Medication Administration - Madawaska Valley Association for
advertisement

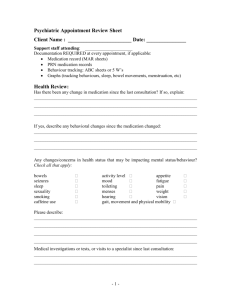
1 Madawaska Valley Association for Community Living MEDICATION ADMINISTRATION POLICY STATEMENT: Madawaska Valley Association for Community Living will administer medications to those individuals it serves. Principles: 1. All medication and treatments administered by MVACL staff are given only if ordered by a doctor. 2. All medication will be reviewed on an annual basis, or more frequently, as recommended by the individuals' physician or on the recommendation of a manager or direct support staff. A continuous effort shall be made to reduce unnecessary medication through consultation with the individual's physician, family, and direct support staff. Each individual has the right to regular medication review by his or her personal physician. These are typically done at the annual exam. Reviews should be documented in the individual's medical records. 3. Full-time support workers are responsible for ensuring that necessary blood work is completed, particularly with relation to medication levels. 4. The Individual's health and safety shall be the primary concern when administering, monitoring and storing medications. 5. Every effort should be made to increase each individual’s understanding of the medications they are taking and, where appropriate, to provide the necessary training directed towards the independent administration of these medications. 6. Medication changes will be implemented only upon written order from the physician. 7. STANDARD TIMES: q.d., od - Once a day b.i.d. Twice a day t.i.d. Three times a day q.i.d Four times a day 8 a.m. (0800 hrs) or 8 p.m.. (2000 hrs) 8 a.m. (0800 hrs) and 8 p.m. (2000 hrs) 8 a.m., 4 p.m. (1600 hrs) and 8 p.m. 8 a.m.,12 noon (1200 hrs), 4 p.m. and 8 p.m. 8. Exceptions to these times are: when doctor’s orders indicate a specific time when medication indicates a need such as “with meals” (e.g. antibiotics) 2 TRAINING: All support staff are responsible for the administration of medication to the individuals they support. All staff will be given training pertaining to medication administration during orientation. This training will include a review of the Medication Policy, orientation to blister packs, MAR sheets, and personal binders. Once this training is complete an experienced staff member will observe (shadow) the new staff when he/she first administers medication. This must be done before new staff can administer on his/her own. Repeat "shadowing" may be requested if necessary by the Manager and or support worker. Once the new staff, the manager and the shadow staff are satisfied with the performance of the new staff, the new staff member will then sign off on the Medication Orientation sheet which will become part of their employment file. MEDICATION ADMINISTRATION It is the responsibility of all support workers to make themselves aware of any medical cautions including allergies. All staff shall obtain medication information (knowledge of drug) from the Personal Binder (see Drug Info sheets from pharmacy), Drug Book, the Internet, CPS or pharmacist/doctor. The person responsible for administering medication must: follow proper procedures related to medication delivery have knowledge of the actions of the drug, possible side effects and any precautions to be taken ensure the medication cupboard is locked at all times when not in use and keep the key in a safe place. check in all medications that arrive during their shift if no Full-time staff is present. These must be documented on the MAR sheet and on the Med Profile in the individual’s binder. New meds should also be noted in the logbook and on the whiteboard. Ensure that there is a drug information sheet (supplied by the pharmacy) filed in the drug info section for each medication the person is on. Staff are required to report to a manager any omissions, errors or concerns related to medications. All errors/omissions must be recorded on an incident report within 24 hours and reported to a manager as soon after the error as possible. 