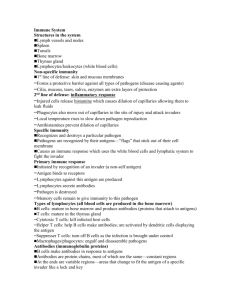
Specific immune defenses
advertisement

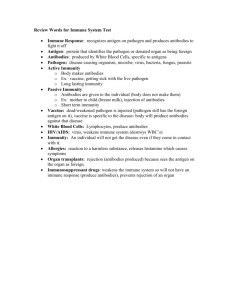
Specific immune defenses and Vaccination I. Overview of specific (acquired) immunity A) Lymphocytes produced in the bone marrow differentiate into B and T cells B cells will eventually produce antibodies (after differentiation to plasma cells) T cells produce lymphokines, which coordinate the immune response B) Macrophages detect foreign antigens, engulf them, and present them to lymphocytes, which initiate specific immune responses C) Lymphocytes which recognize a particular antigen proliferate to produce responder and memory cells, all of which recognize the same antigen (clones) D) Activated B cells differentiate to become plasma cells which secrete large quantities of antibodies E) Activated T lymphocytes differentiate into several different subtypes, each of which either regulates or directly participates in the immune response. II. Major histocompatibility complex: The MHC is a series of genes which code for (i.e. produce) glycoprotein receptors found on cell membranes. The receptors make it possible for the body to distinguish “self” from “non-self”. The MHC’s in a particular person are the result of selection of a small subset of genes available. The more closely related two people are, the closer their MHC complement will be (because they start with a similar set of MHC genes). However, each person has a completely unique MHC complement therefore MHC is a determinant of self. MHC genes are divided into two major classes 1) Class I MHC: Are found on all nucleated cells and are a major determinant of self. 2) Class II MHC: Receptors which regulate immune function. Found on certain white blood cells. Antigen presenting cells (macrophages etc.) display on their surface a combination of antigen and MHC molecules III. T cells are responsible for cell mediated immunity Primarily intracellular parasites (viruses, mycobacterium etc) Immature T cells are produced in the yolk sac, liver, bone marrow (like B cells and all other blood cells) but move to the thymus for maturation. T cells are identified by the receptors (TCR) they possess. These are also known as CD’s for common determinant. Each class of TCR binds specific receptors on other cells. A) What happens to T cells in the thymus (T cell maturation) The immune system must be carefully balanced so that it is neither underactive (AIDS, SCIDS) or overactive (autoimmune diseases such as rheumatoid arthritis, hemolytic anemia, lupus etc.) T cells must be educated as to the difference between “self” and “non-self” T cell maturation (education) occurs in the thymus. As T cells begin to express their randomly generated TCR’s, only cells which are potentially useful are allowed to survive. This selection process results in several possible outcomes 1) TCR’s have no recognition of self MHC (useless) T cell dies 2) TCR’s recognize self MHC and self antigen (autoimmunity) T cell dies 3) TCR’s recognize only self MHC and foreign antigen T cell survives and matures IV. Activation and differentiation of T cells A) Mature T cells are released to bloodstream and lymphoid organs to await presentation of antigen by macrophages B) T cells require two different signals to differentiate 1) Binding of Ag/MHC complex to CD receptors 2) Release of cytokines by antigen presenting cell C) Differentiation leads to production of different classes of T cells 1) T-helper cell 1 (TH1) Expresses CD4 receptors Activated by binding of antigen/MHC-II on APC and release of IL-1, IL-12 Activates more T cells 2) T helper cell 2 (TH2) Expresses CD4 receptors Activated by binding of antigen/MHC-II on APC and release of IL-4, IL-5, IL-6 Helps to attenuate the activity of TH1 cells Causes B cells to proliferate by secreting a number of interleukins 3) T cytotoxic Expresses CD8 Kills foreign cells directly Recognizes foreign proteins on target cells T cytotoxic cells produce proteins called perforins which cause doughnut shaped holes to develop in the cell membrane of the target cell, causing cell lysis Provides much of immunity against virally infected and cancerous cells. Also responsible for graft rejection. 