IMMUNE INFLAMMATORY ATTACKS AND UNSTABLE
advertisement

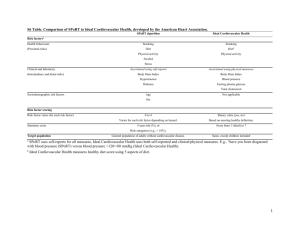
IMMUNE INFLAMMATORY ATTACKS AND UNSTABLE CARDIOVASCULAR PATHOMORPHOSIS. VERIFICATION AND COUNTERACTION. Andriyevskikh I.A., Lukin O.P., Davydov I.V. Chelyabinsk State Medical Academy and Chelyabinsk Federal Center of Cardiovascular Surgery. Hospital surgery department. Russia. MD. PROF. ANDRIYEVSKIKH I.A Abstract The research into the peculiarities of the influence of immune inflammation on the formation of severe forms of cardiovascular diseases, developed by patients, who had a major cardiovascular operation, has been conducted by the authors of this paper. Significant shifts in the patients’ immune status have been detected. The criteria of unstable cardiovascular pathomorphosis have been established. The methods of immunodiagnostics and immunotherapy of such conditions have been worked out. Due to the use of these additional methods the number of intra- and post- operative complications can be reduced by 13,4%. Key words : immune inflammation; unstable cardiovascular pathomorphosis; cardiovascular operations. Topicality. Considerable influence of immune inflammation on the formation of severe forms of cardiovascular pathology is completely proven [1,3,8,11,13,14,16]. However, optimal verification criteria of this negative influence on cardiovascular catastrophes ( provided that patients undergo major cardiovascular operations) and counteraction methods to this pathological component have not been determined yet. Present day standards and algorithms do not include evaluation methods of total immune status or immunotherapy of patients with the hard course of cardiovascular diseases and risky surgical care. Our paper focuses on this urgent problem. Materials and methods. The research is conducted on 492 patients with severe forms of cardiovascular pathomorphosis. These patients were getting surgical care in different arterial pools of our clinic from 2005 to 2010. The average patient’s age was 54,9 ± 11,2years. There were 94,5% of men and 5,5% of women. 50,6% of patients had heart ischemia as the main disease. 73,8% of patients had multivasal damages. All patients with multivasal damages simultaneously had ischemic heart, brain and limbs disorders. 63,4% of patients were under conditions of comorbidity with accompanying pathology of the gastrointestinal tract, lungs, kidneys, endocrinopathy and autoimmune diseases. The common standard methods , such as ACS and MCS, intimectomy from the branches of the aortic arch and branchycephalic trunk prosthetics, surgical operations on visceral and renal arteries, aorto-femoral and femoral-popliteal shuntings were used to cure such patients. We referred all such cases to the group of patients with unstable cardiovascular pathomorphosis. Sign We regarded unstable cardiovascular pathomorphosis as availability of clinical and laboratory-instrumental data, manifesting predominance of the immune inflammatory component over the adaptation component, which was accompanied by rapid progress of ischemic disorders n different arterial pools, also by tolerance to the total amount of traditional treatment and threat of sudden thrombo-hemorrhagic complications. We believe that the clinical markers of unstable cardiovascular pathomorphosis are as following: multivasal damages, comorbidity as a whole complex of interrelated pathologies with marked aggravations, endocrinopathy and connective-tissue dysplasia. On the basis of our research and considering the data, obtained by other authors, we worked out a therapeuticdiagnostic algorithm, which reveals the marked immune inflammatory component of cardiovascular bed. Besides, we established the principles of individualized immunotherapy, applied to such seriously ill patients. The algorithm is as follows: If patients are examined by standard methods, which detect direct and indirect indications of predominance of the immune inflammatory component of cardiovascular bed over compensation reparative component, in this case we carried out additional immunodiagnostics and immunotherapy. This method was worked out on the basis of the preliminary discrete analyses of clinical laboratory data, collected on 119 patients with cardiovascular diseases during a certain period of time prior to this research. For integral analyses we used a score system, whose principle we present in the Table 1. Table 1. Principle of integral assessment of the presence of immune inflammatory