3 ASSOCIATION STANDARDS FOR MEDICATION DELIVERY PERSONAL BINDER, Medication Administration Section Each individual has their own binder with a Medication Administration section that contains: - Medication Profile - MAR Sheet(s) - PRN Record - Doctor’s Standing Order Sheet The Medication Profile lists every medication an individual is currently on. It includes the start and end date of every prescription. It also includes a brief description of why it is taken. The full time staff hand in the Profile each January (for filing) and start a new one for the current year. The new one includes only current medication, not those that have been discontinued. The MAR sheet is the Medication Administration Record which lists all the medication an individual takes, and provides space for recording each dose that has been administered. Note the yellow box in the top right corner which indicates any allergies. Also note that each staff must sign their full name once a month on every MAR sheet that they will initial during that month. The PRN Record is used to sign off for medication given only on an ‘as needed’ basis. You sign off on the MAR sheet with just your initials and the time in the column for that date. You then provide the details on the PRN record. It is imperative that the PRN record be carefully completed at the time of administration. It must include the reason for administering the drug with some detail, e.g. “Complaining of headache for last 90 minutes”, or “anxious, unable to sleep and pacing”. An hour after administration (or a reasonable period of time later, depending on the medication), the person who gave the drug must assess the effectiveness and record this in the appropriate space, under “Observations/Effect”. If this person is unavailable s/he must hand off this responsibility to another staff after providing sufficient background information. You must accurately record the dose, on the PRN record e.g. Lorazepam 2mg. 2 tablets given or Lorazepam 2mg. 1 tablet given. The Doctor’s Standing Order Sheet is completed by the physician each year at the annual exam. It includes a list of prn medications (some over the counter drugs) that people may use for standard problems such as headache, constipation, cough, etc. Remember, we can give nothing without an order. This allows us to give an individual Tylenol for a headache without having to contact a doctor (given that it is included on the Standing Order Sheet). It should not include drugs that someone ‘might’ use. If a drug hasn’t been used in a year, you may consider excluding it from the Standing Orders the next year. 4 STANDARDS 1) All medications (except liquids, topicals, and Tylenol plain) will come from the pharmacy in bubble packs clearly labelled with the individual’s name, prescription, dosage, times and prescribing physician. 2) Bubble packs include all prescribed medications to be given on a regular basis for a one week period beginning on Sunday and ending on Saturday. Bubble packs will be ready for pick-up at the pharmacy by Thursday noon for the week beginning on Saturday. Please note that narcotics will be bubble packed separately and the label is light mauve. 3) The Full-time or designated support staff is responsible for checking the MAR sheet (medication administration record) provided by the pharmacy against the Medication Profile found in the Personal Binder. Once it has been determined that all required medications are included on the MAR sheet, each bubble pack will be checked against the MAR sheet to ensure it includes the correct dose and amount. 4) In the rare event that there has been a verbal order from the doctor over the phone and it is discovered that the change has not been made on the MAR sheet, staff will complete a physician’s order form indicating the required changes. The form will be faxed to the doctor who will fax it back to MVACL. Staff will then take this to the pharmacy so the MAR sheet can be corrected for the next month. 5) Designated staff will colour code MAR sheets after checking them when they arrive from pharmacy. Please see page 11 under “charting”. It is necessary to always use a ruler. PRN meds will also have ”PRN” written and highlighted green, in the medication column beside drugs which are to be given PRN. 6) When accompanying an individual to a medical appointment, the Full-time staff (or when absent, designate) will ensure that a Physician’s Order form is completed if any changes are made to the person’s medications. Staff are responsible for assisting the individual to take the order to the pharmacy to be filled. 7) Staff will then document the medication change a. on the individual’s Medication Profile in their personal binder, b. on the individual’s MAR sheet c. in the logbook d. on the white board. 8) Staff will also fill out the Med Treatment form and provide all necessary information from the appointment. 9) Medication that needs to be kept in the fridge, will be kept in a locked storage container, which can be obtained at the Administration Office. Talk to your manager and s/he will provide you with one. 10) At the end of the month completed MAR sheets will be filed in the appropriate binder section. Remove all perforated tabs and carbon copies. 11) MAR sheets will be submitted to the manager annually for filing. 12) All discontinued medication will be brought to the pharmacy to be discarded in the safest, most environmentally friendly manner. 13) Expiry dates on all bottled medications will be checked monthly and shall be replaced accordingly. 