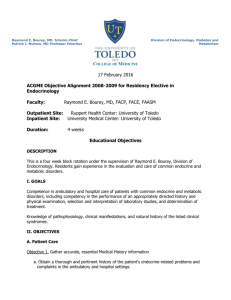
internal medicine residency program

PRINCE GEORGE’S HOSPITAL CENTER
INTERNAL MEDICINE RESIDENCY PROGRAM
SECTION 9: ENDOCRINOLOGY, DIABETES AND METABOLISM
This section has been reviewed and approved by the Chief, Division of Emergency Medicine as well as the Program Director, Internal Med icine Residency Program at Prince George’s
Hospital Center.
________________________
Chief, Division Of Endocrinology
______________________________
Program Director, Residency Program
I. Overview
Endocrinology is the diagnosis and care of disorders of the endocrine system. The principal endocrine problems handled by the general internist include goiter, thyroid nodules, thyroid dysfunction, diabetes mellitus, hyper- and hypocalcemia, adrenal cortex hyper- and hypofunction, endocrine hypertension, gonadal disorders, hyper- and hyponatremia, certain manifestations of pituitary tumors, disorders of mineral metabolism, and hyperlipidemias. Obesity is not strictly an endocrine disorder but is considered part of the spectrum of endocrinology because it frequently enters into the differential diagnosis of endocrine disease and is a major element in the management of non-insulin-dependent diabetes. Preventive efforts focus on complications of hyper lipidemias, obesity, thyroid dysfunction, osteoporosis and diabetes mellitus, and on endocrinologic side effects of pharmacologic glucocorticoids and other medications.
The general internist must be able to evaluate and manage common endocrine disorders and refer appropriately. He/she must also be able to evaluate and identify the endocrinologic implications of abnormal serum electrolytes, hypertension, fatigue, and other nonspecific presentations. The general internist plays a key role in managing endocrine emergencies, particularly those encountered in the intensive care unit, including diabetic ketoacidosis and hyperosmolar nonketotic stupor, sever hyper- and hypocalcemia, and addisonian crisis.
During the rotation residents will be expected to perform a history and physical examination on their patients. Responsibility for formulating diagnostic evaluations and treatment plans will be emphasized. Patients will include hospitalized service with a variety of endocrine, metabolic, electrolyte and bone and mineral disorders. The rotation will help residents to evaluate and develop a diagnostic and therapeutic approach to patients with diabetes, thyroid, lipid and osteoporotic disorders. The residents also become familiar with screening guidelines for osteoporosis, diabetes, hypercholesterolemia, subclinical hypo and hyper thyroidism, and asymptomatic primary hyperthyroidism. Residents are also encouraged to attend the attending’s outpatient clinic once a week to broaden the outpatient experience in the subspecialty. Resident responsibilities for the subspecialty rotations are detailed under Section I of the Resident
Handbook.
II. Principle Teaching Methods
It consists of frequent encounters with the attending physician regarding patient care.
The resident will discuss all patients with the attending physician and interpret clinical data to formulate a differential. The attending will assign reading topics on a regular basis and review the material with the residents. This will include accepted national guidelines used in the diagnosis and treatment of various endocrine, metabolic and bone and mineral diseases. The faculty will also critique the residents consult notes, examination and management plan. Rounds will include short 15-30 minute discussions on current topics driven by patient encounters and initiated by resident and completed by the attending physician on most days. Latest information dealing with the topic as provided by literature search and pertinent articles should be discussed.
Residents will also receive outpatient experience in endocrinology by shadowing Dr
Sotoudeh one halfday a week (Thursday morning at 7:30 am). Residents must turn in a signed attendance sheet (attached at the end of this section) for the month to the program coordinator at the end of the month.
The residents are also required to manage/ interpret results of common endocrine issues. These requirements are delineated in the form of a logsheet at the end of this section. During their rotation residents must make a double sided copy of the logsheet and complete the stated requirements by the end of the month. To receive a satisfactory for the month the residents must turn in a completed logsheet to the program coordinator.