component of cardiovascular bed. Index Score Indirect Direct Connective-tissue dysplasia 0,5 Relative's cardiovascular diseases 0,5 Rapid course (days, weeks) occlusive, stenotic or degenerative changes in vascular walls and cardiac valve structures 0,5 Distal and diffuse damages of cardiovascular bed 0,5 Heightened ESR 1,0 Leukocytosis with deviation of the differential count to the left 1,0 Increased СRP rate 1,0 Thrombocytopenia 1,0 The predominance of the immune inflammatory component was confirmed if the total sum exceeded 3 scores. In this case in order to determine the presence of inflammation and the direction of immunotherapy, we tested the patient’s immune status in the laboratory conditions. This laboratory examination included the characteristic of cell link of the immunity (absolute quantity of lymphocytes, CD3, CD4, CD8, CD 10, CD11в, CD16, CD20, CD25. CD34, CD56, CD95, HLA-DR), humoral link of the immunity (immunoglobulins А, М, G, Е, circulating immune complexes, СН50, С3 и С5 components of complement in the blood serum); phagocytic neutrophils activity of peripheral blood (the quantity of cells taking part in phagocytosis, phagocytic index, phagocytic number and the state of redox processes in neutrophils and the test, stimulating them [7,12]. The most characteristic immunologic signs of the presence of immuno-inflammatory cardiovascular attack were as following: the increased number of immunoglobulins A and G in the blood serum, circulating immune complexes, E immunoglobulin reduction, activation (in case of aggravation) of oxygen –dependent metabolic processes in neutrophils and the presence of immune deficiency with phagocytosis disorders predominating (80-85%). More seldom there occurred changes in the cell link of the immunity (45-50%). The detection of these divergences in the immunogram was an additional confirmation of the discrete analysis results, which allowed us to make final score assessment in accordance with the above mentioned chart. The course of immunotherapy was 15-20 days on average, but never longer than 30 days. The main principle of the prescription of immunotropic medicines for immuneinflammatory component stabilization was the recovery of redox processes in immuno-competent cells. If the index of the neutrophil stimulating test was pushed up, we prescribed intravenous droplet ejection of antioxidants: polioksidony ( if Index CD3,% CD4,% CD8,% CD11,% CD16,% CD95,% HLA-DR,% PhN of neutrophils, conv. units Spontaneous NBT-test,% Induced NBT-test,% IgA, г/л IgM, г/л IgG, г/л CIC, unit опт. density CH50, conv. units ESR , mm/h Leukocyte number, ×109/l Eosinophils,% high rates of immunoglobulins and circulating immune complexes were simultaneously registered) or emoksipin (in cases of isolated breaches of antioxidant defence), besides, discrete plasmapheresis was applied to 178 patients of the 1 st group. In case of decreasing neutrophils stimulating test index we used intravenous injection of glutoxim. In case of the low phagocytic activity rate and lack of immunoglobulin G we used intravenous injection of human polyvalent immunoglobulin (with 108 patients of the 1st group). Since the end of the first week of treatment we added immunomodulators (for all our patients of the 1st group) with the aim of further immune status harmonization (Immunofan , Vobenzim, Licopid, vitamin А etc.). As complex immunotherapy depended on the patient’s individual characteristics of the immune status, the combination of immunotherapy remedies was also individual. This algorithm was used for the patients of the 1 st group, to other patients (2nd group) only traditional methods of diagnostics and preoperative preparation were applied before putting into practice this algorithm. The patients of the both groups were randomized according to the type of the pathology, surgical treatment methods, gender and age. When assessing the immune status of the patients of the 1st group we were guided by regional standard requirements for a normal immune status of Chelyabinsk and Chelyabinsk region residents[2]. During the preoperative period all the patients of the 1 st group got individualized immunotherapy, based on the peculiarities of clinical-laboratory immunodeficiency manifestations. Results. After immunotherapy we got positive dynamics of the immune state change with the patients of the 1st group. This dynamics is shown in Table 2. Table 2. Divergences in the immune status and immunotherapy effectiveness (M±m) with 