Vol IV No 5
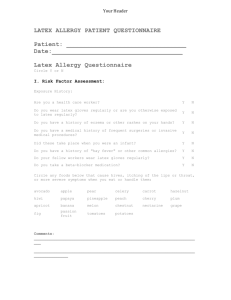
advertisement

-----------------------------------------------------------------------------------------------------------------REPORT OF THE MONTH, Volume IV, Number 5 – September-October 2000 - - - - from the North Carolina Statewide Program for Infection Control and Epidemiology -----------------------------------------------------------------------------------------------------------------CONTENTS: NEWS FEATURES Plant Engineering Must Work Closely with Infection Control Lower Latex Content Linked to Higher Glove Leakage REGULATORY/LEGISLATIVE/QUESTION OF THE MONTH Amended NC State Law Requires Influenza and Pneumococcal Immunization in Long-Term Care Setting QUESTION OF THE MONTH More than One Method Used for Reprocessing Scopes NEWS AND ANNOUNCEMENTS COURSES FOR THE INFECTION CONTROL PROFESSIONAL _____________________________________________________________________ NEWS FEATURES PLANT ENGINEERING MUST WORK CLOSELY WITH INFECTION CONTROL Effective January 1, 2001, the JCAHO revises the Utility Management standard (EC.1.9) to include strategies to minimize the threat of air- and water-borne contaminants such as Aspergillus and Legionella. Presumably, surveyors will ensure that your Utility Management Plan describes how to reduce the potential for organization-acquired illness such as policies to minimize Legionella or Aspergillus in immunocompromised patients. You may already be in compliance with the standard as many facilities work closely with Plant Engineering. If that is the case at your facility, you may just need more documentation (e.g., maintaining air changes, pressure relationships, and filtration efficiencies for ventilation systems serving areas specially designed to control airborne contaminants [e.g., bone marrow, operating rooms, airborne communicable diseases], and managing pathogenic biological agents in cooling towers, domestic hot water, decorative water fountains). LOWER LATEX CONTENT LINKED TO HIGHER GLOVE LEAKAGE With the introduction of Universal Precautions in 1987 and the OSHA Bloodborne Pathogen Standard in 1991, glove use increased from 1 billion pairs per year in the United States in 1987 to 10 billion pairs in 1996 with latex accounting for a large majority of the increase. Between 1988 and 1992 there were more than 1000 reports to the Food and Drug Administration of allergic reactions to latex-containing products that included 15 deaths. Due to concern about the risk of allergic reactions and concern that the increased use of latex gloves could have resulted in increased rates of sensitization, the National Institute for Occupational Safety and Health published an alert in June 1997 recommending the use of nonlatex gloves for activities unlikely to involve contact with infectious materials, the use of powder-free latex gloves with reduced latex protein content if latex gloves were chosen for protection against potentially infectious materials, and of nonlatex gloves for patients or health care workers with latex allergy. Researchers at the University of Virginia showed that leakage rates were greater for examination than for surgical gloves, for manipulated than for unused gloves, and for low latex content surgical gloves or nonlatex content surgical gloves than for high latex content surgical gloves. While high latex gloves were associated with significantly lower leakage rates than the low latex and nonlatex brands tested, some nonlatex and low latex gloves were very resistant to leakage and should provide an effective barrier for preventing exposure to bloodborne pathogens. (Muto CA et al. Arch Surg 2000;135:982-985) REGULATORY/LEGISLATIVE AMENDED NC STATE LAW REQUIRES INFLUENZA AND PNEUMOCOCCAL IMMUNIZATION IN LONG-TERM CARE SETTING Amended NC General Statute 131D.9 requires that adult care homes and nursing homes (facilities) ensure that residents and employees are immunized against influenza virus and that residents are also immunized against pneumococcal disease. Effective September 1, 2000 long-term care facilities must screen new admission for documentation of pneumococcal immunization and notify the resident of the immunization requirements of this law. Long-term care facilities are to request that the resident agree to be immunized. Immunization and documentation of pneumococcal vaccination by long-term care facilities shall occur no later than November 30 of each year. The law further states that effective September 1, 2001 employees and residents of long-term care facilities shall be requested to receive the influenza vaccine on an annual basis no later than November 30 of each year. Long-term care facilities must document immunization status. According to the law, "No individual shall be required to receive vaccine under this section if the vaccine is medically contraindicated, or if the vaccine is against the individual's religious beliefs, or if the individual refuses the vaccine after being fully informed of the health risks of not being immunized." QUESTION OF THE MONTH MORE THAN ONE METHOD USED FOR REPROCESSING SCOPES Q: In my hospital bronchoscopy suite scopes are reprocessed by soaking in 2% glutaraldehyde between cases but at the end of the day they are ETO gas sterilized. In another area of the hospital for outpatient procedures the bronchoscopes are reprocessed in an automated washer/sterilizer. Is it a problem to use the different reprocessing techniques? A: In the "APIC Guideline for Selection and Use of Disinfectants," by WA Rutala and the APIC Guidelines Committee (1996) this practice is discussed as follows. Semicritical equipment (e.g., endoscopes) should be high-level disinfected between patients. However, some institutions choose to sterilize semicritical equipment when used on certain infectious patients or as part of a routine process at the beginning or the end of each day. This may lead to a "double standard" of patient care and is inconsistent with the principle of universal precautions when equipment used on patients with known specific infectious diseases (e.g., tuberculosis, HIV infection) is sterilized, but the same equipment is only high-level disinfected for other patients. Under these circumstances, sterilization should not be performed in the belief that it is providing a greater margin of safety. In contrast, it is not a double standard of patient-care to sterilize endoscopes in one hospital area (e.g., operating room) and high-level disinfect in another area (e.g., gastroenterology clinic) because the outcome is equivalent from an infectious disease transmission perspective. NEWS AND ANNOUNCEMENTS In a letter dated October 18, 2000, Abbott Diagnostics informed their customers that the Abbott/Murex Single Use Diagnostic System (SUDS) HIV test will not be available for an undetermined period of time due to manufacturing problems. The Federal Drug Administration (FDA) suggests several possible interim measures. For more information, see the FDA web site http://www.fda.gov/cber/infosheets/abbsuds101800.htm COURSES FOR THE INFECTION CONTROL PROFESSIONAL "Infection Control Part I: Clinical Surveillance of Nosocomial Infections will be held in Chapel Hill in the spring of 2001. "Infection Control in Long-Term Care" will be held in Chapel Hill in the spring of 2001. -----------------------------------------------------------------------------------------------------------------Contributors to Report of the Month: Karen K. Hoffmann, RN, MS, CIC; William A. Rutala, PhD, MPH, David J. Weber, MD, MPH, Eva P. Clontz, MEd. ------------------------------------------------------------------------------------------------------------------ To subscribe to the Report of the Month, send email to spice@unc.edu Report of the Month is also available on the home page of the Statewide Program for Infection Control and Epidemiology at http://www.unc.edu/depts/spice/ The Statewide Program for Infection Control and Epidemiology (SPICE) is funded by the General Assembly of North Carolina to serve the State. SPICE is not a regulatory agency but provides education and consultation to North Carolina healthcare facilities. Copyright 2000 Statewide Program for Infection Control and Epidemiology