III. Strengths and Limitations
The residents will be exposed to a broad range of clinical problems typical of a community-based practice with emphasis on inpatient illness and care. The teaching faculty for the rotation is committed to teaching and patient care with strong role model presentation. For patients with exceptionally unusual clinical problems, the care may require transfer to a tertiary referral center. Outpatient experience in the subspecialty is be obtained by shadowing the attending physician in their private office. Patients in the
IV. Goals and Objectives continuity clinic at Glenridge Medical Center also offer learning opportunities.
During the course of the year, residents will receive lectures on the following topics.
Residents are advised to pick up cases during the rotation pertaining to one of the following topics after discussion with the chief resident and endocrinology attending. This is to ensure that all of the following topics get covered. Some topics may require more than one scheduled lecture. The topics are:
Diabetic Ketoacidosis
Management of diabetes and new diabetic medications
Thyroid disorders
Parathyroid disorders and calcium metabolism
Electrolyte abnormalities (related to sodium, potassium)
Metabolic bone disease
Adrenal disorders
Pituitary disorders
Sex hormone disorders
Legend of Learning Activities
Learning Venues:
1. Direct Patient Care/Consultation
2. Attending Rounds
3. Core Lecture Series
4. Self Study
Evaluation Methods:
A. Attending Evaluation
B. Direct Observation
C. Nurses’ Evaluation
D. In-training Examination
Competency: Patient Care
Interview patients skillfully, gathers accurate and essential information with emphasis on endocrine disorders
Examine patients more skillfully with competent and complete observation of normal and abnormal signs with emphasis on endocrine disorders
Defi ne and prioritize patient’s medical problems
Generate and prioritize differential diagnoses with appropriate testing and therapeusis in a broad range of multisystem disorders as illustrated by endocrine illness
Develop rational, evidence-based management strategies
Demonstrate ability to generate differential diagnosis, diagnostic strategy, and to define appropriate therapeutic plan and modifications to ongoing therapy in patient with diabetes, diabetic ketoacidosis, or hyperglycemic, non-ketotic coma, fluid balance, adrenal and pituitary disorders, and thyroid disorders
Competency: Medical Knowledge
Expand clinically applicable knowledge base of the basic and clinical sciences underlying the care of patients.
Access and critically evaluate current medical information and scientific evidence relevant to patient care
Articulate the pathophysiology, evaluation, and management of disorders of the
Learning Venues Evaluation Methods
ALL A, B, D
1, 2
1, 2
ALL
ALL
1,2,3,4,
ALL
1, 2, 4
1,2,,4,
A, B, D
A, B
A, B
A, B, D
A, B, D
A, B, D
A, B, D
A, B, D
endocrine organs
Competency: Interpersonal and
Communication Skills
Interact in an effective way with physicians and nurses participating in the care of patients requiring endocrine consultation or care (including physicians requesting consultation, attendings, medical students, and other personnel)
Show understanding of differing patient preferences in diagnostic evaluation and management of endocrine disorders
Competency: Professionalism
1,2
1,2
A, B, C
A, B, C
Treat team members, primary care-givers, and patients with respect
Actively participate in consultations and rounds
1,2
1,2
Attend and present in scheduled conference 3,
A, B, C
Competency: Practice-Based Learning
Identify limitations of medical knowledge in evaluation and management of patients with endocrine disorders and use medical literature to address these gaps in medical knowledge
Competency: Systems-Based Practice
Understand barriers to optimal care of patients with diabetes, obesity, and chronic endocrine problems
1,2,4,
1,2,3,4 A