5 PROCEDURE FOR MEDICATION ADMINISTRATION Objective: To administer the correct drug to the correct person in the correct dose at the correct time using the correct route (method of administration) and correct charting. 1. One staff member per shift will be responsible for administering medication. 2. Always review the entire MAR sheet before administering any medication to ensure all meds are given correctly. 3. All medications will be prepared and administered in a distraction-free area. 4. Medications should be administered as close to the designated time as possible, however, they may be given up to one hour before or one hour after. This ensures a stable blood level of the drug. Medication given before or after the allotted one hour should be considered an omission/error and be reported as such. 5. Staff will ensure that proper hygienic procedures are used when preparing and delivering medications (i.e. wash hands before and in between each individual's medication delivery). All equipment shall be cleaned after use (spoons, droppers, med cups etc.). 6. Staff will ensure that the “correct six” (6) are followed: correct person, correct drug, correct dose, correct time, correct route, correct charting. 7. The staff who administers medication must "sign off" promptly afterward. 8. Staff will review the appropriate delivery techniques and administer the med. accordingly. The individual will be asked to go to where the medication will be administered. Staff are not to dispense meds where distractions may occur. 9. Staff must be sure the medication has been swallowed. A mouth check may be done as well if indicated on the MAR sheet. 10. Staff will sign the appropriate place on the MAR sheet immediately after (not before), the delivery of the medication, verifying the ingestion of the appropriate medication by the specific individual at the correct time. 11. Staff will ensure that medication is NEVER dispensed by one person and administered by another. Medication is given directly after being dispensed. Medications must never be dispensed for more than one person at a time. 12. All medications, which are dropped, contaminated or discontinued, are to be placed in a pill bottle, zip lock bag, or other appropriate container clearly labelled “Contaminated meds”. They will be taken to the pharmacy to be destroyed. Please make a note of this in the Log Notes under “Shift Concerns”. 6 13. When a pill is contaminated, staff will carefully take the exact pill from the Saturday bubble and administer it. They will then tape the Saturday bubble closed and communicate the need for a replacement pill to the full time staff responsible for the individual’s medical care, promptly and clearly. If this happens on a Saturday, take the pill from Saturday of the Bubble Pack for the next week and proceed as above. 14. Individual’s who plan to be absent or are on L.O.A. (leave of absence) will have the bubbles for the times they will be absent detached along the perforated lines. Responsibility for administering these meds will be handed over to a caregiver when applicable. LOA will be written on the MAR sheets for the periods when the individual was away, as we cannot sign for meds we do not give. 15. Before administering any medication, be aware of indications, contradictions, precautions, adverse effects, overdose symptoms, etc. for that medication. This information is available on the drug information sheets from the pharmacy. 16. Individuals who are capable may self-administer medication but must have a documented procedure outlined in an Individual Training Plan and should be supervised. 7 INSTRUCTIONS FOR ADMINISTERING VARIOUS FORMATS OF MEDICATION Bubble packaged pills: Ensure the prescription label on pack matches the MAR sheet Ensure that pills in bubble match description on pack (colour, number, etc.) Dispense pill directly to individual or into medication cup Give pill for self-administration or place in individual’s mouth Observe that the pill has been swallowed PRN Medication: PRN (given as necessary) or Non-prescription medication may not be administered without a Doctors Order (this includes Tums, Tylenol/Aspirin, Vitamins, Cough Syrup etc.) Any ‘prns’ you may administer should be included on the Doctor’s Standing Order sheet. All procedures for administering prescription medication apply to the administration of nonprescription medication. When administering a non-prescription medication with a standing order, the staff person should follow the directions on the bottle. If necessary, contact the physician for clarification. Before administering a non-prescription medication, the staff person should be aware of all the individual's present medication and should consult the C.P.S. for any possible contraindications*. All PRN medication administered