277 patients of the 1st group. Before therapy After therapy 37,31±2,56 38,69±1,06 25,52±1,78 27,71±1,34 21,5±1,31 23,5±0,941 16,5±1,29 16,84±0,81 14,65±0,81 17,31±0,61 19,41±1,61 19,22±0,97 14,54±1,32 14,75±1,66 3,44±0,26 3,45±0,29 27,21±2,1 27,58±1,34 36,53±2,36 38,12±1,24 1,83±1,33 1,78±1,16 1,08±0,05 1,05±0,045 8,43±0,26 8,12±0,41 97,32±8,87 92,32±4,57 61,78±1,99 59,18±1,16 24,11±2,27 11,71±3,59 15,59±3,31 11,34±2,17 9,10±0,64 7,02±0,85 p 0,027* 0,048* 0,040* 0,048* 0,035* 0,050 0,112 0,084 0,048* 0,033* 0,652 0,043* 0,050 0,049* 0,019* 0,306 0,191 0,121 Stab neutrophils,% СRP, mg/l 11,85±2,77 8,71±,1,26 Note: Valid distinctions (p <0.05) are marked *. Our next step was to compare the number of intra- and postoperative thrombo-hemorrhagic 8,31±1,12 6,25±0,26 0,146 0,042* and reparative complications in both the groups of patients. This is shown in Table 3. Table 3. Types of operative interventions and peculiarities of intraoperative unstable pathomorphosis manifestations I st group II nd group n =277 n =215 Types of operations CS and CABG Operative interventions on brachycephalic arteries Aorto-femoral and femoralpopliteal shuntings Intervention ons on visceral branches of aorta TOTAL Thrombosis of shunts Diffuse hemorrh age Incision of the vessel suture Total of operated patients/ complication s (%) 4 8 10 133/16,5 - 1 2 3 6 7 Diffuse hemorrhage Incision of the vessel suture Total of operated patients/ complication s 16 21 22 116/42,2 50/6 - 4 7 41/26,8 7 77/20,7 8 14 18 46/86,9 1 1 17/11,7 1 4 3 12/66,6 16 20 277/15,5 25 43 50 215/54,8 All the above mentioned complications in both the groups of patients were overcome due to local hemostatic means, using of sutures on pads and thrombectomy. Therefore, in Thrombosis of shunts the 1st group there were considerably fewer complications after the immunotherapy. This is shown in Table 4. Table 4. Patient’s distribution according to the character of postoperative complications in the 1st experimental group and the IInd group for comparison I group II group n =277 n =215 Total of Total of operated Types of PurulentPurulentoperated Acute patients/ Acute interventions Multiorgan septic Multiorgan septic patients/ heart complication heart insufficiency complicati insufficiency complicatio complications failure s failure ons ns (%) (%) ACS and CABG Operative interventions on brachycephalic arteries Aorto-femoral and femoral-popliteal shuntings Interventions on visceral branches of aorta TOTAL 5 2 3 - 1 - - 1 7 1 1 6 5 133/7,5 9 7 4 - 3 1 77/10,3 1 2 12 46/32,6 1 17/17,6 1 2 2 12/41,6 11 277/9,4 11 14 19 215/20,4 50/2 None of the patients in both groups died during the intraoperative period. During the postoperative period 22 (9,4%) patients of the experimental main group and 44 (20,4%) patients in the 2nd comparative group developed hemorrhagic and reparative complications. In the majority of cases we cured these complications with the help of traditional methods of treatment. Nevertheless, 2 (0,7%) patients of the experimental main group and 7 (3,2%) patients in the 2 nd comparative group died from heart failure or multiorgan insufficiency. 116/17,2 41/9,7 Discussion: There remains a lot of problems to solve in the present day immunodiagnostics and immunotherapy of cardiovascular pathology [3,5,9,11]. However, the obtained new data on the cell-molecular level of many pathological states give hope for evolving more effective and selective methods of influence on the immune component of severe forms of cardiovascular pathomorphosis [4,6,7,8,17,18]. The majority of present day medicines, used for cardiovascular pathology treatment, influence only separate links of pathogenesis. Immunotherapy has a lot of advantages over traditional medical care due to its simultaneous influence on the key moments of the main pathogenetic links in cell-humoral associations [3,13,15]. Therefore, we believe that due to immunotherapy it is possible to raise the level of phagocytosis of this group of seriously ill patients. So far, methods of immunodiagnostics and immunotherapy are put into clinical practice with difficulty because of their systemic, nonselective influence. Nevertheless, simultaneous organism-molecular synthesis of data [3,6,10,14] and medical proficiency in the analysis and synthesis of data according to general pathological principles, angiology peculiarities, functions of monocyte- macrophage system and immune status assessment allow to achieve good success [2,3,8,12]. The data, which we obtained, give a good chance to look with optimism upon the perspective of developing this trend of medical science. 