Understand how financing of diabetes care and care for chronic medical/endocrine conditions can influence patient care
Understand need for effective communication between multiple caregivers and sites (e.g., endocrinologists, primary care physicians, diabetes nurse educators, nutritionists, surgeons, interventional radiologists, social workers, hospitals, in- and out-patient units) in delivering optimal care to patients with diabetes and other chronic endocrine problems
1,2,3,4
1,2,3,4
V. Educational Content
A. Pituitary gland
1) Understand the causes and presentation of patients with:
Pituitary adenomas
A
A
A, B, C
A, sign in on attendance sheet
A
Prolactinomas
Panhypopituitarism
2) Interpretation of results of:
Pituitatary and target organ hormones
Serum prolactin concentration
Imaging studies of the sella turcica
Relationship between prolactin, gonadotropin, TSH and medications
B. Thyroid disorders
1) Understand the causes, presentation, pathophysiology, and management of:
Enlarged thyroid (goiter, nodule)
Hyperthyroidism, thyrotoxicosis, thyroid storm, thyroiditis
Hypothyroidism, myxedema coma
Sick euthyroid
Thyroid cancers
2) Order appropriate tests and interpret results of:
Serum thyroid function tests
Thyroid scanning and ultrasound
C. Parathyroid disorders
1) Understand the causes, presentation, pathophysiology, and management of:
Hypercalcemia
Hypocalcemia
Hyperparathyroidism (primary and secondary)
Vitamin D metabolism
2) Order appropriate tests and interpret results of:
Urinary calcium, phosphate, uric acid excretion
Serum phosphate concentration
D. Adrenal disorders
1) Recognition and management of:
Primary and secondary adrenal insufficiency, steroid dependency
Hypercortisolism
Hypoadrenocortisolism, acute
Hypoadrenocortisolism, chronic
Incidentalomas, Adenomas
2) Understand the pathophysiogy and interpretation of:
Dexamethasone suppression test (overnight)
Home blood glucose monitoring
ACTH stimulation test
Urinary sodium, potassium excretion
Urine metanephrine, VMA (vanillylmandelic acid), and total catecholamine levels
E. Pancreas
1) Know the pathophysiology, complications and updated management guidelines for diabetes as well as treat patients with:
Diabetic ketoacidosis
Type 1
Type 2
Gestational diabetes
Exocrine and endocrine functions of pancreas: including the standards of care for DM- cardiovascular risk reduction, BP and lipid control, lifestyle changes
Islet cell tumors (insulinomas glucagonomas, vipomas)
2) Understand and interpret results of:
Fasting and standardized postprandial serum glucose concentrations
Glycohemoglobin or serum fructosamine concentration Microalbuminuria
Serum and urine ketone concentrations (quantitative or qualitative)
Serum and urine osmolalities
F. Reproductive/sexual disorders
1) Understand the causes, presentation, pathophysiology, and management of:
Change in sexual function
Galactorrhea
Gynecomastia – differential diagnosis and management
Hirsutism/virilization
Hypogonadism, female menopause
Hypogonadism, male gonadal failure
Erectile dysfunction
Menstrual disorders, infertility; PCOS and its relation with metabolic syndrome
2) Order appropriate tests and interpret results of:
Serum gonadotropin concentrations (follicle-stimulating hormone, luteinizing hormone)
Estrogen, progesterone
Serum testosterone concentration
G. Bone disorders
1) Recognition and management of:
Osteopenia/osteoporosis
Paget’s disease of bone
2) Understand the indications and interpretation of:
Bone mineral analysis (densitometry)
Serum alkaline phosphatase activity (for Paget’s disease of bone)
H. Metabolic disorders
1) Understand the causes, pathophysiology and treatment of:
Hyperosmolar state
Hypoglycemia
Hyponatremia/hypernatremia (incliuding SIADH, Diabetes Insipidus)
Lipid disorders
Obesity and its complications
2) Interpret results of:
Serum and urine osmolalities
Lipid profile
BMI
Serum and urine electrolytes
I. Paraneoplastic syndromes
1) Recognise presentation, diagnose and management of ectopic hormone production from tumors (like PTHrP etc.)
