DNACPR Orders in the Primary Care Setting
DNACPR Orders in the Primary Care Setting
Guidance notes to accompany the All-Wales DNACPR form.
November 2009
DNACPR Orders in the Primary Care Setting
Scope of Document
This document deals with DNACPR (do not attempt cardio-pulmonary resuscitation) orders for adults over 18 years old in the primary care setting.
DNACPR refers to cardio-pulmonary resuscitation only. A valid DNACPR order does not preclude other active interventions or care.
The term “primary care setting” is used to include the patient’s home, another’s home, nursing home and other out-of-hospital settings.
Purpose
DNACPR orders are an important mechanism to avoid inappropriate CPR attempts, when those attempts would be:
futile - and/or
against the expressed wishes of the patient - and/or
not in the best interests of a patient
Relevant legislation and guidance
The document takes account of relevant legislation and guidance, especially:
1) The Mental Capacity Act, 2005
2) Decisions relating to Cardiopulmonary Resuscitation; A Joint Statement from the British Medical Association, the Resuscitation Council (UK), and the
Royal College of Nursing. Updated version November 2007
3) End of life treatment and care: Good practice in decision-making. Draft
Guidance, GMC; April 2009.
4) Recommended Resuscitation Form and Guidance; UK Resuscitation Council,
March 2009
Writing a DNACPR order
Box 1. Care of the Dying/Last Days of Life Care Pathway
A DNACPR order should be made whenever a patient is started on the Last
Days of Life care pathway.
Discussion of CPR is not necessary if the family are aware of imminent death.
Patients who are cared for using the Care of the Dying/Last Days of Life Care
Pathway have, by definition, been recognized to be imminently dying from an irreversible illness. As such, CPR can never be medically appropriate when such patients die.
Although staff should discuss the impending natural death with family or carers, a specific discussion about CPR is often irrelevant and inappropriate.
Nevertheless, a DNACPR order is important because family or carers will occasionally call the emergency services, often due to panic.
The care pathway documentation for community setting will include a DNACPR form.
DNACPR orders in the Primary Care setting November 2009
Box 2. "Best-interests" DNACPR orders
A DNACPR order may be appropriate at home in circumstances when a patient lacks mental capacity to make his/her own decision:
Examples
Advanced end stage cardiovascular disease - identified as “likely to be in last
6 months of life” (i.e. GSF criteria) - where there is a significant chance of a
cardio-pulmonary arrest occurring.
Advanced end stage disease - metastatic cancer, COPD, dementia, ESRD - identified as “likely to be in last 6 months of life”
(i.e. GSF criteria) - but no particular risk
of cardio-pulmonary arrest.
Patient without mental capacity
The issue of CPR should be sensitively explored (proactively) with the next-of-kin.
Discussion with the next-of-kin 1 is usually necessary before a DNACPR order is made.
DNACPR orders will normally only follow a conversation led by the family / carer.
2
Discussion with the next-of-kin is usually necessary before a DNACPR order is made.
Box 3. DNACPR order as an Advance decision by the patient
A DNACPR form may be used to record the expressed wishes of a patient with mental capacity to decline CPR.
If a patient has made a valid advance decision to refuse treatment, this is a legally binding document. However, use of the standard DNACPR form with its familiar layout, will help healthcare professionals to act appropriately in an emergency situation.
Who should complete the Form?
The responsibility for making a DNACPR decision rests with the most senior clinician currently in charge of the patient’s care. Wherever possible, a decision should be agreed with the whole healthcare team. The most senior clinician could be a consultant, GP or suitably experienced nurse.
Mental Capacity Act 2005
It is the duty of the senior healthcare professional who signs a DNACPR order made in the 'best interests' of a patient who lacks mental capacity, to ensure that the order complies with all aspects of the Mental Capacity Act 2005. In particular, the following should be considered:
Is the patient unable to make a decision, due to impairment or disturbance of mind or brain?
make all possible attempts to exclude communication barriers e.g hearing aids, speech therapists, translators
Consider whether, and if so when, the patient might have capacity for the decision in the future
As far as is practicable, permit and encourage the patient to participate in the decision
1 The next-of-kin is usually the person who should be consulted; consultation should include, when appropriate, a person with a Lasting Power of Attorney, a Court Appointed Deputy, or if there is no family, an IMCA. cf. Mental Capacity Act 2005
2 With increasing interest in Advance Care Planning, DNACPRs may more commonly follow conversations which explore of end-of-life issues with patients or families
DNACPR orders in the Primary Care setting November 2009
If a decision relates to life-sustaining treatment , the professional must not be motivated by a desire to bring about the patient's death
Take into account, as far as is reasonable, all the relevant circumstances:
patient's past - and present- feelings and wishes
beliefs and values likely to influence the patient's wishes if he/she had capacity, and any other factors
any other relevant written statement
Take account, if practicable, of views as to what would be in the patient's best interests - family, friends, carers
In particular, the following may be legally binding:
Advance Decisions
Lasting Power of Attorney (LPA)
Court Appointed Deputy (CAD)
If no family, friends, CAD, or LPA are available - consider the appointment of an
Independent Medical Capacity Advocate (IMCA)
DNACPR Order Form
A distinctive orange-bordered form has been developed for use across the whole of
Wales. The form needs to be instantly recognisable because of the emergency circumstances in which it is required. Therefore only one form should be used across
Wales (no variants), and it should always be reproduced in colour.
