botulinum toxin type-a for the management of the upper limb
advertisement

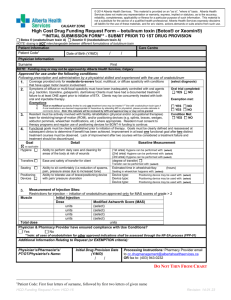
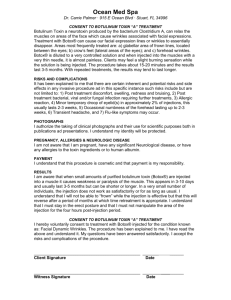
BOTULINUM TOXIN TYPE-A FOR THE MANAGEMENT OF THE UPPER LIMB SPASTICITY IN STROKE PATIENTS. Tasiopoulos N, Zikopoulos K, Sivetidou S. “ANAPLASI” REHABILITATION CENTER, ATHENS, GREECE. INTRODUCTION Spasticity is a very common problem met during the process of a therapeutic rehabilitation program for stroke patients. When localized in lower limbs, spasticity interferes with gait, ambulation, transfers, hygiene, urination and defecation and leads to adoption of bad body postures. When affecting upper limbs it may result in hand deformities, in poor motor improvement, in a decrease of the normal range of motion of the ipsilateral shoulder. Furthermore, spasticity interferes with the therapeutic interventions of the physical and occupational therapists and results in a decreased ability to perform activities of daily living, especially hygiene and dressing. AIM To evaluate the therapeutic effect of botulinum toxin type-A (Dysport) on the spasticity of the upper limb of hemiplegic patients, following a rehabilitation program, on an outpatient basis. MATERIAL AND METHOD Twenty patients suffering from CVA and severe hypertonia of upper limb, were included in the study (12 with Left hemiplegia and 8 with Right) ( MAS score 2). Average age was 63,4. All participants had poor voluntary control and spastic flexion deformity of elbow, wrist and fingers. All patients were following a rehabilitation program, on an outpatient basis, usually on alternate days. Different types of therapy were included, like neuropsychological therapy, speech therapy, physical therapy, occupational therapy, biofeedback, recreational therapy (e.g. basketball inside the therapeutic pool etc). Furthermore, home modifications and adaptations in conjuction with assistive devices were used to enhance function and independence. The assessment of the effectiveness of the treatment was performed by the rehabilitation team members, at regular intervals, therefore establishing coordination of care within the team. All patients were evaluated prior to receiving botulinum toxin and 1 week, 1 month and 3 months after, with: 1. Modified Ashworth Scale (ΜΑS), for the assessment of spasticity 2. Motricity Index, for the assessment of motor deficits 3. Barthel Index (BI), for the assessment of functional abilities 4. Wrist Goniometry, for the measurement of wrist joint range of movement Botulinum toxin was injected under EMG guidance. Total toxin dose was 1500 IU per patient. Toxin in each vial was diluted with 2 ml of injectable solution NaCl (0.9%) and 0.25 ml (60 IU) were administered per site, in 2-3 injection sites per muscle. Muscles injected were pectoralis major, biceps brachii, brachioradialis, flexor carpi ulnaris and radialis, flexor digitorum superficialis and profundus. RESULTS A significant reduction in spasticity and in MAS score (at least one grade in all patients) was found, resulting in functional benefits (mainly in hygiene and dressing) and a reduction in discomfort and pain. The need for administration of antispasticity medication was reduced. Patients were more actively involved in their rehabilitation program. No side effects were observed. 1. Measurements (mean) in Modified Ashworth Scale BEFORE INJECTION Modified Ashworth Scale (mean) 2,45 1 WEEK AFTER 2,00 1 MONTH AFTER 1,85 3 MONTHS AFTER 1,90 2. Measurements (mean) in Barthel Index Barthel Index (mean) BEFORE INJECTION 73 1 WEEK AFTER 79 1 MONTH AFTER 84 3 MONTHS AFTER 89 3. Measurements (mean) in Motricity Index Upper limb Motricity Index 40 BEFORE INJECTION Lower limb Motricity Index 34 1 WEEK AFTER 48 34 1 MONTH AFTER 55 54 3 MONTHS AFTER 60 54 4. Measurements (mean) of active and passive range of movement BEFORE INJECTION Dorsal wrist ROM (mean) ACTIVE 0º Palmar wrist ROM (mean) ACTIVE 10º 1 WEEK AFTER PASSIVE 25º ACTIVE 15º PASSIVE 65º ACTIVE 20º 1 MONTH AFTER