will be recorded on the MAR sheet and on the PRN Record. It is imperative that the PRN record be carefully completed at the time of administration. It must include the reason for administering the drug with some detail, e.g. “Complaining of headache for last 90 minutes”, or “anxious, unable to sleep and pacing”. An hour after administration (or a reasonable period of time later, depending on the medication), the person who gave the drug must assess the effectiveness and record this in the appropriate space, under “Observations/Effect”. If this person is unavailable s/he must hand off this responsibility to another staff after providing sufficient background information. You must accurately record the dose, on the PRN record e.g. Lorazepam 2mg. 2 tablets given or Lorazepam 2mg. 1 tablet given. When signing off a PRN, on the MAR sheet, include only your initials and the time in the column for that date. There should be no times written in the hours column of a PRN medication, on the MAR sheet. Note: *Contraindications are conditions under which it is not advisable to administer a drug 8 Bottled liquid or pills: (Always read all instructions on the bottle) Ensure that the prescription label matches the MAR sheet Check individual’s name on bottle, name of medication on bottle and dosage When pouring liquid medicine into a spoon, use a house hold measuring spoon or medicine spoon obtained from the pharmacy. When pouring liquid medicine into a medicine glass, place the glass on a level surface and pour the medicine at eye level. The quantity is read when the lowest part of the concave surface of the fluid is on mark on the medicine glass. Always hold the bottle with the label touching the palm of the hand to avoid soiling the label. When liquids have been poured wipe the mouth of the bottle with a clean cloth to eliminate any residue. Use a pill cutter where it is necessary to dispense a partial tablet Lotions and Ointments: (Always read instructions on container) Always wash your hands before you begin the procedure and wear protective gloves. Lotions and ointments are best applied gently in small amounts by patting rather than rubbing. If skin is itchy, apply with a firm stroke; dabbing increases itchiness. Ointments should be removed from jars with a cotton swab applicator, never with fingers, so remaining contents are not contaminated. Take only required amounts. Eye Drops and Ointments: (Read instructions) Always wash your hands before the procedure and wear protective gloves. When administering eye drops or ointment use only prepared Ophthalmic drugs. Have tissue and drops ready. Place drops in the centre of and behind lower eyelid. The eyedropper bottle or ointment tube should never touch the eye membranes. Instruct the individual to look up. Head should never be tilted back. With one hand, hold eyelids open, resting top eyelid on upper bony part of eye socket and lower lid on lower bony part to eye socket. With other hand instil the prescribed number of drops in centre of and behind the lower eyelid. Instruct the individual to close eyes gently but not to squeeze. Wipe excess drops and tears from cheek with tissue. To apply eye ointment, place in between the eye and lower lid. Apply moving in direction from the nose side to the outer margin of the eye. 9 Ear Drops: (Read instructions) Always wash your hands before you begin the procedure and wear protective gloves. When administrating eardrops, instruct the individual to tilt their head with the affected ear up. Instil the prescribed number of drops. Keep the head tilted for five (5) to ten (10) seconds to allow absorption to take place. Absorbent cotton may be placed at the opening of the ear canal. Suppositories: (Read instructions) Always wash your hands before you begin the procedure. Put on protective gloves or a finger cot. Always provide privacy and reassurance for the individual. Rectal suppositories should be administered with the individual lying in a knee to chest position or side lying position. Lubricate the suppository with Vaseline. Separate the buttocks. Identify the rectum. With the suppository between thumb and forefinger, insert into rectum with formed tapered end first. With index finger push suppository past the internal sphincter (to second knuckle of index finger). Vaginal Suppositories are to be administered according to package directions, again ensuring that your hands are washed and protective gloves are used. L.O.A. (Leave Of Absence) Medications: ALL necessary medication is to be given to the responsible person with direction. If leave is with staff, the binder will accompany the individual. If leave is with family or friends, simply detach the necessary doses and chart LOA on the MAR sheet. 