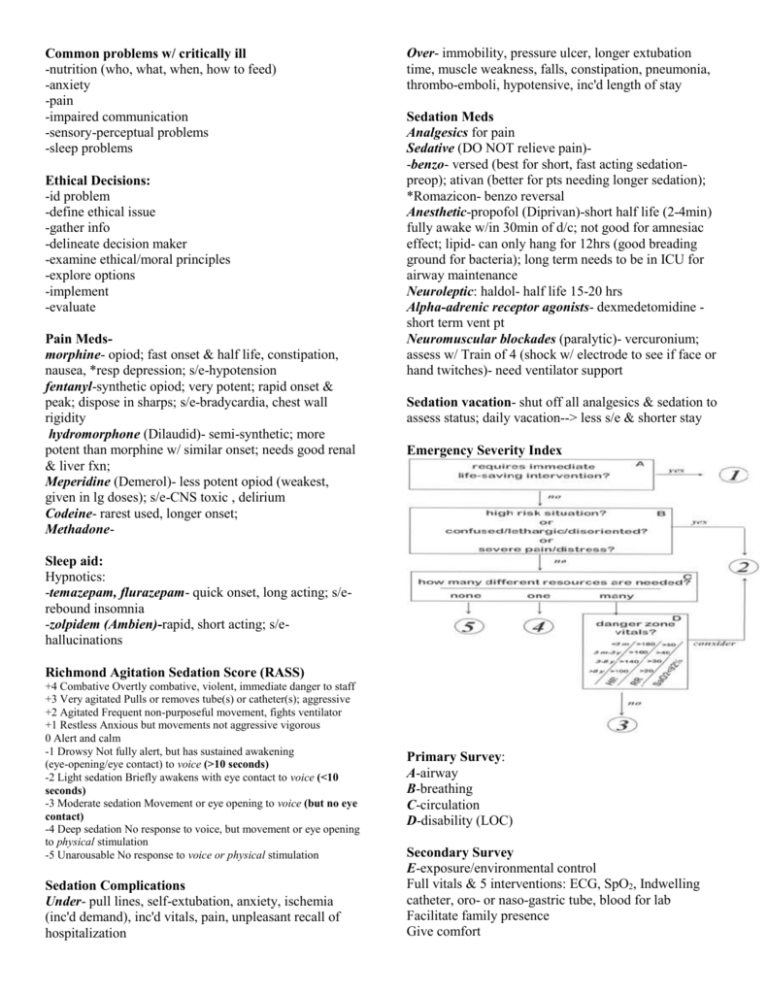
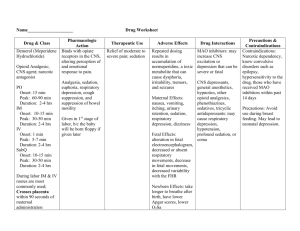
Common problems w/ critically ill -nutrition (who, what, when, how to feed) -anxiety -pain -impaired communication -sensory-perceptual problems -sleep problems Ethical Decisions: -id problem -define ethical issue -gather info -delineate decision maker -examine ethical/moral principles -explore options -implement -evaluate Pain Medsmorphine- opiod; fast onset & half life, constipation, nausea, *resp depression; s/e-hypotension fentanyl-synthetic opiod; very potent; rapid onset & peak; dispose in sharps; s/e-bradycardia, chest wall rigidity hydromorphone (Dilaudid)- semi-synthetic; more potent than morphine w/ similar onset; needs good renal & liver fxn; Meperidine (Demerol)- less potent opiod (weakest, given in lg doses); s/e-CNS toxic , delirium Codeine- rarest used, longer onset; Methadone- Over- immobility, pressure ulcer, longer extubation time, muscle weakness, falls, constipation, pneumonia, thrombo-emboli, hypotensive, inc'd length of stay Sedation Meds Analgesics for pain Sedative (DO NOT relieve pain)-benzo- versed (best for short, fast acting sedationpreop); ativan (better for pts needing longer sedation); *Romazicon- benzo reversal Anesthetic-propofol (Diprivan)-short half life (2-4min) fully awake w/in 30min of d/c; not good for amnesiac effect; lipid- can only hang for 12hrs (good breading ground for bacteria); long term needs to be in ICU for airway maintenance Neuroleptic: haldol- half life 15-20 hrs Alpha-adrenic receptor agonists- dexmedetomidine short term vent pt Neuromuscular blockades (paralytic)- vercuronium; assess w/ Train of 4 (shock w/ electrode to see if face or hand twitches)- need ventilator support Sedation vacation- shut off all analgesics & sedation to assess status; daily vacation--> less s/e & shorter stay Emergency Severity Index Sleep aid: Hypnotics: -temazepam, flurazepam- quick onset, long acting; s/erebound insomnia -zolpidem (Ambien)-rapid, short acting; s/ehallucinations Richmond Agitation Sedation Score (RASS) +4 Combative Overtly combative, violent, immediate danger to staff +3 Very agitated Pulls or removes tube(s) or catheter(s); aggressive +2 Agitated Frequent non-purposeful movement, fights ventilator +1 Restless Anxious but movements not aggressive vigorous 0 Alert and calm -1 Drowsy Not fully alert, but has sustained awakening (eye-opening/eye contact) to voice (>10 seconds) -2 Light sedation Briefly awakens with eye contact to voice (<10 seconds) -3 Moderate sedation Movement or eye opening to voice (but no eye contact) -4 Deep sedation No response to voice, but movement or eye opening to physical stimulation -5 Unarousable No response to voice or physical stimulation Sedation Complications Under- pull lines, self-extubation, anxiety, ischemia (inc'd demand), inc'd vitals, pain, unpleasant recall of hospitalization Primary Survey: A-airway B-breathing C-circulation D-disability (LOC) Secondary Survey E-exposure/environmental control Full vitals & 5 interventions: ECG, SpO2, Indwelling catheter, oro- or naso-gastric tube, blood for lab Facilitate family presence Give comfort History & head to toe Inspect posterior Eval tetanus prophylaxis, ongoing monitoring, prepare for transport Triage Emergent- life, limb, eye threatening; needs immediate attention; ie: CP, cardiac arrest, severe resp distress, chemicals in eyes, limb amputation, acute neuro deficits Urgent- needs tx in 20min-2hrs; ie: fever >104 (40), diastolic BP >130, kidney stone, simple fracture, abd pain, asthma/no