Awareness
Paramedic crews, accident & emergency department staff, and all social and health care staff working in the community should be:
aware of the All-Wales DNACPR form
able to identify rapidly if an order has been completed correctly
aware of their responsibility to respect a DNACPR order
aware of occasions when they may/should disregard an order
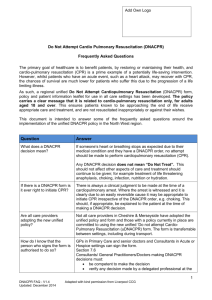
Correct completion of a DNACPR Form
The patient's name, date of birth and address must be clearly legible (block capitals are recommended)
One of the three boxes must be ticked:
Option 1 (Last Days of Life Care Pathway) - 1 of the 2 options must be ticked
Option 2 (Best-interests decision for a patient who lacks capacity) - All of the additional boxes must be ticked
Option 3 (Patient's express wishes) - 1 of the 2 options must be ticked
In order to aid rapid assessment of the form's validity, options are indicated by circles, and essential checklists are indicated by squares (similar to the radio buttons and checkboxes on computer forms which many people will be familiar with).
3
If any box is ticked stating that discussions with the next-of-kin, LPA, CAD or IMCA have taken place, their name and contact details should be recorded.
3
Square boxes must always be ticked
Circles are options where only one of the group need be ticked
DNACPR orders in the Primary Care setting November 2009
The form should be signed by the senior healthcare professional - every box must be completed: signature, full name (printed), address (e.g. GP practice/surgery, or organisation), telephone number, date and time.
Responsibility to respect an order
Healthcare professionals should respect a DNACPR that is correctly completed . It is not their responsibility to confirm the details on the form, signatures etc. (other than the identity of the patient).
Occasions when discretion should be used
Staff should be aware of possible situations when they may need to act according to their own professional judgement, for example:
any concerns about the identity of the patient
any other doubts about the validity of the form
a relative is present who is challenging the validity of the order
Although a relative does not have a legal right to overturn a decision made by a patient with capacity or an LPA or IMCA, in an emergency situation it may not be possible to ascertain the validity of the information on the form, and a decision to start
CPR may be the only appropriate course of action.
Where to keep a DNACPR Order
For patients on the Last Days of Life Care Pathway, a DNACPR form will be included in the Care Pathway documentation, and should be kept with the Care
Pathway.
At home, the form should be kept with the district nursing records where appropriate.
In nursing and residential homes, the form should be kept with the patient's health care records.
Patients who have made an advance decision (Box 3) but who do not have healthcare records in the house, should be advised to consider:
using a bottle in the fridge (Message in a Bottle scheme - Rotary Club and
Lions' Club)
obtaining a bracelet (MedicAlert etc.)
Alerting others of a DNACPR Order
Other key healthcare professionals should be informed of the presence of (and any changes to) a DNACPR form:
GP (if not signed the form)
District nursing team
Social services care manager
Specialist palliative care team
Limitations of Scope
DNACPR decisions for children, including those between 16 and 18 years old are not covered by the All-Wales form or this document.
DNACPR orders in the Primary Care setting November 2009
Appendix 1
Members of the Working Group:
Dr Ian Back (Chair, Palliative care consultant, Cwm Taf NHS Trust)
Dr Rhys Davies (GP Macmillan facilitator, North Wales)
Anne-Louise Ferguson (Managing Solicitor, Welsh Health Legal Services)
Professor Ilora Finlay (Professor of Palliative Medicine, Chair of Palliative
Care Implementation Board)
Dr Andrew Fowell (Palliative care consultant, Ysbyty Glan Clwyd)
Dr Matthew Makin (Palliative care consultant, Nightingale House, Wrexham)
Jessica Gwynne (Trainee Solicitor, Welsh Health Legal Services)
Dr Fiona Rawlinson (Palliative care consultant, Bridgend)
Mr Andrew Williams (Advanced Paramedic Practitioner / Care Pathways
Project Lead, Welsh Ambulance NHS Trust)
Mr Grant Williams (Unscheduled care manager, Welsh Ambulance NHS
Trust)
DNACPR orders in the Primary Care setting November 2009