10 RECORD KEEPING Record keeping is the responsibility of the staff who administers a medication and will be monitored regularly by Full-time staff. Medication record keeping should include: 1) Personal Binder, Medication Administration section- consisting of: a) Medication Profile – list of all current medications, administration information. b) MAR sheet(s). These list all medications being used and the times they are given. This sheet should be initialled using only black or blue ink as meds are given. The medication administrator's signature in black or blue ink should appear once on this page. Discontinued medications should be stroked out with a single line using red ink and a ruler and must be dated and initialled. c) PRN Record – To provide more information on the use of PRN medication such as, reason the drug was given and the effect it had. d) Dr’s Standing Orders – Provides a list of over-the-counter drugs which may be administered on a PRN basis. e) Drug information – specific information pertaining to each drug. 2) The Log Book - All new medication, discontinued meds and med errors should be recorded here by the staff. The manager is to be informed of all of the above. ERRORS AND OMISSIONS: All medications are prescribed by doctors and are necessary to maintain the health of individuals. The administration of medication to individuals is an extremely important responsibility of support staff and must always be dealt with in a serious manner. Any administration of medication which is not in compliance with MVACL’s med policy will be considered an error. Errors include: Failure to administer medication. Administration of the wrong drug. Administration of the wrong dose. Administration to the wrong individual. Medication administered at the wrong time. Medication administered by the wrong route. (e.g. gave a topical medication orally) Failure to sign for an administered medication. Signing incorrectly. In the event that a medication error is made, Support Staff should proceed as follows: a) Contact staff involved from previous shift to discuss incident and get all relevant information (i.e. – confirm that meds given/not given) b) During business hours: contact your manager for further direction. c) After business hours: Discuss the error with the Full-time staff at your location. If no full-time staff is available, contact your manager. A decision will be made as to whether to contact the pharmacy or a medical professional. If there is any doubt, seek advice as to how to proceed. d) Follow advice given by pharmacy and/or medical professional. An Incident Report must be completed within 24 hours and forwarded to a manager. 11 CHARTING a) All Charting must be done in black or blue ink. b) Use red ink to indicate “discontinued” or “failure to sign”. c) “Failure to sign”- circle box without signature in red. Notify staff person involved. Staff who erred will sign (when next in on shift) in green ink. d) Any errors in charting must be reported. e) Corrective material (i.e. white out) must never be used on the MAR Sheet. f) It is always necessary to use a ruler. g) PRN meds will also have ”PRN” written and highlighted green, in the medication column beside drugs which are to be given PRN. h) All medical records must be kept on file as specified by Government Legislation. The times for medication administration are highlighted on MAR sheets using the following colour coding: 6:00 am, 6:00 pm…………………orange 8:00 am………………………….…pink 8:00 pm………………………….…blue 12:00 pm/noon……………………green 10:00 pm…………………….……. yellow 4:00 pm…………………………….purple 12:00 am/midnight……………….red REFUSAL OF MEDICATION If an individual refuses medication (beyond 1 hour duration): Contact manager if during business hours. Unless it is critical that the medication be given you will be instructed to squeeze “REF” (for refused) in the box with your initials. After business hours: Discuss with the full-time person at your location. If no full-time staff is available, contact your manager. A decision will be made as to whether or not to contact the pharmacy or a medical professional. If there is any doubt, seek advice as to how to proceed. If necessary, contact pharmacy and/or medical professional and explain situation. If considered life threatening by above, transport individual to medical facility and explain situation. Contact a Manager. Complete an Incident Report within 24 hours and forward to a Manager. 