2) Order appropriate tests and interpret results
VI. Recommended Readings
All senior residents are encouraged to read the MKSAP for Endocrinology during their one-month rotation. Questions will help develop analytical thinking. Residents should also consult the following texts during their rotation regarding the key clinical issues in diagnosis, pathophysiology and therapy raised by the patients they evaluate and care for on the consult rotation:
Harrison’s Principles of Internal Medicine
Principles and Practice of Endocrinology and Metabolism by K.L. Becker
Endocrine Secrets by M.T. McDermott
Williams Textbook of Endocrinology can be accessed through MDConsult
Residents are also encouraged to use MDConsult and Up To Date to read on a case-bycase basis. Other reading resources are as follows:
A. Diabetes
1) ADA practice recommendations for 2006. Diabetes Care29: S4-42
2) Anonymous. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). UK
Prospective Diabetes Study (UKPDS) Group. Lancet. 1998 Sep
12;352(9131):854-65
3) Wulffele MG. Kooy A. de Zeeuw D. et.al: The effect of metformin on blood pressure, plasma cholesterol and triglycerides in type 2 diabetes mellitus: a systematic review. J Intern Med. 2004 Jul;256(1):1-14
B. Dyslipidemias
1) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol
Education Program (NCEP) Expert Panel on Detection, Evaluation, And
Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA.
2001 May 16;285(19):2486
2) Maki KC. Dietary factors in the prevention of diabetes mellitus and coronary artery disease associated with the metabolic syndrome. Am J Cardiol. 2004 Jun
3;93(11A):12C-17C
3) LaRosa JC. Gotto AM Jr. Past, present, and future standards for management of dyslipidemia. Am J Med. 2004 Mar 22;116 Suppl 6A:3S-8S
4) Foley KA. Vasey J. Alexander CM. Markson LE. Development and validation of the hyperlipidemia: attitudes and beliefs in treatment (HABIT) survey for physicians. J Gen Intern Med. 2003 Dec;18(12):984-90
5) Lorenzo C. Okoloise M. Williams K. et.al: San Antonio Heart Study. The metabolic syndrome as predictor of type 2 diabetes: the San Antonio heart study.
Diabetes Care. 2003 Nov;26(11):3153-9
C. Thyroid Disorders
1) Baelaurt K, Franklyn JA. Thyroid hormone in health and disease. Journal of endocrinology 2005, Oct 187 (1) 1-15
2) Cooper DS. Ridgway EC. Thoughts on prevention of thyroid disease in the
United States. Thyroid. 2002 Oct;12(10):925-9
3) Vanderpump MP. Tunbridge WM. Epidemiology and prevention of clinical and subclinical hypothyroidism. Thyroid. 2002 Oct;12(10):839-47
4) Biondi B. Palmieri EA. Lombardi G. Fazio S. Subclinical hypothyroidism and cardiac function. Thyroid. 2002 Jun;12(6):505-10
5) Sawin CT. Subclinical hyperthyroidism and atrial fibrillation. Thyroid. 2002
Jun;12(6):501-3
6) Osman F. Gammage MD. Franklyn JA. Hyperthyroidism and cardiovascular morbidity and mortality. Thyroid. 2002 Jun;12(6):483-7
7) Fontanilla JC. Schneider AB. Sarne DH. The use of oral radiographic contrast agents in the management of hyperthyroidism. Thyroid. 2001 Jun;11(6):561-7
D. Primary Hyperparathyroidism
1) Bilezikian JP. Potts JT Jr. Fuleihan Gel-H. et.al: Summary statement from a workshop on asymptomatic primary hyperparathyroidism: a perspective for the
21st century. J Clin Endocrinol Metab. 2002 Dec;87(12):5353-61
2) Rao DS. Wallace EA. Antonelli RF. Talpos GB. Ansari MR. Jacobsen G. Divine
GW. Parfitt AM. Forearm bone density in primary hyperparathyroidism: long-term follow-up with and without parathyroidectomy. Clin Endocrinol (Oxf). 2003
Mar;58(3):348-54
3) Rao DS. Agarwal G. Talpos GB. Phillips ER. Bandeira F. Mishra SK. Mithal A.