4) Natural killer cells (NK) Related to T cells and respond to many of the same chemical signals NK cells display a natural cytotoxicity against some cancer cells and virally infected cells V. Antibody mediated immunity (B cells) A) B cells responsible for the eventual production of antibodies are formed in the bone marrow in response to hormonal signals. Cells then move to bloodstream and lymphoid organs Because B cells produce large quantities of antibodies, the B cells themselves are found in low numbers in the blood. B) Antibody molecules are proteins made of four distinct regions (Variable, Diversity, Joining and Constant). Each of these regions is coded for by an individual segment of DNA and each region has multiple stretches of DNA which are similar but not identical. During the process of transcribing the mRNA for each antibody molecule, randomly selected V, D, J, and C regions are joined together. This unique mRNA is then translated to produce a unique antibody heavy chain. A similar process occurs to produce the antibody’s light chain. Two heavy chains and two light chains are joined together to form a unique antibody molecule. This process is illustrated in figure 15.5 in your textbook. Read it, know it, love it (well…do the best you can). C) The antibody producing process results in the production of millions of antibodies, each of which has a different variable region while retaining a constant region similar to all other antibody molecules. The variable region is responsible for binding to antigens while the constant region determines the effector cells (macrophages, neutrophils etc.) in the body that can interact with the antibody D) The antibody molecule itself is shaped liked the letter Y. The uppermost tips of the Y make up the variable region. Both variable regions are identical and it is here that antigens bind. The rest of the antibody consists of the constant region, which allows the antibody to bind to various cells of the immune system. Antibodies can also be divided into Fc and Fab regions. The structure of an antibody is illustrated in figure 15.5 of your text. Immunoglobulins (another name for antibodies) are divided into five classes which differ primarily in the FC fragment and the presence and type of accessory molecules. Two different accessory molecules are seen 1) J chain: Joins antibody molecules into multimers (IgA, IgM) 2) Secretory component: Helps move immunoglobulins across mucous membranes Immunoglobulin classes 1) IgG (monomer) 80% of total antibodies Confers long term immunity (memory Ab) Crosses placenta 2) IgA (monomer, dimer) 13% of total antibodies Secretory antibodies (found in tears, saliva, mucous, colostrums) 3) IgM (pentamer) 6% of total antibodies First antibody class produced in response to antigen 4) IgD (monomer) .001% of total antibodies 5) IgE (monomer) 0.002% of total antibodies Involved in allergy and helminth infection E) A few definitions Antigens (Antibody generators): Anything that is perceived by the cell as non-self. Typically proteins such as enzymes, toxins, lipoproteins, glycoproteins. Large (greater than 100,000 MW) and complex (the less repetition the better) molecules make the best antigens. Antigenic determinant (epitope): That small portion of a molecule which reacts with an antibodies antigen binding site. Autoantigens: Molecules to which the immune system has never been exposed, even though they are part of the body. These autoantigens can later be mistaken for foreign molecules, causing autoimmune disease. Alloantigens (isoantigens): Cell surface markers that occur in some members of the same species but not in others. The best example of this is the set of markers which determine blood type (i.e. people have different combinations of A and B markers). F) Antibody response to antigens 1) The Ig receptors on the surface of a B cell recognize a foreign microbe (virus, bacterial cell etc.). The immunoglobulin on the B cell binds to the foreign antigen. This process is known as clonal selection. 2) The foreign antigen is processed by the B cell and displayed on the MHC II complex on the B cell. 3) The B cell must interact with a helper T cell that possesses receptors for the same antigen that was recognized by the B cell. 4) T cell releases interleukins and B cell growth factors, which stimulate the B cells to divide. 5) B cells which have been stimulated multiply to produce a large population of identical cells (clonal expansion) Memory B cells are produced by B cells which do not terminally differentiate Vast majority of B cells differentiate to become antibody producing plasma cells 6) Plasma cells secrete large quantities of antibodies with the same specificity as the original receptor 7) Antibodies bind to all cells expressing the same antigenic determinant as the original antigen. Several outcomes are possible Opsonization: Antigens are coated with antibodies, which makes them more recognizable to phagocytes Agglutination: Antibodies cross-link antigens, again making the antigen more recognizable by clumping them together Neutralization: Antibodies fill surface receptors on viruses or bacterial active sites which prevent the organism from functioning normally 8) Plasma cells eventually die off, leaving only B memory cells, which