12 MEDICATION CHANGES a) Changes in medication shall only be made with a written or verbal order from a physician. When accompanying an individual to a medical appointment, the Full-time staff (or when absent, designate) will ensure that a Physician’s Order form is completed if any changes are made to the person’s medications. Staff are responsible for assisting the individual to take the order to the pharmacy to be filled. b) In the event that there has been a verbal order from the doctor over the phone staff will complete a physician’s order form indicating the required changes. The form will be faxed to the doctor who will fax it back to MVACL. Staff will then take this to the pharmacy so the MAR sheet can be corrected for the next month. c) All changes must be indicated on the Log Notes under “Health Alerts, New Meds” and on the whiteboard. Medication changes or new medications are also indicated on the Medication Profile and on the MAR sheet, kept in the individual's binder. d) In the event of a change, (e.g. a change in the dose or time) discontinue the previous entry on the MAR sheet and the Profile, and enter as a new medication. e) If drug information does not accompany the medication, consult C.P.S. Manual as to the possible side effects and contraindications of the medication. Drug information should be filed in the binder in the appropriate section. f) Any adverse changes in the individual's physical state or behaviour should be documented and reported to the manager and a physician if necessary. g) An individual's day program (if applicable) should be notified of the change of medication and informed of the possible side effects. h) When an individual who administers medication him/herself has a medication change, the direct support staff must re-evaluate the individual's ability to handle this change, monitor this adjustment as necessary, and supply data to a Manager or designate. INDIVIDUAL’S ILLNESS When an individual vomits after taking a prescribed medication, the staff should attempt to determine how much, if any, of the medication was emitted. With this information, the staff member should then contact the manager or if after hours, a full-time staff or their manager. If deemed necessary, the physician or hospital will be contacted for directions on how to proceed (i.e. whether or not to administer additional medication, signs/symptoms to be observed, etc.). INDIVIDUALS AWAY FROM HOME All medication leaving the residential location shall be in a sealed container. The bubble pack sections will be sent with the individual. Medication instructions must be sent with the individual and/or parent guardian. The parents/guardian should be notified that the individual is on a medication and that he/she has a record of that medication with them. 13 INDEPENDENT INDIVIDUAL MEDICATION ADMINISTRATION a) When an individual is being considered for an independent medication administration program the Support Staff, individual, and physician should be involved in the process of determining whether the individual is capable of doing so. b) Once approved, a program should be implemented based on the individual's ability to safely administer his/her medication. Initially, the individual should only receive a maximum of one week’s supply of the daily quantity of medication. Records will be kept at each stage of the program. The criterion for success requires the individual to administer the correct drug, correct dose, at the correct time, in a safe manner for 30 consecutive days. c) Where individuals live independently and may or may not receive daily support, the choice of how to store meds shall be made with staff input. d) No medications shall be maintained outside of the locked storage area. e) Individuals taking medication should be instructed to inform staff of any changes that they may experience (i.e. diarrhoea, temperature, etc.). This is particularly important when a new medication has been prescribed. f) All medication taken must be documented daily and include date, time, dosage, and medication used. g) An individual may re-order his/her medication when s/he demonstrates ability to: independently administer his/her medication independently re-order communicate (verbally or in written form) the following information to the appropriate pharmacy; individual's name, name of medication, prescription number and physician's name. Direct Support Staff will ensure that medication has been re-ordered before the expiry date each month. EXCEPTIONS TO MEDICATION PROCEDURES In the event that policies/procedures outlined in this paper cannot be followed in their entirety, the support staff must notify a manager in writing of those specific procedures which cannot be complied with. Wherever possible, this notice should be made prior to the change in procedures or on the next working day. 14 MEDICAL ABBREVIATIONS: The following are commonly used medication terms and their meanings: o.d. once a day p.c. after meals q.d. each day gtte. a drop b.i.d. twice a day stat. at once/right away t.i.d. three times a day ml. millilitre (liquid measure) q.i.d. four times a day mg. milligrams h.s. at bedtime cap. capsule a.c. before meals tab. tablet PRN as necessary gtts. drops p.o. by mouth cc cubic centimetre (liquid