Role of vitamin D and calcium nutrition in disease expression and parathyroid tumor growth in primary hyperparathyroidism: a global perspective. J Bone Miner
Res. 2002 Nov;17 Suppl 2:N75-80
4) Rao DS. Parathyroidectomy for asymptomatic primary hyperparathyroidism
(PHPT): is it worth the risk? J Endocrinol Invest. 2001 Feb;24(2):131-4
5) Talpos GB. Bone HG 3rd. Kleerekoper M. Phillips ER. Alam M. Honasoge M.
Divine GW. Rao DS. Randomized trial of parathyroidectomy in mild asymptomatic primary hyperparathyroidism: patient description and effects on the SF-36 health survey. Surgery. 2000 Dec;128(6):1013-20;discussion 1020-1,
2000
6) Rao DS. Honasoge M. Divine GW. Phillips ER. Lee MW. Ansari MR. Talpos GB.
Parfitt AM. Effect of vitamin D nutrition on parathyroid adenoma weight: pathogenetic and clinical implications. J Clin Endocrinol Metab. 2000
Mar;85(3):1054-8
E. Osteoporosis
1) Hauselmann HJ. Rizzoli R. A comprehensive review of treatments for postmenopausal osteoporosis. Osteoporos Int. 2003 Jan;14(1):2-12
2) Anonymous. Osteoporosis: review of the evidence for prevention, diagnosis and treatment and cost-effectiveness analysis. Introduction. Osteoporos Int. 1998;8
Suppl 4:S7-80
3) Looker AC. Bauer DC. Chesnut CH 3rd. et.al: Clinical use of biochemical markers of bone remodeling: current status and future directions. Osteoporos Int.
2000;11(6):467-80
4) Anonymous. Who are candidates for prevention and treatment for osteoporosis?
Osteoporos Int. 1997;7(1):1-6
F. Hormone/Estrogen Replacement Therapy
1) Anderson GL. Limacher M. Assaf AR. et.al: The Women's Health Initiative
Steering Committee. Effects of conjugated equine estrogen in postmenopausal women with hysterectomy: the Women's Health Initiative randomized controlled trial. JAMA. 2004 Apr 14;291(14):1701-12
PRINCE GEORGE’S HOSPITAL CENTER
INTERNAL MEDICINE RESIDENCY PROGRAM
ENDOCRINOLOGY LOGSHEET
RESIDENT NAME______________________________________________
PGY LEVEL_______________ ROTATION MONTH_____________
LABORATORY
DATA
THYROID
FUNCTIONS
DIABETES
MANAGEMENT
ADRENAL
FUNCTION/COSYNTROPIN
STIMULATION
MR#
Interpretation of result by resident
(diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
MR#
Interpretation of result by resident
(diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
MR#
Interpretation of result by resident
(diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
CALCIUM*
RESIDENT NAME:
LABORATORY DATA
THYROID
FUNCTIONS
MR#
Interpretation of result by resident (diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
MR#
Interpretation of result by resident (diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
MR#
Interpretation of result by resident (diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
MR#
Interpretation of result by resident (diagnosis/ management plan)
Comment by supervising attending
(correct/not, missed findings etc)
SIGNATURE of
Supervising attending & DATE
DIABETES
MANAGEMENT
DEXA SCANS SODIUM*
PRINCE GEORGE’S HOSPITAL CENTER
INTERNAL MEDICINE RESIDENCY PROGRAM
ENDOCRINOLOGY OUTPATIENT ATTENDANCE SHEET
RESIDENT NAME______________________________________________
PGY LEVEL_______________ ROTATION MONTH_____________
DATE COMMENTS (IF ANY) BY ATTENDING
SIGNATURE OF
ATTENDING
Outpatient Visits are to be done at the following office:
Dr. F. Sotoudeh
7525 Greenway Center Drive
Ste 209
Greenbelt, MD 20770
Phone: 301-474-0400
Residents must report at 7:30 am every Thursday morning