resp distress Nonurgent- can wait hrs or days; ie: sprain, minor laceration, cold symptoms, rash, simple HA Mass Casualty Incident- Triage in 15 sec: Heat exhaustion/ stroke Etiology-lack of aclitimzation, prolonged exposure, physical exertion, head/spine injury, dehydration, thyrotoxicosis, diabetes, phenothiazines, tricyclic antidepressants, diuretics, cocaine, ethanol, antihistamines, CV diseas, CNS disorders, alcoholism S/S-severe muscle contractions, thirst; pale, ashen; fatigue, weakness; profuse sweating (skin becomes dry w/ heat stroke); altered mental status; hypotension; tachycardia; weak, thread pulse; temp 100-104oF (37.840.0oC) for exhaustion, >104oF (40oC) for heat stroke Interventions - initial: manage & maintain ABC’s; high flow O2 w/ non-rebreather or bag-mask; establish IV & fluid replacement; cool environment; rapid cooling measures for heat stroke (remove clothing, wet sheets, fan, ice bath, cool IV fluids, lavage w/ cool fluids); ECG; blood for electrolytes & CBC; urinary catheter -ongoing-monitor ABC’s, VS, LOC, cardiac rhythm, SpO2, electrolytes, urinary output, devel’t of myoglobinuria, clotting studies (for DIC) Hypothermia Etiology- prolonged exposure/submersion, inadequate clothing, hypoglycemia, hypothyroidism, cold IV fluids, blood admin, inadequate warming in ED or surgery, admin of neuromuscular blocking agents, phenothiazines, barbiturates, alcohol, trauma, shock S/S- core body temp: mild 90-95oF (32.2-35oC), mod 8790oF (30.6-32.2oC), profound <87oF (<30.6oC); shivering (diminished or absent w/ temp <92oF or 33.3oC); hypoventilations, hypotension, altered mental status; areflexia; pale, cyanotic; blue, white or frozen extremities; arrhythmias (brady, a-fib, v-fib, asystole); fixed, dilated pupils Interventions-initial- remove from cold environment; manage & maintain ABC’s; high flow O2 NRB or BMV; anticipate intubation for diminished or absent gag reflex; rewarm pt (passive- remove wet & apply dry clothing, warm blankets, admin warm fluids; active external- body-tobody contact, heating devices or radiant light; active core warming- warmed IV fluids, heated humidified O2, peritoneal/gastric/colonic lavage w/ warmed fluids); anticipate hemodialysis or cardiopulm bypass; warm cental trunk first in pts w/ profound hypothermia to avoid aftershock; IV access w/ 2 lg-bore catheters for fluid resuscitation; assess for other injuries; keep pt’s head covered w/ warm, dry towels or stocking cap to limit heat loss; tx gently to avoid inc’d cardiac irritability -ongoing-monitor ABC’s, LOC, temp, VS, SpO2, cardiac rhythm, electrolytes, glucose Anthrax (bacillus antrhacis)- inhalation (most deadly), cutaneous (most common) or GI Manifestations- incubate 1-2days up to 6 wks; abrupt onset; dyspnea; diaphoresis; fever; cough; CP; septicemia; shock; meningitis; resp fail; widened mediastinum on x-ray Transmission- direct contact, no person-to-person, spores dormant until enter living host Tx- ATB effective only if tx’d early; Cipro is tx of choice; also use PCN, doxycycline; post expure prophylaxis for 30 days if vaccine avail, 60 days if no vaccine; vaccine has limited availability Small pox (varioloa major & minor viruses) Manifestations- incubation 7-17 days; sudden onset of symptoms- fever, HA, myalgia, lesions that progress from macules to papules to pustular vesicles, malaise, back pain Transmission- highly contagious, direct person-toperson, air droplets, handling contaminated materials Tx- no known care, Cidofovir (Vistide) under testing; isolation for containment; vaccine