measure) Ung ointment note: cc and ml are equivalent volumes PRN EXAMPLES: Tylenol, Midol, Ativan Medication which may be purchased over the counter (OTC) or by prescription. These will either be listed on the Dr’s Standing Order or ordered on a prn basis. They are administered as needed; not for a specific duration. SHORT TERM MED EXAMPLES: Antibiotics, Ointments, Cream, Drops Any medication or medical instruction with a very specific duration of administration, e.g. eye cream 2x daily for 5 days or apply dressing 2x daily until healed. MEDICAL TREATMENT EXAMPLE: Hot water bottle, bath with Epsom salts, saline wash, etc. REFERENCES: Lorraine’s Pharmasave 756-2013 C.P.S. Nursing Drug Handbook St. Francis Hospital 756-3044 Poison Control Centre 1-800-267-1373 15 CLASSIFICATIONS OF MEDICATIONS: Analgesics - Analgesics are painkillers and are classified as mild or strong, depending on the pain they relieve. For mild and moderate pain, A.S.A. or Acetaminophen is used. For more severe pain, A.S.A. or Acetaminophen is used in conjunction with Codeine, i.e. - 222's 292's. Note: A.S.A. or Aspirin is also classified as an anti-inflammatory agent which acts on the body not only to reduce pain but also swelling and fever. Excessive use of A.S.A. is known to irritate/damage the stomach lining. Anti-Biotic – Combat only bacterial infections by either destroying bacteria or stopping its growth or both. Note: Antibiotics are often wrongly prescribed for virus infections - cold, flu, undiagnosed fevers - which they cannot combat. Misuse allows resistant bacterial strains to flourish, ultimately resulting in a lack of effective antibiotics. It is imperative that a course of antibiotics be completed even if symptoms disappear. Anti-Convulsants - Various types of drugs that act on the brain to decrease the responsiveness of normal neurons (a nerve cell, the structural and functional unit of the nervous system) to the sudden storms of nervous impulses from a hyperirritable centre in the brain. Most anti-convulsants are effective in controlling only certain types of seizures. Note: Abrupt cessation of many anti-convulsants may precipitate a series of seizures. Discuss this with the individual’s doctor when medication changes are being made. Anti-Depressants - Drugs, which reduce the degree of depression and usually increase psychomotor activity. Anti-Diarrhoeal Drugs - Any medication which acts to stop diarrhoea. Antiemetic – Drug that prevents or reduces nausea and vomiting. Antihistamines – These drugs are used to provide symptomatic relief of allergic symptoms caused by the release of histamines and to treat anaphylactic reactions after acute symptoms have been controlled. They act by: Constricting blood vessels. Relaxing smooth muscles. Inhibiting secretions of mucous glands specifically in the lungs and sinuses. Anti-Manic Agents – Bipolar (manic/depressive) disorders are treated long term with Lithium Salts. Regular blood-work is necessary to maintain therapeutic levels and prevent toxicity. 16 Anti-Pyretic - Medications which reduce an elevated temperature, e.g. Acetylsalicylic Acid (also known as A.S.A or Aspirin) Cardiac Medications - A broad classification, which includes many medications, which aid heart function. They may regulate the heart rate or lower blood pressure but they all assist the heart to function normally. Corticosteroids - Used topically (lotions, creams, sprays) or systemically (by mouth or needle) to treat skin problems associated with allergic reactions. Also used to treat psoriasis and dermatitis. Diuretics - Are medications, which increase the secretion of urine. They are often used to assist in normal heart function. Hypnotic - These drugs dull the senses and induce sleep. Laxatives - drugs that induce defecation classified by how they achieve that goal. Stimulate peristalsis by increasing fluid, gases or solid bulk or intestinal content (e.g. Fleet enema) Wetting agents, lower surface tension and prevent drying of stool (e.g. Colace, Surfak) Bulk forming - coat food and liquid particles, delay absorption, delay drying of fecal content (e.g. Metamucil). Chemical irritation to increase peristalsis (e.g. Senokot). Muscle Relaxants - Drugs used to provide muscular relaxation necessary for various medical and surgical procedures and for relief of muscle pain. Sedatives - Drugs, which exert a soothing, or tranquillizing effect. Tranquilizers – Major: also known as Neuroleptics or Antipsychotics used for relief of symptoms, sedates without inducing sleep and reduces irritability. Minor: also known as Anxiolytics used for SHORT TERM treatment of anxiety disorders. In small doses they can reduce anxiety and promote relaxation without causing sedation. Prolonged use can cause tolerance and dependency. MP Amended Jan. 07 C:\MyDocuments\Medication Policy