6. 7. 8. 9. 10. Conclusion: 1. It is advisable to single out patients with the hard course of cardiovascular pathology into a separate group of unstable cardiovascular pathomorphosis. 2. In the overwhelming majority of cases patients with unstable cardiovascular pathomorphosis evince marked immune inflammation of cardiovascular bed. 3. The immunogram of this status of patients allows to determine individual peculiarities of the secondary immunodeficiency. 4. Individualized immunotherapy for the patients with unstable cardiovascular pathomorphosis gives the patients effective defence against sudden cardiovascular catastrophes and surgical aggression. 11. 12. 13. References: 1. 2. 3. 4. 5. Anikin, V.V. Immunotherapy as a means of raising nitrates effectiveness in stenocardia treatment / V. V. Anikin , A. А. Mikhailenko,R . V. Mayorov // Rossiysky kardiologuichesky journal: nauchno-praktichesky meditsinsky journal . — 2010 . — N 5 . — P. 73-76 . Dolgushin I.I.., Selyanina G.A., Kolesnikov O.L., Dodonov N.P. Normative immune status indexes of Chelyabinsk region residents. //Chelyabinsk, Pub.H. «ChelGMA», 2008.- 23 p. Karaulov, A.V. Molecular medicine and clinical immunology. Clinical immunology and allergology successes. Vol.3.-2002.-. -P.3-5. Morozov, S. U. Immunotherapy and principles of appliance / S. U. Morozov // Rossiysky meditsinsky journal . — 2008 . -Vol. 16.-N4. - P. 242-244. Teplyakov, А.Т., Suppressive influence of recombinational immunomodulator roncoleukin on the level of proinflammatory cytokins, auto-antibodies to cardiolipin in blood and heart falure./ А.Т. Тeplyakov, L.А. Bolotskaya, 14. 15. 16. 17. 18. Т.А. Stepacheva, N.V. Кaraman, Е.V. Rybalchenko, S.N. Shilov, А.P. Маslov//Kardiologia. -2008.-Vol.48.-P.34-40. Khaitov, R.М. Immunodiagnostics and immunotherapy of immune system disorders / R.М. Khaitov, B.V. Pineguin // Praktikuyushy vratch.- 1997.-№ 9.-P. 9-13 Khaidukov S. V. Broadening the opportunities of the method of flowing cytometry fer clinical immunology practice / S.V. Khaidukov , А.V. Zurochka, V.А. // Меditsinskaya immunologia,- 2008. -Vol. 10(1). -P. 5— 12. Tsinkelnagel, R.М. Selected articles / Ed. V.А. Chereshneva, G.А. Bocharova, I.А. Тyuzankina. – Ekaterinberg, 2003. – 122 p. Charnaya, М. А. System of hemostasis change at operations on aorta in the conditions of artificial blood circulation./М.А. Charnaya, U.А. Morozov, V.G. Gladysheva, Е.V. Roitsan, А.М. Isayeva, U.V. Belov, А.V. Goncharova // Angiologia e sosudistaya khirurgia. – Vol.11.-№3. -2005.-P.27-31. Caughey, G.E. Comorbid chronic diseases, discordant impact on mortality in older people: a 14-year longitudinal population study / G.E. Caughey, E.N. Ramsay, A.I.Vitry, A.L.Gilbert, M.A.Luszcz, P.Ryan, E.E Roughead.// J Epidemiol Community Health.- 2010.- Dec. Vol.64(12).-Р. 1036-42 Chironi G., Pagnoux C., Simon A., Pasquinelli-Balice M., Del-Pino M., Gariepy J., Guillevin L. Increased prevalence of subclinical atherosclerosis in patients with small-vessel vasculitis. // Heart. – 2007. – Vol. 93. – № 1. – P. 96–99. Claude, L. Enumeration of peripheral lymphocyte subsets using 6 vs. 4 color staining: a clinical evaluation of new flowcytometer/ L.Claude, C. Lobagiu, C. Genin // Cytometry. Pt B.-2005. -Vol. 70B. - P. 29—38. Cohen, S. New interpretation of vasculitis in the light of evolution / S. Cohen // Am. J. Med. Sci. – 2008. – Vol. 335 (6). – P. 469-746. Derksen, R. Management of the obstetric antiphospholipid syndrome / R. Derksen, M.A. Khamashta, D.W. Branch // Arthritis. Rheum. – 2004. – Vol. 50. – P. 1028-1039. Fichtlscherer, S. Inhibition of cytochrome P450 2C9 improves endothelium-dependent, nitric oxide-mediated vasodilatation in patients with coronary artery disease / S. Fichtlscherer, S. Dimmeler, S. Breuer et al. // Circulation. – 2004. – Vol. 109 (2). – P. 178-183. Libby P. Changing concepts of atherosclerosis. / Libby P. // О. Intern. Med PubMed.– 2000.– 247.– P. P. 349-358. Maksimowicz-McKinnon, K. Limitations of therapy and a guarded prognosis in an American cohort of Takayasu arteritis patients / K. Maksimowicz-McKinnon, T.M. Clark, G.S. Hoffman // Arthritis Rheum. – 2007. – Vol. 56, № 3. – P. 1000-1009. Nishimoto, N. Successful Treatment of a Patient With Takayasu Arteritis Using a Humanized Anti-Interleukin-6 Receptor Antibody / N. Nishimoto // Arthritis Rheum. – 2008. – Vol. 58, №. 4. – P. 1197-1200.