PASSIVE 25º ACTIVE 15º PASSIVE 65º ACTIVE 55º 3 MONTHS AFTER PASSIVE 45º ACTIVE 25º PASSIVE 80º ACTIVE 65º PASSIVE 65º PASSIVE 80º DISCUSSION No satisfactory treatment for neurological impairments appearing after a vascular cerebral injury, has been found so far. Therefore, the only remaining choice, is to try to reduce disability by improving patient’s physical abilities, with the help of a well planned rehabilitation program, enriched with a symptomatic pharmaceutical treatment. Spasticity is one of the symptoms of the upper motor neuron syndrome. Potentially, it may become a deteriorating factor for the hemiplegic patient mobility and his functional ability. When localised in lower limbs concomitantly with muscle weakness, spasticity may result in poor ambulation and movement. When localised in upper limbs, spasticity restricts joint mobility and may result in hand deformities, in poor motor improvement, in a decrease of the normal range of motion of the ipsilateral shoulder. Furthermore, spasticity interferes with the therapeutic interventions of the physical and occupational therapists and results in a decreased ability to perform self care activities, especially hygiene and dressing. Spasticity treatment is necessary when a patient feels pain, has a significant impairment of mobility and develops hand deformities and a bad posture. Also, when the activities of self care are poorly performed and when therapeutic interventions of the therapists are difficult to implement. Pharmacological management has not been satisfactory. Anti-spasticity medication (baclofen, dantrolene, diazepam, tizanidine) can be occasionally effective. However, these agents have systemic side effects, including level of consciousness impairment. Selective spasticity treatment would be the ideal approach, to induce patient mobility and functional ability. Botulinum toxin is a neurotoxin produced by the anaerobic bacterium causing botulism. It inhibits acetylcholine release in neuromuscular junction. The therapeutic administration of botulinum toxin, acts selectively in the specific muscles that cause inability to the patient and achieves selective suppression of spasticity. It is a useful symptomatic treatment. However, it creates a brief temporary time window of reduced spasticity, facilitating therefore the work and increasing the efficacy of interventions of the therapists. Thus, botulinum toxin treatment should be part of a comprehensive rehabilitation program and should be administered only when the patient is following a rehabilitation program, that continues after the botulinum toxin administration. In such a rehabilitation program, a daily routine of prolonged muscle stretching, strengthening exercises, coordination exercises, occupational therapy, biofeeback, splint application etc. may be included. Our patients followed such a rehabilitation program. They presented a significant impairment in mobility and performance of daily activities, due to severe upper limb spasticity, and all of them have been following a rehabilitation program, that was continued after the botulinum toxin treatment. Already from the first week after toxin treatment, an apparent reduction of spasticity and an improvement of self care ability were noticed. Furthermore, we noticed a reduction of MAS index score, an increase of patients’ ability to perform self care activities (hygiene and lower limb dressing), an increase of BI score and a decrease in the need for anti-spasticity medication. All patients showed a more active participation in their rehabilitation program. This improvement lasted for three months. After this period, spasticity started to worsen, but the functional abilities of the patients had already improved significantly. CONCLUSION Local injections of botulinum toxin type-A can provide a significant relief of the upper limb spasticity in stroke patients, enhancing their functional abilities to perform self care activities and facilitating their rehabilitation program.