can quickly produce more antibodies if the same antigen is ever encountered again VI. Classifying immunities Specific immunity can be classified as active or passive, as well as artificial or natural A) Active immunity: A foreign antigen activates B and T cells, causing the body to produce an immune response Essential attribute of an immunocompetent person Creates a memory for fast reaction if re-exposure to the same antigen occurs Requires several days to develop Lasts for a relatively long time (decades, possibly lifetime) B) Passive immunity: Receiving antibodies that were produced in another organism. Provides protection for a short time even though there has been no prior exposure Lack of memory Lack of production of new antibodies Immediate onset of protection Lasts for a short time (months at most) C) Natural immunity: Acquired during normal biological experiences (no medical procedures) D) Artificial immunity: Acquired from medical procedures We can also combine each of the first two categories with each of the last two Natural active: After infection, person is actively resistant to reinfection (getting sick) Natural passive: Occurs when antibodies are passed from mother to child. Two possible routes 1. IgG is able to cross the placenta, providing protection to the newborn child for several months (resistance to tetanus and pertussis is first acquired this way) 2. Breast milk: Provides approximately 1% of all antibodies, particularly IgA, which provides protection against intestinal pathogens such as E. coli and Salmonella Artificial active: Vaccination. Exposure to prepared antigen stimulates the immune system to produce antibodies and lymphocytes which will guard against future exposure Artificial passive: Immunotherapy. Using pooled human serum (horse serum was used in the past) to provide a source of preformed antibodies either to people with weakened immune systems or those in need of immediate immunological protection (e.g. rabies, tetanus, snakebites) VII. Artificial Passive Immunity Immunotherapy refers to the injection of antibodies created in another organism (almost always another human) A. Immune serum globulin (ISG, gamma globulin): Consists of the serum taken from a large pool of healthy donors (generally at least 1000 people) The antibodies found in the serum provide protection against a wide range of diseases Protection last two to three months B. Specific immune globulin (SIG): Serum is taken from a specific group of donors who are recovering from a single disease (pertussis, chickenpox, tetanus). Use to provide increased protection against a single disease. VIII. Artificial Active Immunity A. Vaccination involves exposing a person to a microbe (or portion of a microbe), that is antigenic, but not pathogenic. Stimulating T and B cells will allow the body to mount an anamnestic response if the pathogen is ever encountered. B. Vaccines generally fall into one of four categories 1. Killed whole cells or inactivated viruses Pathogens are killed with formalin or radiation so that antigenicity is not affected. Because dead microbes don’t multiply, larger doses and more boosters are required. Eg. Cholera, plague 2. Live attenuated cells or viruses Pathogens cannot cause disease but retain ability to multiply Attenuation is achieved through long term cultivation, selection of cold mutants or removal of virulence genes Because microbes can multiply in the body, smaller doses and fewer boosters are needed Can be transferred from person to person and may cause infection in immunocompromised patients Eg. Tuberculosis, measles, mumps, chickenpox 3. Subunit vaccines (acellular or subcellular vaccines) Contain only a portion of a cell or virus, which acts as an antigenic determinant (epitope) Toxoid vaccines: contain only a dentured exotoxin. Immunity is raised to the toxin, not the microbe (tetanus, diphtheria) Eg. Pertussis, anthrax, hepatitis B 4. Genetically engineered vaccines Refers to a technique in which a vaccine is created using genetic engineering methods. Trojan horse vaccine: Contains antigenic determinants from many pathogens. DNA vaccines: Contain DNA from a pathogen. The body transcribes and translates the DNA to produce the antigenic protein. C. Potential side effects of vaccination 1. Redness and swelling at site of vaccination, fever 2. Serious reactions (seizures, paraencephalitis, back mutation to a virulent strain) Approximately 1 in 225,000 3. Allergic reactions to eggs or growth media (rare) 4. Contamination of vaccine (also rare) D. Who to vaccinate Herd Immunity: If almost everyone in the population is protected from a disease, even the occasional uninfected person will be safe because there will be no one from whom to catch the disease.